Last Updated on November 26, 2025 by Bilal Hasdemir
At Liv Hospital, we tackle the tough cases of adrenocortical carcinoma. This rare cancer starts in the adrenal cortex. We use the latest medical tech and focus on our patients to treat it.
We know how to handle adrenal tumors at each stage. Our goal is to give top-notch care to patients from around the world.
Key Takeaways
- Understanding adrenocortical carcinoma is key to treating it well.
- Adrenal tumors can be either benign or cancerous, needing different treatments.
- Knowing the stage and spread of the tumor helps plan the best treatment.
- Liv Hospital is all about caring for patients with complex conditions.
- We offer advanced treatments for adrenocortical carcinoma.
Understanding Adrenocortical Neoplasms
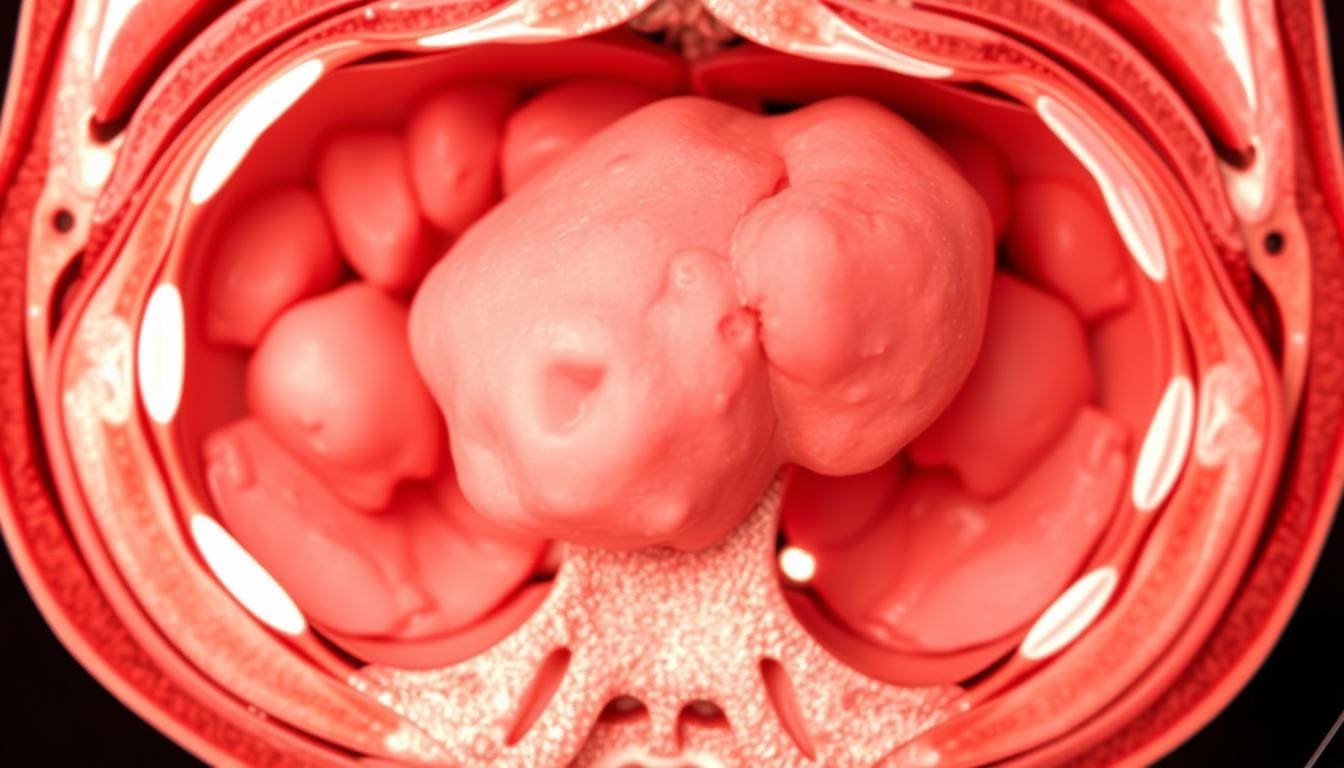
Adrenocortical neoplasms are tumors that grow in the adrenal cortex. This is the outer layer of the adrenal gland. They can be non-cancerous or cancerous, with the cancerous type being rare but dangerous. These tumors can greatly affect hormone production, causing various symptoms.
Definition and Prevalence
These tumors start in the adrenal cortex. They can be benign or malignant, with the cancerous type being rare but dangerous. The number of people with these tumors is small, but their impact can be big. This is because they can cause hormonal imbalances and other problems.
Some important facts about adrenocortical neoplasms include:
- Variety of presentations: These tumors can be hormone-producing or not.
- Rarity: Adrenocortical carcinoma, a cancerous form, is rare, affecting about 1-2 people per million each year.
- Detection challenges: Finding these tumors often requires imaging and biochemical tests.
Adrenal Gland Anatomy and Function
The adrenal glands sit on top of each kidney. They are key in making hormones that control many body functions. These include stress response, blood pressure, and electrolyte balance. The adrenal cortex makes corticosteroids, like cortisol and aldosterone, which help keep the body balanced.
Knowing how the adrenal gland works is key. It helps us see how tumors can upset hormone balance and health.
Tumor Adrenocortical: Benign vs. Malignant Forms
Adrenocortical tumors can be benign or malignant. Knowing the difference is key for treatment and outlook.
Adrenocortical Adenomas
Adrenocortical adenomas are benign tumors from the adrenal cortex. They are common and often found by chance. Most don’t make too much hormone, but some can cause hormonal issues.
Characteristics of Adrenocortical Adenomas:
- Typically small in size
- Often non-functioning
- Rarely malignant
- Usually unilateral
Adrenocortical Carcinoma (ACC)
Adrenocortical carcinoma (ACC) is a rare and aggressive cancer from the adrenal cortex. It can happen at any age but is more common in young children and adults in their 40s and 50s. ACC can make too much hormone or not at all.
Characteristics of Adrenocortical Carcinoma:
- Often large at diagnosis
- Can be functioning or non-functioning
- High risk of spreading
- Poor outlook if caught late
Risk Factors and Genetic Predisposition
There are risk factors and genetic links for adrenocortical tumors. Knowing these can help catch them early.
| Risk Factor | Description |
|---|---|
| Genetic Syndromes | Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, and others can increase the risk of developing ACC. |
| Family History | A family history of adrenocortical tumors or other cancers can be a risk factor. |
| Previous Radiation Exposure | Exposure to radiation, specially in childhood, may increase the risk of developing ACC. |
Understanding the differences between benign and malignant adrenocortical tumors helps us diagnose and treat better.
Key Fact 1: Clinical Presentation and Symptoms
It’s important to know how adrenocortical tumors show up early. They can appear in different ways, depending on what hormones they make.
Functioning vs. Non-functioning Tumors
Adrenocortical tumors are either functioning or non-functioning. Functioning tumors make too much hormone, causing specific symptoms. On the other hand, non-functioning tumors don’t make hormones and might not show symptoms at all.
Hormonal Manifestations and Adrenocorticosteroid Production
Functioning tumors can make hormones like cortisol, aldosterone, and androgens. Too much of these can cause problems like Cushing’s syndrome or virilization. The symptoms depend on the hormone and how much is made.
Non-specific Symptoms and Incidental Discovery
Non-functioning tumors might cause vague symptoms like belly pain. Often, they’re found by accident during tests for other issues. This makes it hard to diagnose them, so doctors need to be careful.
Key Fact 2: Diagnostic Approaches and Workup
To diagnose adrenocortical tumors, doctors use many methods. This includes imaging and biochemical tests. We will look at how these methods help identify these tumors.
Imaging Techniques and Findings
Imaging is key in finding adrenocortical tumors. CT scans and MRI are often used. They help see the tumor’s size, location, and type.
CT scans are great for spotting big tumors and checking if they might be cancerous. MRI gives detailed pictures. It helps tell if a tumor is benign or malignant.
Biochemical Testing and Hormone Evaluation
Biochemical tests are vital for adrenocortical tumors. They check hormone levels to see if the tumor is making too much hormone.
For tumors that make hormones, we test for cortisol, aldosterone, and androgens. High levels can show what kind of hormone problem there is. This helps decide how to treat it.
| Hormone | Associated Condition | Typical Symptoms |
|---|---|---|
| Cortisol | Cushing’s Syndrome | Weight gain, hypertension, hyperglycemia |
| Aldosterone | Conn’s Syndrome | Hypertension, hypokalemia |
| Androgens | Virilization | Masculinization, hirsutism |
Biopsy Considerations and Limitations
Biopsy is not usually the first choice for adrenocortical tumors. It can spread the tumor and it’s hard to tell if it’s cancerous from a biopsy.
But, sometimes a biopsy is needed when tests are unclear. It’s important to talk about the risks and benefits with the patient.
We use a mix of imaging and biochemical tests to accurately diagnose and treat adrenocortical tumors.
Key Fact 3: Staging System for Adrenocortical Carcinoma
Understanding the staging system for adrenocortical carcinoma is key. It helps us see how far the disease has spread. This information guides treatment plans.
The staging system helps us sort adrenocortical carcinoma into different stages. Each stage has its own features and treatment needs. Accurate staging is important for predicting how well a patient will do.
Stage I: Localized Disease (≤5 cm)
Stage I adrenocortical carcinoma is a small tumor, 5 cm or less. It’s usually found only in the adrenal gland. There’s no sign of spread to other areas. Surgery is often the main treatment, and the outlook is good.
Stage II: Locally Advanced (>5 cm)
Stage II has a tumor bigger than 5 cm. It might be in the adrenal gland or nearby tissues. Surgery is harder because of the size and location. Treatment may include surgery, chemotherapy, and radiation.
Stage III: Regional Spread and Lymph Node Involvement
Stage III means the tumor has reached nearby lymph nodes or organs. This stage is more serious. Treatment may include surgery, chemotherapy, and radiation. Surgery is harder because of the lymph nodes.
Stage IV: Distant Metastasis
Stage IV shows the cancer has spread to distant places like the lungs or liver. This is a serious case. Treatment aims to ease symptoms and improve life quality. Chemotherapy and targeted therapy are common treatments.
A leading oncologist says, “The staging system is vital for us. It helps us tailor treatments to each patient’s needs.” This shows how important accurate staging is in treating adrenocortical carcinoma.
Tumor Adrenocortical Carcinoma: Metastasis
Understanding how adrenocortical carcinoma spreads is key to managing it well. This aggressive cancer’s spread is a big factor in how it progresses and affects patients.
Common Sites: Lungs, Livers, and Bones
Adrenocortical carcinoma often spreads to the lungs, liver, and bones. The lungs are at high risk because of their blood supply. The liver, involved in metabolism, is also a common site. Bone metastases, though less common, can greatly affect a patient’s quality of life.
| Metastatic Site | Frequency | Clinical Implications |
|---|---|---|
| Lungs | High | Respiratory symptoms, possible pneumothorax |
| Liver | Moderate to High | Hepatic dysfunction, risk of liver failure |
| Bones | Moderate | Pain, risk of fractures, high calcium levels |
Detection Methods for Metastatic Disease
Spotting metastatic disease in adrenocortical carcinoma requires imaging and blood tests. We use CT scans, MRI, and PET scans to find metastases in different organs. Blood tests, like hormone level checks, help track the disease’s progress and treatment response.
Imaging Techniques: CT scans are great for finding lung and liver metastases. MRI is better for soft tissue and bone metastases. PET scans show metabolic activity, helping find active disease sites.
Clinical Implications of Different Metastatic Patterns
The spread of cancer affects treatment and outcomes. Patients with few metastases might do well with local treatments like surgery or radiation. Those with many metastases might need systemic treatments, like chemotherapy or targeted therapy.
When planning treatment, we must look at each patient’s spread pattern. This can change survival chances and quality of life.
Key Fact 5: Histopathologic Classification and Grading
Understanding the histopathologic characteristics of adrenocortical neoplasms is key for accurate diagnosis and effective management. The histopathologic classification and grading of these tumors help in determining the prognosis and guiding treatment decisions.
WHO Classification System for Adrenocortical Tumors
The World Health Organization (WHO) classification system provides a framework for categorizing adrenocortical tumors based on their histopathologic features. This system helps in distinguishing between benign adrenocortical adenomas and malignant adrenocortical carcinomas. According to a study published in Springer Link, the WHO classification system is widely used for its clarity and reliability in diagnosing adrenocortical tumors.
Weiss Criteria and Ki-67 Index for Malignancy Assessment
The Weiss criteria are a set of histopathologic parameters used to assess the malignancy of adrenocortical tumors. These criteria include features such as nuclear atypia, mitotic rate, and capsular invasion. A high Ki-67 index, which is a marker of cell proliferation, is often associated with more aggressive tumor behavior and a higher likelihood of malignancy.
Molecular and Genetic Markers
In addition to traditional histopathologic evaluation, molecular and genetic markers are increasingly being used to assess the malignancy of adrenocortical tumors. These markers can provide valuable information on tumor biology and help in identifying targets for therapy. The integration of molecular and genetic analysis into the diagnostic workup can enhance the accuracy of adrenocortical carcinoma diagnosis and inform personalized treatment strategies.
By combining the WHO classification system, Weiss criteria, Ki-67 index, and molecular and genetic markers, clinicians can obtain a complete understanding of the tumor’s characteristics. This information is vital for developing an effective treatment plan and improving patient outcomes.
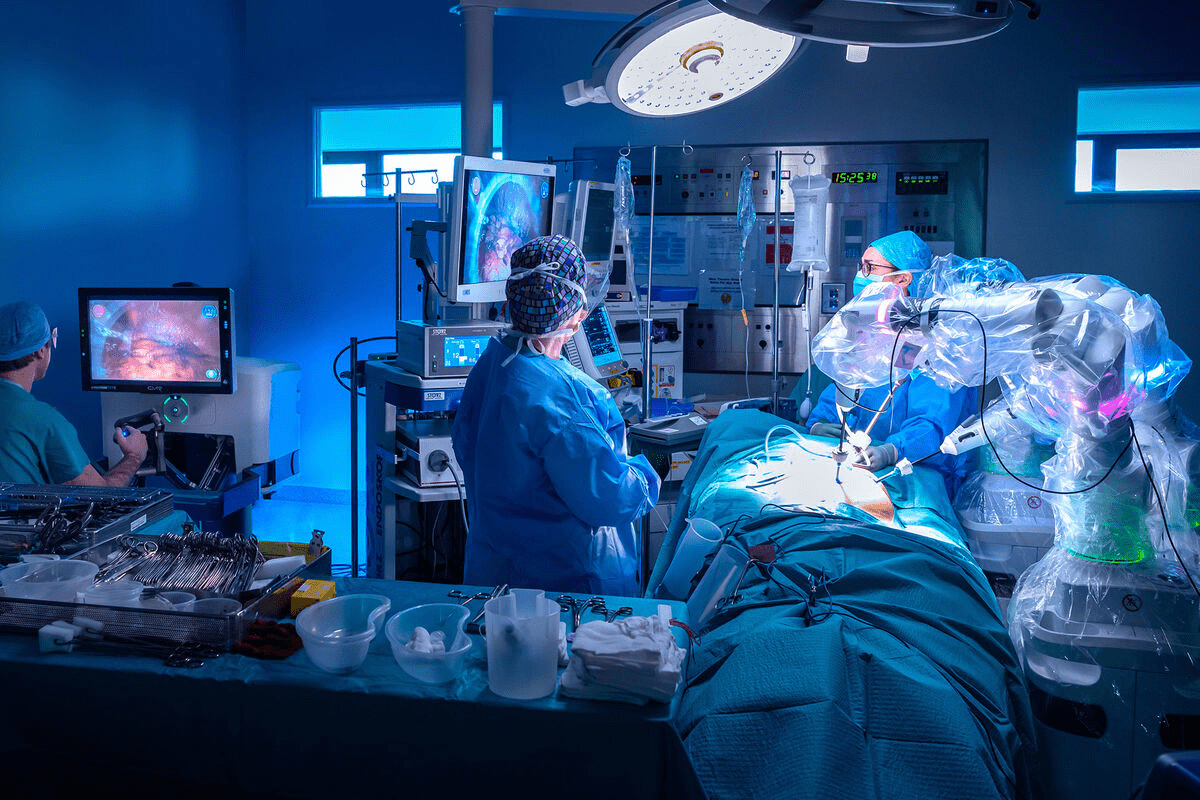
Key Fact 6: Surgical Management Strategies
Surgery plays a key role in treating adrenocortical carcinoma. We will look at different surgical methods used for these tumors.
Open vs. Laparoscopic Adrenalectomy
The choice between open and laparoscopic adrenalectomy depends on several factors. These include tumor size, suspicion of malignancy, and the patient’s health. Laparoscopic adrenalectomy is best for small, benign tumors. It’s less invasive, leading to less pain and faster recovery.
Open adrenalectomy is often chosen for larger tumors or those thought to be malignant. It offers better control over cancer.
Surgical Approaches for Metastatic Disease
For metastatic adrenocortical carcinoma, surgery might be an option. We assess the extent of metastasis and the patient’s condition. Metastasectomy can be beneficial for those with limited metastasis. It may improve survival and quality of life.
Post-surgical Monitoring Protocols
After surgery, close monitoring is vital to catch any recurrence or metastasis early. This includes regular imaging, biochemical tests, and clinical evaluations. The monitoring plan is based on the patient’s risk factors and disease specifics.
| Surgical Approach | Indications | Benefits |
|---|---|---|
| Laparoscopic Adrenalectomy | Small, benign tumors | Less postoperative pain, quicker recovery |
| Open Adrenalectomy | Larger or malignant tumors | Better oncological control |
| Metastasectomy | Limited metastatic disease | Potential improvement in survival and quality of life |
We know each patient is different. Our team works with patients to create a treatment plan that meets their unique needs.
Key Fact 7: Medical Therapy Options
We explore the medical therapy options that are changing the treatment paradigm for adrenocortical carcinoma. Medical therapy plays a vital role in managing this condition, specially in advanced stages.
Mitotane: Mechanism and Administration
Mitotane is a cornerstone in the treatment of adrenocortical carcinoma. It works by inhibiting steroidogenesis and has a direct cytotoxic effect on adrenocortical cells. The administration of mitotane requires careful monitoring due to its narrow therapeutic index and possible side effects.
Chemotherapy Regimens for Advanced Disease
Chemotherapy is considered for patients with advanced adrenocortical carcinoma. Common regimens include combinations of etoposide, doxorubicin, and cisplatin, often used alongside mitotane. The choice of chemotherapy depends on various factors, including the patient’s overall health and previous treatments.
Emerging Targeted Therapies and Immunotherapy
Research into targeted therapies and immunotherapy is ongoing, giving new hope for patients with adrenocortical carcinoma. Targeted therapies aim to exploit specific molecular vulnerabilities in cancer cells, while immunotherapy seeks to enhance the body’s immune response against the tumor.
Management of Hormonal Excess
Managing hormonal excess is key in adrenocortical carcinoma, as it can lead to significant morbidity. Medications that inhibit steroid synthesis, such as ketoconazole and metyrapone, are used to control hormonal imbalances. In some cases, surgical intervention may be necessary to reduce tumor burden and alleviate symptoms.
| Treatment Option | Mechanism | Use in Adrenocortical Carcinoma |
|---|---|---|
| Mitotane | Inhibits steroidogenesis, cytotoxic to adrenocortical cells | Primary treatment for adrenocortical carcinoma |
| Chemotherapy (e.g., EDP) | Cytotoxic, targets rapidly dividing cells | Used in advanced disease, often with mitotane |
| Targeted Therapies | Targets specific molecular vulnerabilities | Emerging treatment, under investigation |
| Immunotherapy | Enhances immune response against tumor | Under investigation, possible future treatment |
We continue to advance our understanding and treatment of adrenocortical carcinoma, giving patients more options and hope for better outcomes.
Multidisciplinary Approach to Patient Care
Adrenocortical carcinoma is complex and needs a team effort. We think a team approach is key to caring for patients fully.
Role of Endocrinologists, Surgeons, and Oncologists
Healthcare experts like endocrinologists, surgeons, and oncologists are vital. Endocrinologists help with hormone issues. Surgeons do surgeries like removing the adrenal gland. Oncologists help plan treatments like chemotherapy.
We work together to make a treatment plan that fits each patient. This team effort ensures patients get the best care from start to finish.
Supportive Care and Symptom Management
Supportive care is a big part of treating adrenocortical carcinoma. We focus on easing symptoms and improving life quality. This includes managing pain, nutrition, and mental health.
By meeting patients’ physical and emotional needs, we can make treatments better. Our team aims to provide care that supports patients fully.
Clinical Trials and Research Participation
Joining clinical trials is important for finding new treatments. We encourage patients to look into these studies. They might get new therapies and help find better treatments.
We’re always looking for new ways to help patients. By joining trials, patients get the latest treatments and help advance care for adrenocortical carcinoma.
Prognosis and Long-term Outcomes
Knowing the prognosis for adrenocortical carcinoma is key for both patients and doctors. The outlook changes a lot based on when the disease is caught and the patient’s health.
Stage-specific Survival Rates
Survival rates by stage give us a clear picture of what to expect. Early detection means a better chance of survival.
- Stage I: Patients have a relatively favorable prognosis with a 5-year survival rate of approximately 60-80%.
- Stage II: The survival rate decreases to around 40-60%.
- Stage III: Patients face a more challenging prognosis, with a 5-year survival rate ranging from 20-40%.
- Stage IV: The prognosis is generally poor, with a 5-year survival rate of less than 20%.
A recent study found that the 5-year survival rate for adrenocortical carcinoma is about 50%. This shows the importance of catching it early and using effective treatments.
Prognostic Factors and Risk Stratification
Several factors affect how well a patient will do with adrenocortical carcinoma. These include:
- Tumor size and stage at diagnosis.
- Histological grade and Ki-67 index.
- Presence of genetic mutations, such as TP53.
- Patient’s age and overall health.
Risk stratification helps doctors plan treatments better and predict how well a patient will do.
Recurrence Patterns and Management
Recurrence is a big worry for those with adrenocortical carcinoma, even after treatment. Some see local recurrence, while others get distant metastases.
Effective management of recurrence needs a team effort. This includes surgery, chemotherapy, and targeted therapy. Regular check-ups are key to catching recurrence early.
In summary, the outlook for adrenocortical carcinoma is complex. But, understanding the factors and having a detailed treatment plan can make a big difference in patient outcomes.
Conclusion
Understanding tumor adrenocortical, like adrenocortical carcinoma, is key for good patient care. We’ve looked at its stages, how it can spread, and treatment choices.
Dealing with tumor adrenocortical needs a team effort. Doctors like endocrinologists, surgeons, and oncologists work together. This helps make treatment plans that fit each patient’s needs.
Knowing how to manage adrenocortical carcinoma is vital. It involves understanding its stages and how to treat it. This includes surgery, medicine, and new targeted therapies. We also need more research and clinical trials to improve treatment.
FAQ
What is adrenocortical carcinoma (ACC), and how does it differ from benign adrenocortical adenomas?
Adrenocortical carcinoma (ACC) is a rare, malignant tumor of the adrenal gland. Benign adrenocortical adenomas are non-cancerous growths. We differentiate between the two based on characteristics, risk factors, and genetic predisposition.
What are the symptoms of adrenocortical tumors, and how do they vary between functioning and non-functioning tumors?
Symptoms of adrenocortical tumors can vary. Functioning tumors produce excess hormones, leading to hormonal manifestations. Non-functioning tumors may present with non-specific symptoms or be discovered incidentally. We evaluate the clinical presentation to determine the tumor’s functionality.
How are adrenocortical tumors diagnosed, and what diagnostic approaches are used?
We diagnose adrenocortical tumors using a combination of imaging techniques, biochemical testing, and hormone evaluation. Biopsy is also considered, but its limitations are taken into account.
What is the complete staging system for adrenocortical carcinoma, and why is it important?
The staging system for adrenocortical carcinoma ranges from Stage I (localized disease) to Stage IV (distant metastasis). Accurate staging is key for determining prognosis and guiding treatment decisions.
How does adrenocortical carcinoma metastasize, and what are the common sites of metastasis?
Adrenocortical carcinoma can metastasize to various sites, including the lungs, liver, and bones. Understanding the patterns of metastatic spread helps us develop effective treatment strategies.
What are the treatment options for adrenocortical carcinoma, including surgical management and medical therapy?
Treatment options for adrenocortical carcinoma include surgical management (open or laparoscopic adrenalectomy) and medical therapy (mitotane, chemotherapy, targeted therapies, and immunotherapy). We also manage hormonal excess and provide supportive care.
What is the role of a multidisciplinary team in managing adrenocortical carcinoma?
A multidisciplinary team, including endocrinologists, surgeons, and oncologists, works together to provide care for patients with adrenocortical carcinoma. They address complex needs and improve outcomes.
What are the prognosis and long-term outcomes for patients with adrenocortical carcinoma?
Prognosis and long-term outcomes vary based on stage, prognostic factors, and risk stratification. We monitor patients closely for recurrence and develop strategies to manage it.
Are there any clinical trials or research studies available for patients with adrenocortical carcinoma?
Yes, we participate in clinical trials and research studies to advance the understanding and treatment of adrenocortical carcinoma. This offers patients access to innovative therapies and contributes to the development of new treatments.
References
American Cancer Society — Adrenal Cancer: Staging.
https://www.cancer.org/cancer/types/adrenal-cancer/detection-diagnosis-staging/staging.html
PubMed Central (PMC) — [Article].