
The Neuro-Navigation System is often described by neurosurgeons as a “GPS for the brain.” It is a sophisticated computer-assisted technology that guides surgeons during delicate procedures within the skull and vertebral column. Just as a satellite navigation system tracks a car’s exact location on a digital map, this technology tracks the surgeon’s instruments in real-time on a 3D model of the patient’s own anatomy.
The primary problem this technology solves is the “black box” nature of neurosurgery. Once a surgeon makes an incision, their view is limited to the immediate surface tissue. Critical structures such as deep-seated tumors, major blood vessels, or vital nerve pathways are often hidden underneath healthy brain tissue or bone. Historically, surgeons relied on anatomical knowledge and mental visualization to estimate where these structures were located, which carried a margin of error. Neuro-navigation eliminates this guesswork. It provides a live, interactive roadmap, allowing the surgeon to “see through” the skull and skin before making a cut, ensuring that the surgical path is perfectly calculated to reach the target while avoiding “no-fly zones” of healthy, functional tissue.
How the Neuro-Navigation System Works?
The functionality of neuro-navigation relies on the precise synchronization of three components: diagnostic imaging, the patient’s physical anatomy, and the surgical instruments. This process, known as “registration,” bridges the virtual world with the physical world.
Step 1: Image Acquisition (The Map)
The process begins days before the surgery. The patient undergoes a high-resolution MRI or CT scan.
- Fiducial Markers: In many cases, small adhesive stickers (fiducials) are placed on the patient’s scalp or forehead during the scan. These act as fixed landmarks, similar to lighthouses on a nautical map.
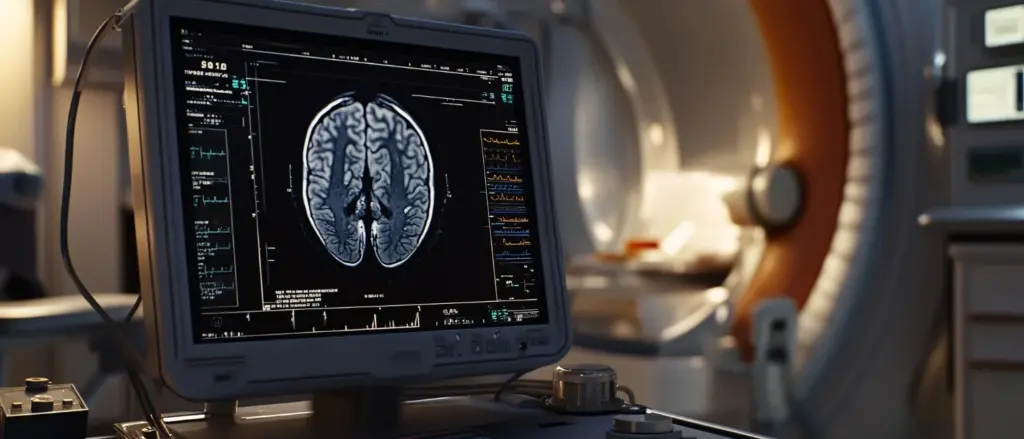
- 3D Rendering: The scan data is loaded into the neuro-navigation workstation. Advanced software processes these hundreds of 2D slices and constructs a highly detailed, rotatable 3D model of the patient’s brain, skull, and spine.
Step 2: Patient Registration (The Sync)
In the operating room, once the patient is asleep and positioned on the table, the “registration” phase begins. This creates a mathematical link between the 3D map on the screen and the patient’s actual head.
- Point Matching: The surgeon uses a specialized probe to touch the fiducial markers or specific anatomical landmarks (like the bridge of the nose) on the patient.
- Triangulation: The computer system recognizes these points and aligns the pre-operative 3D MRI with the physical position of the patient’s head on the operating table. Once registered, touching any point on the patient’s scalp immediately shows that exact point on the monitor’s MRI.
Step 3: Real-Time Tracking (The Drive)
During the surgery, the system tracks the instruments.
- Optical Tracking: Most modern systems use an infrared camera array positioned above the operating table. The surgical instruments (probes, suction tubes, forceps) are fitted with reflective spheres.
- Live Feedback: As the surgeon moves the instrument, the camera tracks the spheres. The computer calculates the instrument’s position and tip angle in millisecond intervals. On the screen, the surgeon sees a virtual crosshair moving through the brain slices, showing exactly where their instrument is located, how deep it is, and what lies millimeters ahead.
Clinical Advantages and Patient Benefits
The integration of neuro-navigation has fundamentally shifted the risk profile of neurosurgery, allowing for “minimally invasive” approaches in areas previously considered too dangerous to operate on.
Maximizing Tumor Resection
The goal of cancer surgery is to remove as much of the tumor as possible (maximal resection) without causing new neurological deficits.
- Defining Margins: Brain tumors often look similar to healthy brain tissue. Navigation allows the surgeon to outline the tumor boundaries on the screen. During surgery, they can verify if they have reached the edge of the tumor or if residual cancer cells remain hidden around a corner, leading to more complete removal and better survival rates.
Smaller Craniotomies (Bone Openings)
Without navigation, surgeons historically made larger openings in the skull to ensure they didn’t miss the pathology.
- Keyhole Approach: With pinpoint accuracy, the surgeon can plan the incision to be directly over the tumor. This allows for a “keyhole” craniotomy a bone opening often no larger than a coin.
- Reduced Trauma: Smaller openings mean less disruption to the scalp muscle, less blood loss, and significantly less post-operative pain.
Trajectory Safety
In deep brain biopsies or ventricle catheter placements, the instrument must pass through healthy brain to reach the target.
- Avoiding Eloquent Areas: The software calculates the safest trajectory, angling the path to avoid “eloquent” areas (regions controlling speech or movement) and major blood vessels. This drastically reduces the risk of stroke or paralysis caused by the surgical approach itself.
Targeted Medical Fields and Applications
While “neuro” implies the brain, this technology is a workhorse across several surgical disciplines involving complex bony or soft tissue anatomy.
Neurosurgery (Cranial)
- Brain Tumors: Used for gliomas, meningiomas, and metastases. It is critical for locating deep-seated tumors that are not visible on the brain surface.
- Epilepsy Surgery: It guides the resection of focal cortical dysplasia tiny, subtle malformations in the brain architecture that cause seizures.
- Vascular Surgery: Used to locate small cavernomas or AVMs (Arteriovenous Malformations) that are buried deep within the brain tissue.
- Biopsies: Allows for the needle biopsy of undefined lesions with millimeter precision, ensuring a diagnostic sample is obtained on the first pass.
Spinal Surgery (Orthopedic and Neuro)
- Pedicle Screw Placement: In spinal fusion surgery, metal screws are inserted into the narrow bony bridges (pedicles) of the vertebrae. Navigation allows the surgeon to see the screw entering the bone in real-time, ensuring it does not breach the wall and hit the spinal cord or nerve roots.
- Deformity Correction: In scoliosis or complex spinal reconstruction, anatomy is often twisted and unrecognizable. Navigation provides a reliable reference to true anatomy, reducing the risk of catastrophic nerve injury.
ENT (Otorhinolaryngology)
- Sinus Surgery: Functional Endoscopic Sinus Surgery (FESS) uses navigation to operate near the skull base and eye orbits. It helps the surgeon remove polyps and open sinuses without accidentally penetrating the thin bone separating the nose from the brain or the eye.
What to Expect: The Neuro-Navigation System Procedure
For the patient, the use of neuro-navigation adds layers of safety without adding significant time or discomfort to the experience.
Pre-Operative Mapping
The experience begins a day or two before surgery (or the morning of).
- Fiducial Placement: If skin markers are used, a technician will stick small, donut-shaped markers on the patient’s scalp. Patients are instructed not to pick at or wash these off, as they are essential for the system’s accuracy.
- The Scan: The patient undergoes a standard MRI or CT scan. This is painless and non-invasive. The scan may take slightly longer than a diagnostic scan (about 20-30 minutes) to acquire the ultra-thin slices needed for the 3D model.
In the Operating Room
- Positioning: Once the patient is under general anesthesia, their head is gently secured in a specialized clamp (Mayfield skull clamp). This prevents even microscopic movements during the surgery, which is vital for navigation accuracy.
- Registration: The surgeon performs the registration process while the patient is asleep.
- The Procedure: The surgery proceeds. The patient is unaware of the infrared cameras or the digital screens.
Post-Operative
- Marker Removal: The sticky markers are removed from the skin immediately after surgery.
- Recovery: Because the incisions are smaller and the brain manipulation is minimized, patients often experience less swelling and a faster return to alertness compared to non-navigated procedures.
Safety and Precision Standards
Neuro-navigation is a tool of high precision, but it is supported by rigorous verification protocols to account for the dynamic nature of the human body.
Brain Shift Compensation
One of the challenges in neurosurgery is “Brain Shift.” When the skull is opened and cerebrospinal fluid is drained, the brain can sag or shift slightly, meaning the pre-operative MRI map is no longer perfectly accurate.
- Intraoperative Updates: To counter this, advanced navigation systems can be paired with intraoperative ultrasound or intraoperative MRI. The surgeon scans the brain during the surgery, and the system updates the 3D model to reflect the new position of the brain tissue. This ensures the “GPS” remains accurate from start to finish.
Accuracy Verification Checks
Before making the incision, the surgeon performs a “checkpoint verification.”
- Anatomical Audit: The surgeon touches a known landmark such as the outer corner of the eye or the tragus of the ear with the probe. They verify that the crosshair on the screen lands on that exact pixel. If the discrepancy is more than 1-2 millimeters, the system is re-registered or recalibrated.
Instrument Calibration
Every instrument used with the system involves a specific calibration file. Before using a suction tube or a drill, the surgeon validates the tool with the system. This ensures the computer knows the exact length and diameter of the tool, preventing the “virtual tip” from being displayed deeper or shallower than the actual tip is in the brain. This rigorous digital hygiene prevents over-shooting targets and protects vital structures.











