Last Updated on November 27, 2025 by Bilal Hasdemir

Understanding breast cancer pathophysiology is key in the fight against this disease. It’s a major cause of cancer worldwide.
At Liv Hospital, we use the latest medical methods and care with heart. We aim to give the best results in treating breast adenocarcinoma and other related issues.
We’ll dive into the details of cancer mammae. We’ll cover its pathophysiology, stages, and possible complications. This will help both patients and healthcare workers understand this complex condition better.
Key Takeaways
- Understanding breast cancer pathophysiology is essential for effective management.
- Liv Hospital offers advanced medical protocols and compassionate care.
- The article will cover key facts, stages, and complications of breast cancer.
- Breast adenocarcinoma is a significant focus in breast cancer treatment.
- Staying informed about the latest developments in breast cancer research is important.
Understanding Breast Cancer: Epidemiology and Impact

Breast cancer is a big health issue worldwide. It affects women and men, though men are less likely to get it. The disease’s spread and death rates show how big its impact is.
Global Prevalence and Mortality Rates
Studies show breast cancer is the top cancer in women, making up 25% of all cases. It’s estimated that over 2 million new cases happen every year. Sadly, about 15% of all cancer deaths in women are due to breast cancer.
The numbers of breast cancer cases and deaths differ by region and country. In rich countries, more cases are found, but in poor countries, more people die because of late diagnosis and lack of healthcare.
Key statistics include:
- Over 2 million new breast cancer cases diagnosed worldwide each year.
- Breast cancer is the leading cause of cancer-related deaths among women aged 20-59 years.
- The 5-year survival rate for breast cancer varies significantly between high-income and low-income countries.
Risk Factors and Demographic Patterns
Many things can increase the chance of getting breast cancer. These include genes, hormones, and lifestyle. Knowing these helps find who’s at higher risk and how to prevent it.
Demographic patterns also matter. For example, most breast cancer happens in women over 50. Other things like family history, when you had your first period, and your ethnicity also play a part.
Notable risk factors include:
- Genetic mutations, such as BRCA1 and BRCA2.
- Family history of breast cancer.
- Hormonal influences, including early menarche and late menopause.
- Lifestyle factors, such as alcohol consumption and lack of physical activity.
Normal Breast Anatomy and Physiology

To understand breast cancer, we must first know how the breast works normally. The breast is a complex organ with a unique structure. This structure is key to its functions.
Structural Components of the Breast
The breast has glandular, adipose, and connective tissue. The glandular tissue makes milk and is organized into lobules. These lobules drain into ducts, which then merge into larger ducts that open at the nipple.
Hormonal Regulation and Cellular Function
Hormones greatly affect the breast’s function. Estrogen and progesterone control how cells grow and change in the breast. Knowing how these hormones work is vital for understanding breast cancer.
| Hormone | Function | Impact on Breast Tissue |
|---|---|---|
| Estrogen | Promotes cellular proliferation | Influences ductal development and growth |
| Progesterone | Regulates cellular differentiation | Affects lobular development and milk production |
Understanding the normal breast helps us see how cancer changes it. We learn how hormones play a part in this change.
7 Key Facts About Breast Ca Pathophysiology
Breast cancer pathophysiology is complex. It involves genetics, hormones, and the environment. Knowing these factors helps us find better ways to diagnose and treat the disease.
Fact 1: Cellular Origin and Transformation
Breast cancer starts when normal cells turn into cancer cells. This change is caused by genetic mutations. The cells that start breast cancer are often stem cells or progenitor cells in the breast tissue.
Fact 2: Role of Hormonal Influences
Hormones like estrogen and progesterone are important in breast cancer. Estrogen receptor-positive breast cancers grow because of estrogen. Targeting these hormones helps manage the disease. Knowing how hormones affect breast cancer helps doctors choose the right treatments.
Fact 3: Genetic Mutations as Drivers
Genetic changes are major players in breast cancer. Mutations in BRCA1 and BRCA2 genes raise the risk of breast cancer. Other genes, like PIK3CA and TP53, also play a role in cancer growth and treatment success.
Fact 4: Tumor Microenvironment Significance
The area around a tumor is key in breast cancer growth and spread. It includes immune cells, fibroblasts, and endothelial cells. These cells interact with cancer cells, affecting growth. Research aims to find new ways to treat based on these interactions.
Studying breast cancer pathophysiology is vital for better patient care. By understanding the role of cells, hormones, genes, and the tumor environment, we can create more precise treatments.
Histopathological Classification of Breast Cancer
It’s key to know the different types of breast cancer for the right treatment. Breast cancer is not just one disease. It’s a group of diseases with unique features.
Invasive Ductal Carcinoma (Breast Adenocarcinoma)
Invasive ductal carcinoma, or breast adenocarcinoma, is the most common breast cancer. It makes up about 70-80% of all cases. It starts in the milk ducts and grows into the surrounding tissue.
Characteristics: It feels firm or hard in the breast. Cancer cells have invaded beyond the ducts into the tissue.
Invasive Lobular Carcinoma
Invasive lobular carcinoma is the second most common type, making up about 10% of invasive cases. It starts in the lobules and can spread to nearby tissues.
Clinical Implication: It’s harder to find by mammography than invasive ductal carcinoma.
Other Histological Subtypes
There are other, less common types of breast cancer. These include:
- Medullary carcinoma
- Tubular carcinoma
- Mucinous (colloid) carcinoma
| Histological Subtype | Frequency | Characteristics |
|---|---|---|
| Invasive Ductal Carcinoma | 70-80% | Originates in milk ducts, invades surrounding tissues |
| Invasive Lobular Carcinoma | 10% | Begins in lobules, can be harder to detect |
| Medullary Carcinoma | <5% | Distinct boundary, often associated with BRCA1 mutations |
| Tubular Carcinoma | <2% | Well-differentiated, favorable prognosis |
Molecular Classification and Cancer Mammae Subtypes
Breast cancer is a complex disease with different types. These types are identified through molecular classification. This method looks at certain proteins and genes to understand the cancer’s behavior and choose the best treatment.
Hormone Receptor Status (ER/PR)
The hormone receptor status of breast cancer is checked for estrogen and progesterone receptors. If a tumor has these receptors, it’s hormone receptor-positive. These cancers often respond well to hormone therapy. About 70-80% of breast cancers are hormone receptor-positive, making hormone therapy a common treatment.
Tests like immunohistochemistry (IHC) check for ER and PR. These results help doctors decide if hormone therapy will work.
HER2 Status and Its Significance
HER2 is a protein that helps cancer cells grow. HER2-positive cancers grow faster because of too much HER2. Doctors use IHC or FISH tests to find out if a cancer is HER2-positive.
HER2-positive cancers are more aggressive and spread faster. But, new treatments like trastuzumab have greatly improved outcomes for these patients.
Triple-Negative Breast Cancer
Triple-negative breast cancer (TNBC) lacks ER, PR, and HER2. TNBC makes up about 15-20% of breast cancers and is very aggressive. It’s more likely to come back and spread.
Because TNBC doesn’t have hormone receptors or HER2, it doesn’t respond to hormone or HER2-targeted therapies. Chemotherapy is the main treatment for TNBC.
Luminal A and B Subtypes
Luminal A and B are types of hormone receptor-positive breast cancers. Luminal A has high ER-related gene expression and low cell growth. Luminal B has higher cell growth and lower ER levels.
Luminal A cancers usually have a better outlook than Luminal B. Knowing the difference helps doctors choose the best treatment, including hormone therapy and chemotherapy.
In summary, the molecular classification of breast cancer into subtypes has greatly improved our understanding of the disease. This system helps guide treatments, leading to better patient outcomes and more personalized care in breast cancer.
Genetic Basis of Breast Carcinoma
Understanding the genetic roots of breast carcinoma is key to spotting high-risk people and creating targeted treatments. Genes like BRCA1 and BRCA2 are major players in breast cancer. We’ll dive into these genetic factors, looking at how they affect risk and treatment.
BRCA1 and BRCA2 Mutations
BRCA1 and BRCA2 are genes that help fix DNA damage. But, mutations in these genes raise the risk of breast and ovarian cancer. The National Cancer Institute says women with these mutations face a higher risk of breast cancer.
“Having a BRCA mutation is a big risk for breast cancer,” say genetic oncology experts. “Genetic tests can find people who need closer screening and prevention,” they add.
Other High-Risk Gene Mutations
Other genes like TP53, PTEN, and CDH1 also raise breast cancer risk. Mutations in these genes can cause cancer syndromes like Li-Fraumeni and Cowden syndromes. Finding these mutations is key to managing cancer risk.
Polygenic Risk Factors
Genes like BRCA1 and BRCA2 aren’t the only ones at play. Common genetic changes also add to breast cancer risk. Research has found many single-nucleotide polymorphisms (SNPs) linked to breast cancer. Together, these can give a score that shows a person’s risk of breast cancer.
Sporadic vs. Hereditary Breast Malignancy
It’s important to know the difference between sporadic and hereditary breast cancer. This knowledge helps in diagnosing and treating the disease. We will look at the characteristics of each type and how they affect patients and their families.
Sporadic Breast Cancer
Sporadic breast cancer makes up 90-95% of all breast cancer cases. It’s not caused by inherited genes. Instead, it’s linked to lifestyle, environment, and random genetic changes over time.
The risk factors for sporadic breast cancer include:
- Age: Risk goes up after 50.
- Lifestyle factors: Alcohol, lack of exercise, and obesity.
- Hormonal influences: Early menarche, late menopause, and hormone therapy.
Hereditary Breast Cancer
Hereditary breast cancer makes up 5-10% of all breast cancer cases. It’s linked to inherited gene mutations, like BRCA1 and BRCA2. These genes increase the risk of breast cancer, often at a younger age.
The characteristics of hereditary breast cancer include:
- Family history: Many cases in the family.
- Early onset: Cancer diagnosed young.
- Bilateral breast cancer: Cancer in both breasts.
Here’s a comparison of sporadic and hereditary breast cancer:
| Characteristics | Sporadic Breast Cancer | Hereditary Breast Cancer |
|---|---|---|
| Percentage of Cases | 90-95% | 5-10% |
| Genetic Link | No direct inherited genetic link | Associated with inherited gene mutations (e.g., BRCA1, BRCA2) |
| Age of Onset | Typically after 50 | Often at a younger age |
| Family History | Less significant | Significant, with multiple cases across generations |
Knowing the difference between sporadic and hereditary breast cancer is key. It helps in creating the right treatment plans and genetic counseling. We focus on identifying those at high risk and providing them with personalized care and support.
Breast Cancer Staging: Current Authoritative Guidelines
Staging breast cancer is key to patient care. It affects treatment and how well a patient might do. Getting the staging right is vital for knowing how far the disease has spread.
Tumor Size (T) Assessment
Tumor size is very important in breast cancer staging. The size of the tumor is measured in centimeters. This helps decide the T classification.
- T1: Tumor is ≤2 cm
- T2: Tumor is >2 cm but ≤5 cm
- T3: Tumor is >5 cm
- T4: Tumor of any size with direct extension to the chest wall or skin
Lymph Node (N) Involvement
Lymph node involvement is also key in breast cancer staging. It looks at how many nodes are affected and where they are.
- N1: Metastases to movable ipsilateral level I, II axillary lymph nodes
- N2: Metastases in ipsilateral level I, II axillary lymph nodes that are clinically fixed or matted
- N3: Metastases in ipsilateral infraclavicular (level III axillary) lymph nodes
Metastasis (M) Evaluation
Checking for metastasis is vital. It tells if the cancer has spread to other parts of the body. This is important for knowing the disease’s overall stage.
- M0: No distant metastasis
- M1: Distant metastasis present
Integrated Staging System
The integrated staging system uses T, N, and M classifications. It helps figure out the overall stage of breast cancer.
| Stage | T | N | M |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III | T3 | N1 | M0 |
| IV | Any T | Any N | M1 |
Knowing the current guidelines for breast cancer staging is key for healthcare providers. It helps them make the best decisions for patient care. By looking at tumor size, lymph node involvement, and metastasis, they can plan the right treatment.
Progression Pathways in Breast Adenocarcinoma
The growth of breast adenocarcinoma involves local invasion and distant metastasis. It’s key to grasp these steps to create better treatments and outcomes for patients.
Local Invasion Mechanisms
Local invasion is the first step in breast adenocarcinoma growth. Cancer cells spread to the surrounding breast tissue. This happens through changes in cells and molecules, like losing cell adhesion and making enzymes to break down tissue.
Key factors influencing local invasion include:
- Genetic mutations that make cancer cells more invasive
- The tumor microenvironment, which can either suppress or promote tumor growth
- Hormonal influences that regulate the growth and behavior of cancer cells
As cancer cells spread locally, they can harm normal breast tissue. They might even reach nearby structures like the chest wall or skin.
Distant Metastasis Processes
Distant metastasis is when cancer cells move from the original tumor to other organs. This journey includes steps like invasion, getting into blood vessels, traveling through blood, exiting blood vessels, and settling in new areas.
The metastatic cascade is highly inefficient, with only a small fraction of cancer cells successfully establishing metastases. Success depends on the cancer cells’ genetics, the new environment’s readiness, and their ability to avoid the immune system.
“The process of metastasis is not just a simple spread of cells; it’s a complex interplay between the tumor and the host environment.”
Common places for breast adenocarcinoma to spread include bones, lungs, liver, and brain. Knowing how metastasis works is vital for finding new treatments and improving patient care.
Understanding both local invasion and distant metastasis helps us see how breast adenocarcinoma grows. It also points to new ways to treat it.
Complications of Breast Cancer: A Detailed Look
There are many types of complications from breast cancer, each with its own effects. These issues can greatly impact a patient’s life and their chances of recovery. We will dive into these complications, helping you understand their impact and how to manage them.
Local Complications
Local complications come from the tumor itself or its spread nearby. These include:
- Ulceration and Fungation: Advanced tumors can break through the skin, causing a lot of discomfort.
- Pain: When the tumor invades nearby tissues, it can cause severe pain.
- Lymphedema: Blockages in lymphatic pathways can lead to arm swelling, known as lymphedema.
Systemic Complications
Systemic complications happen when cancer spreads to other parts of the body. Common ones include:
- Bone Metastases: Cancer in bones can cause pain, fractures, and high calcium levels.
- Pulmonary Metastases: Cancer in the lungs can lead to breathing problems.
- Liver Metastases: Cancer in the liver can cause liver failure.
- Brain Metastases: Cancer in the brain can lead to neurological issues.
It’s important to understand these complications to manage advanced breast cancer effectively. For more on how breast cancer affects patients, check out Liv Hospital’s resource on breast cancer’s impact.
Treatment-Related Complications
Complications from treatments for breast cancer include:
- Chemotherapy Side Effects: Chemotherapy can cause nausea, hair loss, and a higher risk of infections.
- Radiation Therapy Side Effects: Radiation can cause skin changes, fatigue, and swelling.
- Surgical Complications: Surgery can lead to infections, scarring, and swelling.
- Hormonal Therapy Side Effects: Hormonal therapies can cause menopausal symptoms, mood changes, and osteoporosis risk.
It’s key to manage these complications well to improve patient outcomes and quality of life. A full approach to breast cancer care includes treating the cancer and addressing these complications.
Diagnostic and Monitoring Approaches in Breast Pathology
Managing breast cancer starts with accurate diagnosis and monitoring. We use many methods to detect and track breast diseases.
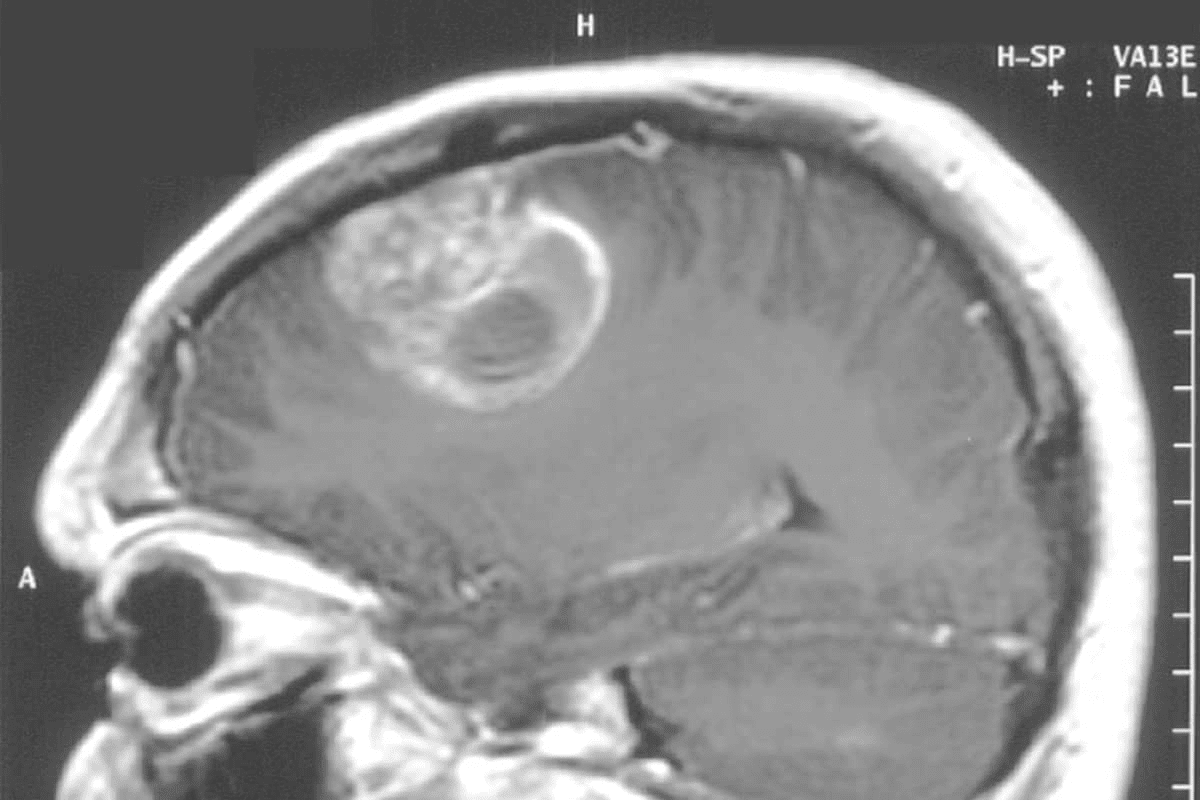
Imaging Modalities
Imaging is key in finding and watching breast cancer. Different imaging tools are used, each with its own benefits.
- Mammography: It’s the main tool for finding breast cancer early.
- Ultrasound: Helps check out any odd spots found on mammograms, great for figuring out what they are.
- MRI: Very sensitive, used for those at high risk or to see how far the cancer has spread.
Biopsy Techniques and Histopathological Analysis
Biopsy methods are vital for getting tissue samples. These samples are then analyzed to confirm a diagnosis.
| Biopsy Technique | Description | Advantages |
|---|---|---|
| Fine-needle Aspiration Biopsy | Uses a thin needle to collect cell samples. | Minimally invasive, quick procedure. |
| Core Needle Biopsy | Removes small cores of tissue for examination. | Provides tissue architecture information. |
| Surgical Biopsy | Involves surgical removal of tissue or the entire lump. | Highly accurate, allows for extensive histological examination. |
Molecular and Genetic Testing Advances
New molecular and genetic tests have improved how we diagnose and treat breast cancer.
- Genetic Testing: Finds mutations in genes like BRCA1 and BRCA2 that raise cancer risk.
- Molecular Profiling: Reveals the tumor’s genetic details, helping choose treatments.
By combining these methods, we offer full care for breast cancer patients. This leads to early detection and better treatment.
Conclusion: Integrating Pathophysiology into Clinical Management
Understanding breast cancer’s pathophysiology is key for good treatment. Studies have found important biomarkers like EPB41L4A-AS1 and LINC00667. These are linked to better survival rates in breast cancer patients, as shown in a Nature study.
Using pathophysiology in treatment planning helps doctors make better choices. The AMPK and PI3K-Akt pathways are important for guiding treatments. Genes like AURKA and CCNB1 are involved in cell growth and death.
Knowing how these genes work helps doctors create targeted treatments. This approach improves patient care and outcomes. Good management of breast cancer needs a deep understanding of its biology.
FAQ
What is breast cancer and how common is it?
Breast cancer starts in the breast tissue. It’s a common cancer in women worldwide. It has a big impact on health globally.
What are the risk factors associated with breast cancer?
Risk factors include genetic mutations like BRCA1 and BRCA2. Family history, hormones, and demographics also play a part. Knowing these helps in early detection and prevention.
What is the pathophysiology of breast cancer?
Breast cancer’s pathophysiology is complex. It involves cells, hormones, genetics, and the tumor environment. We’ve outlined 7 key facts about this, including hormonal and genetic roles.
How is breast cancer classified?
Breast cancer types are based on cell and molecular characteristics. Main types include invasive ductal and lobular carcinomas. There are also molecular types like hormone receptor-positive and HER2-positive.
What is the significance of breast cancer staging?
Staging is key for knowing the disease’s extent and treatment. It looks at tumor size, lymph nodes, and metastasis. This helps guide treatment.
What are the complications associated with breast cancer?
Complications include local issues like tumor invasion and systemic issues like metastasis. Treatment can also cause problems. Understanding these is vital for patient care.
How is breast cancer diagnosed and monitored?
Diagnosis and monitoring use imaging like mammography and ultrasound. Biopsy and genetic testing are also used. These methods help accurately track the disease.
What is the difference between sporadic and hereditary breast cancer?
Sporadic breast cancer is common and not linked to genes. Hereditary breast cancer is rare and linked to genes like BRCA1 and BRCA2.
How do genetic mutations contribute to breast cancer risk?
Mutations in BRCA1 and BRCA2 increase breast cancer risk. Other genes and polygenic factors also play a role in risk.
What is the role of hormonal influences in breast cancer?
Hormones like estrogen and progesterone are key in breast cancer. Knowing hormone receptor status helps in choosing treatments.
References
- National Center for Biotechnology Information (NCBI). NBK564324. https://www.ncbi.nlm.nih.gov/books/NBK564324/
- National Center for Biotechnology Information (NCBI). NBK482286. https://www.ncbi.nlm.nih.gov/books/NBK482286/
- StatPearls / NCBI Bookshelf via Scribd. Breast Cancer. https://www.scribd.com/document/670488391/Breast-Cancer-StatPearls-NCBI-Bookshelf
- StatPearls. “Breast Cancer” (Point‑of‑Care). https://www.statpearls.com/point-of-care/search?q=Breast+Cancer
- StatPearls. “Metastatic Breast Cancer” (Point‑of‑Care). https://www.statpearls.com/point-of-care/search?q=Metastatic+Breast+Cancer