Last Updated on November 27, 2025 by Bilal Hasdemir
Having a prostatectomy or prostate surgery can change a patient’s life, especially for those with prostate cancer, highlighting the effects of prostate removal.
Every surgery, like prostate removal surgery, comes with risks and complications. It’s important for patients to know these risks before the surgery.
Those who have prostate cancer surgery should watch out for dangers right after. Knowing what to expect can help with recovery.
Key Takeaways
- Prostatectomy carries risks and complications.
- Understanding these risks allows patients to better prepare for the surgery and its potential outcomes.
- There are dangers right after surgery.
- Being informed aids in recovery and managing expectations.
- Prostate cancer surgery needs careful thought about complications.
Understanding Prostate Surgery and Its Purpose

Prostate surgery, or prostatectomy, is a procedure to remove part or all of the prostate gland. This gland is key to the male reproductive system. Its removal can have big effects.
The Function of the Prostate Gland
The prostate gland is a small gland, like a walnut, below the bladder in men. It surrounds the urethra and helps make seminal fluid. This fluid nourishes sperm during ejaculation. It also helps control urine flow.
Common Reasons for Prostate Surgery
Prostate surgery is often for prostate cancer or benign prostatic hyperplasia (BPH). BPH makes the prostate gland big, causing urine problems. Surgery is also for recurrent prostatitis or severe urine blockage.
Can You Live Without a Prostate?
Yes, living without a prostate gland is possible. But, prostate removal through radical prostatectomy can change how you urinate and have sex. Men might need to adjust their lifestyle and get extra treatments for these changes.
Types of Prostate Surgical Procedures

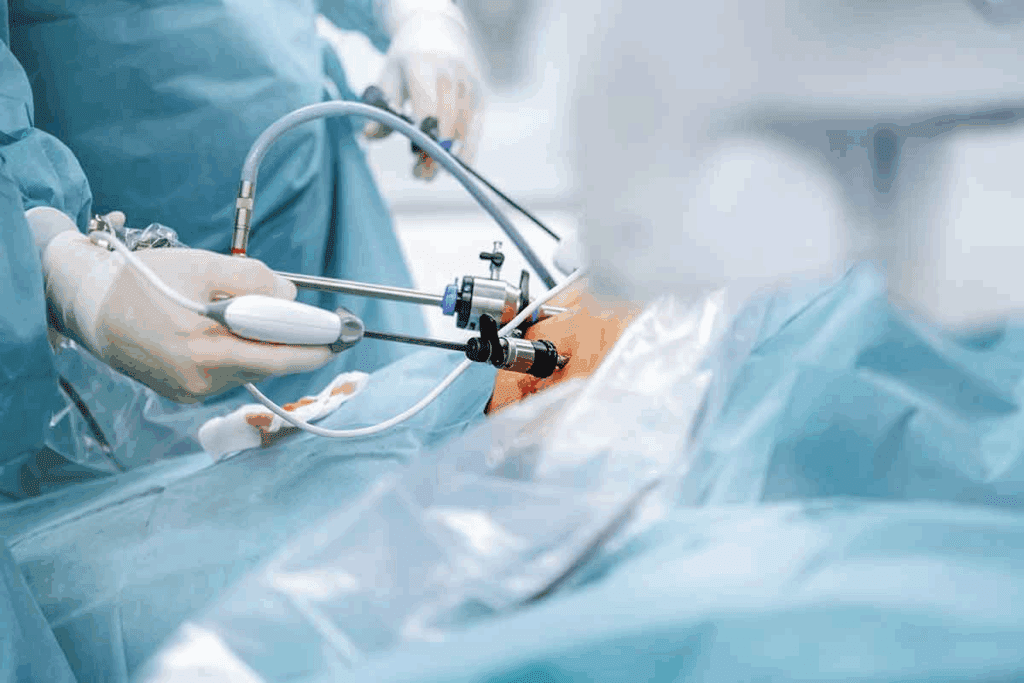
It’s important for patients to know about the different prostate surgeries. These vary based on the patient’s health, the surgeon’s skills, and the technology used.
Radical Prostatectomy
Radical prostatectomy removes the prostate gland, seminal vesicles, and some nearby tissue. It’s mainly for prostate cancer. This surgery can be done in open or minimally invasive ways.
Simple Prostatectomy
Simple prostatectomy removes the inner part of the prostate gland. It’s for symptoms of benign prostatic hyperplasia (BPH). This surgery is less invasive and aims to improve urine flow.
Robotic-Assisted Laparoscopic Prostatectomy
Robotic-assisted laparoscopic prostatectomy uses robotic technology for better surgery. It’s precise, reduces blood loss, and leads to quicker recovery than open surgery.
Open vs. Minimally Invasive Approaches
The choice between open and minimally invasive approaches depends on several factors. These include the patient’s health, cancer stage, and the surgeon’s advice. Minimally invasive surgery, like robotic-assisted, causes less body trauma, leading to faster healing.
Each prostate surgery has its own benefits and drawbacks. Patients should talk to their healthcare provider to find the best treatment for their situation.
Immediate Risks During Prostate Surgery
Understanding these risks allows patients to better prepare for the surgery and its potential outcomes.
Anesthesia-Related Complications
Anesthesia is key for prostate surgery, making it painless. But, it can cause problems like allergic reactions, breathing issues, and heart problems. Having an experienced anesthesiologist watch over you is very important.
Bleeding Risks
Bleeding is a big risk during prostate surgery. It can be mild or serious, sometimes needing blood transfusions. Using advanced techniques and careful bleeding control helps lower this risk.
Organ Injury Potentia
The prostate is close to important organs, which means there’s a chance of damage. This could hurt the rectum, urethra, or nerves that control pee and sex. Planning and doing the surgery carefully helps avoid these problems.
Surgical Site Infections
Any surgery, like prostate surgery, can lead to infections at the site. These infections can be treated with antibiotics, but stopping them before they start is better. Using antibiotics before surgery and keeping everything clean helps prevent infections.
| Risk Category | Description | Mitigation Strategies |
| Anesthesia-Related Complications | Allergic reactions, respiratory and cardiac issues | Experienced anesthesiologist, careful patient monitoring |
| Bleeding Risks | Mild to severe bleeding, possible need for blood transfusions | Advanced surgical techniques, careful bleeding control |
| Organ Injury Potentia | Damage to nearby organs like rectum, urethra, or nerves | Precise surgical planning, careful execution |
| Surgical Site Infections | Infections at the surgical site | Prophylactic antibiotics, sterile surgical techniques |
First 24 Hours After Prostate Surgery
The first 24 hours after prostate surgery are very important. Patients are watched closely for any problems. They also get help to manage pain and avoid future issues.
Post-Anesthesia Recovery
Patients go to a recovery room after surgery. Here, they recover from the anesthesia. Post-anesthesia care is key because patients might feel sick, dizzy, or have nausea.
Nurses keep an eye on the patient’s health and manage pain. They aim to help the patient smoothly move from anesthesia to recovery.
Vital Sign Monitoring
Vital sign monitoring is a big part of care after surgery. Nurses check temperature, blood pressure, heart rate, and oxygen levels often. This helps spot any problems early.
By watching these signs closely, nurses can act fast if something goes wrong. This keeps the patient safe and helps them recover better.
| Vital Sign | Normal Range | Significance |
| Temperature | 97.7°F – 99.5°F | Indicates presence of infection or inflammation |
| Blood Pressure | 90/60 mmHg – 120/80 mmHg | Reflects cardiovascular health and possible bleeding |
| Heart Rate | 60 – 100 beats per minute | Shows heart health and possible bleeding |
Pain Management Protocols
Managing pain well is key in the first 24 hours after surgery. Patients get pain medicine, like epidurals or pills. The goal is to keep pain low so they can rest and start recovering.
Initial Mobility Concerns
Moving around after surgery is good to avoid blood clots and help healing. But, how much they can move depends on their health and the surgery type.
Nurses help patients with their first steps, like getting out of bed or walking. They make sure it’s safe and provide support.
Urinary Complications Following Prostatectomy
After prostate surgery, patients often face various urinary complications. These can affect their recovery and quality of life. It’s important to understand these issues to manage them well.
Urinary Retention
Urinary retention is common after prostate surgery. It makes it hard to empty the bladder completely. This can be due to swelling or nerve problems. Symptoms include a weak urine flow, frequent urination, and trouble fully emptying the bladder.
Catheter Management and Related Issues
Using a catheter is common after prostate surgery to drain urine. But, managing the catheter can lead to problems like discomfort, blockages, or infections. It’s key to take good care of the catheter to avoid these issues.
Urinary Tract Infections
Urinary tract infections (UTIs) are another risk after prostate surgery. The risk goes up with a catheter. Proper care and, if needed, antibiotics can manage UTIs. Common symptoms include burning while urinating, needing to urinate often, and urine that’s cloudy or smells bad.
Urinary Leakage at Surgical Site
Some patients may leak urine at the surgical site. This is usually temporary and can be managed with good wound care. Sometimes, more surgery is needed. Keeping the area clean and dry is key to prevent infection.
To lower the risk of these urinary problems, patients should follow their healthcare provider’s post-operative care closely. Regular check-ups can help catch and manage any issues early.
- Monitor urinary output and report any significant changes to your healthcare provider.
- Follow proper catheter care instructions to reduce the risk of infections.
- Attend all scheduled follow-up appointments to check for any complications.
Bleeding and Hematoma Concerns
Bleeding and hematoma are big worries after prostate surgery. It’s key to know the signs and when to get help.
Internal Bleeding Signs
Internal bleeding can show in different ways. Look out for severe abdominal pain, swelling, or dizziness. If you see these, get medical help right away.
Hematoma Formation
A hematoma is blood outside of blood vessels, near the surgery site. Watch for painful swelling or bruising around the surgery area.
When Bleeding Requires Medical Intervention
Not all bleeding needs a doctor, but some cases do. If you have heavy bleeding, increased pain, or trouble urinating, get help fast.
Monitoring Surgical Drains
Surgical drains help remove fluid after surgery. Keep an eye on them for excessive bleeding or infection signs. Learn how to check them and what to tell your doctor.
| Signs to Monitor | Action Required |
| Severe abdominal pain | Seek immediate medical attention |
| Swelling or bruising around the surgical site | Notify healthcare provider |
| Heavy bleeding or discharge from surgical drains | Contact healthcare provider immediately |
Infection Risks After Prostate Surgery
Infection is a big worry after prostate surgery. It’s important to know the signs and how to prevent it. Knowing about post-operative infections helps doctors take better care of patients.
Wound Infection Symptoms
Wound infections can show up in different ways. Look out for:
- Redness and swelling around the surgical site
- Increased pain or tenderness
- Pus or discharge from the wound
- Fever or chills
Spotting these signs early is key. It helps stop the infection from getting worse.
Systemic Infection Warning Signs
Systemic infections are more serious. They can spread. Watch for:
- High fever
- Chills or shaking
- Confusion or disorientation
- Rapid heartbeat
These signs mean you need to see a doctor right away. It’s to avoid serious problems.
Preventive Measures
To avoid infections, take these steps:
- Keep the wound clean and follow hygiene rules
- Take all antibiotics as told by your doctor
- Watch for infection signs early
- Stay healthy to help your body recover
By doing these things, you can lower your chance of getting an infection after surgery.
Antibiotic Protocols
Antibiotics are very important for preventing and treating infections. They usually include:
- Antibiotics before surgery to lower infection risk
- Antibiotics after surgery based on your health and surgery details
Doctors tailor antibiotic use to each patient. This makes treatment more effective.
In short, knowing about infection risks and taking action can greatly improve recovery. By understanding infection symptoms and following preventive steps, patients can reduce their risk of complications.
Cardiovascular Complications
It’s key for patients getting prostate surgery to know about heart risks. These risks can come from the surgery or from not moving much after it.
Blood Clot Risks
Blood clots are a big worry after prostate surgery. They can happen because of staying in bed too long or not moving enough while recovering. Deep vein thrombosis (DVT) is when a blood clot forms in the deep veins, usually in the legs.
Deep Vein Thrombosis
DVT is serious because it can cause pulmonary embolism if the clot moves to the lungs. Signs of DVT include swelling, pain, or tenderness in the leg.
Pulmonary Embolism Warning Signs
Pulmonary embolism is very dangerous and needs quick medical help. Signs include sudden shortness of breath, chest pain, and coughing up blood. If you see these signs, get medical help right away.
Preventive Strategies
To avoid heart problems, there are steps to take. These include moving around soon after surgery, wearing compression stockings, and taking blood-thinning meds. Patients should listen to their doctors closely to lower these risks.
Knowing the risks and taking steps to prevent them can help patients avoid heart problems after prostate surgery.
Effects of Prostate Removal on Bodily Functions
Prostatectomy can change a man’s health in many ways. It affects urinary and sexual functions. Removing the prostate gland is a big surgery that can impact a patient’s life quality.
Immediate Urinary Control Changes
Prostate removal can change how you control your urine. Many patients face urinary incontinence. This can be from a little leak to not being able to hold it at all. It usually gets better over time, but it can take months or even years.
Using a catheter helps with urine issues at first. But how fast you get better depends on your age, health, and the surgery type.
Initial Sexual Function Impact
Sex life is also affected by prostate removal. Erectile dysfunction is a common side effect. How much it affects you can vary. It depends on the surgery’s success in keeping nerves intact and your sex life before surgery.
Some men might get their sex life back, but others might not. There are treatments like medicines and other options to help with erectile dysfunction.
Hormonal Considerations
The prostate gland helps with male hormones, but removing it doesn’t directly change hormone levels. Yet, it can affect hormone balance indirectly because of body changes.
Some patients might get hot flashes or symptoms like menopause. This is more common with hormone therapy.
Bowel Function Changes
Bowel habits can also change after prostate surgery, but it’s not common. Some might have constipation or changes in bowel habits. These issues are usually short-term and can be fixed with diet changes and other simple steps.
| Bodily Function | Immediate Effects | Long-term Outlook |
| Urinary Control | Incontinence, catheter use | Improvement over time, full recovery possible |
| Sexual Function | Erectile dysfunction | Recovery varies, treatments available |
| Hormonal Balance | Potential for hot flashes | Usually stable, some hormonal changes possible |
| Bowel Function | Constipation, bowel habit changes | Usually short-term, manageable with diet and simple measures |
Pain Management Challenges
Pain management after prostate surgery is complex. It’s key for patient comfort and a smooth recovery.
Expected Pain Levels
Patients face different pain levels after surgery. Pain depends on the surgery type and the person’s pain tolerance. Most feel discomfort in the first days.
Pain Medication Options
Managing pain involves various medications. Opioids, NSAIDs, and acetaminophen are common. The choice depends on pain severity and medical history.
- Opioids: Good for moderate to severe pain.
- NSAIDs: Help with mild to moderate pain and reduce inflammation.
- Acetaminophen: Used with other meds to improve pain relief.
When Pain Indicates Complications
Some pain is normal after surgery. But, severe or worsening pain needs quick medical help. Look out for fever or trouble urinating too.
Non-Pharmaceutical Pain Management
There are non-medication ways to manage pain. These include:
- Physical Therapy: Gentle exercises help move better and feel less pain.
- Relaxation Techniques: Deep breathing, meditation, and muscle relaxation reduce stress and pain.
- Heat or Cold Therapy: Heat or cold on the area can help.
Using these methods can help manage pain and improve recovery.
Recognizing Emergency Warning Signs
Knowing the emergency warning signs after prostate surgery can save lives. After surgery, patients must watch their health closely. They should look out for any signs that could mean a complication.
Complications after prostate surgery are rare but serious. It’s key for patients and their caregivers to know the difference between normal symptoms and those that need urgent care.
When to Call Your Doctor
If you notice any of these symptoms, call your doctor right away:
- Increased pain not managed by your current medication
- Fever over 100.4°F (38°C)
- Redness, swelling, or discharge from the surgical site
- Difficulty urinating or painful urination
- Blood clots or heavy bleeding
Your doctor can offer advice over the phone or might ask you to come in. It’s always safer to be cautious with your health.
When to Go to the Emergency Room
Some symptoms are so severe they need emergency room care. These include:
- Severe bleeding that doesn’t stop
- Chest pain or difficulty breathing
- Severe abdominal pain
- Signs of infection, such as high fever or chills
- Leg swelling or pain, which could indicate a blood clot
If it’s an emergency, don’t wait to get help. As one doctor says,
“Prompt recognition of complications can significantly improve outcomes for patients after prostate surgery.”
| Symptom | Action |
| Mild pain or discomfort | Manage with prescribed medication, call doctor if persists |
| Severe pain or bleeding | Seek emergency care |
| Fever over 100.4°F | Contact your doctor |
Knowing these emergency signs and when to seek help can greatly improve your recovery. Always put your health first and don’t hesitate to contact medical professionals when unsure.
Hospital Discharge and Home Care
Knowing how to move from the hospital to home after prostate surgery is key. A smooth transition is vital for a good recovery.
Typical Hospital Stay Duration
The time in the hospital after surgery can change based on the surgery type and patient health. Those with minimally invasive surgery might stay less than those with open surgery.
Discharge Criteria
Before leaving, patients must meet certain criteria. They need to be able to pee normally, manage pain well, and show no complications. The healthcare team will give care instructions and schedule follow-ups.
Home Preparation Needs
Getting the home ready is important for a safe and comfy recovery. You’ll need pain meds, comfy bedding, and a phone nearby.
Caregiver Support Requirements
Having someone at home can really help with recovery. They can help with daily tasks, watch the patient, and offer emotional support. It’s key for caregivers to know the patient’s needs and watch for any complications.
When moving to home care, following the doctor’s advice and going to follow-up visits is important. Understanding the discharge process and preparing the home can help avoid complications and ensure a good recovery.
First Week Recovery Milestones
After prostate surgery, the first week is key for healing. It’s a time to watch for signs of progress. These signs help set the stage for a good recovery.
Physical Activity Limitations
In the first week, it’s important to rest and move gently. Heavy lifting, bending, or hard activities should be avoided to avoid complications like blood clots.
Short walks are good for keeping blood flowing and preventing constipation. But, it’s important to not push too hard.
Dietary Considerations
Eating well is key for healing. Drink lots of water and eat foods high in fiber to help with constipation.
Steer clear of spicy or heavy foods to ease discomfort and aid in recovery.
Medication Management
Following your medication plan is vital. It helps manage pain, prevent infection, and ensures a smooth recovery. Stick to the dosage and report any side effects to your doctor.
Wound and Catheter Care
Keeping the surgical site and catheter clean is essential. Follow the cleaning and drying instructions given by your healthcare team.
If you have a catheter, watch for signs of infection or blockage. Any issues should be told to your healthcare provider right away.
Returning to Normal Activities
After prostate surgery, knowing when to start normal activities is key. It’s important to slowly get back to daily life. Patients need to follow guidelines for different activities.
Driving Restrictions
Most doctors say not to drive for 1-2 weeks after surgery. This is because you might feel uncomfortable or have trouble moving. Make sure you’re off pain meds before driving again.
Work Return Timeline
When you can go back to work depends on your job and how fast you heal. Usually, it’s 2-6 weeks. Desk jobs might let you return sooner than jobs that are hard on your body.
Exercise Resumption Guidelines
Starting to exercise again is important, but do it slowly. Avoid heavy lifting, bending, or strenuous activities for 4-6 weeks. Start with light walks and gradually increase how long and hard you exercise.
Sexual Activity Considerations
Most doctors say you can start having sex again 6-8 weeks after surgery. But, this can change based on how you heal and what your doctor says. Always listen to your doctor about when to start sex again.
Getting back to normal after prostate surgery takes time and following the right steps. Knowing when to drive, go back to work, exercise, and have sex helps you heal better.
Psychological Impact in the Immediate Recovery Period
Prostate surgery can deeply affect a patient’s mind during the first few weeks. The pain, changes in how the body works, and the stress of surgery can all play a part. It’s important to understand these effects to help patients fully recover.
The effects of prostate surgery on the mind are complex. Patients might feel relieved the surgery is over but also worried about the future. It’s key to know these effects to give the best care possible.
Anxiety and Depression
After prostate surgery, many patients face anxiety and depression. The stress of the surgery and worries about recovery can cause these feelings. Healthcare providers need to watch for these signs closely.
Depression can also happen, often because of big changes in life or past episodes. It’s vital for doctors to keep an eye out for depression during recovery.
Body Image Concerns
Body image issues can also come up after prostate surgery. Changes in how the body works can make patients feel differently about themselves. This can affect their sense of masculinity.
Counseling or support groups can help with these feelings. Patients can share their stories and learn from others who have gone through the same thing.
Coping Strategies
Finding ways to cope is important for dealing with the mind’s response to prostate surgery. Patients can benefit from:
- Staying connected with family and friends
- Trying relaxation techniques like meditation or deep breathing
- Joining support groups
- Living a healthy lifestyle, including eating well and staying active
These strategies can lessen the mind’s stress from surgery and improve overall health.
Support Resources
Having access to support is key for patients after prostate surgery. This includes:
| Resource | Description |
| Support Groups | Groups where patients can share their experiences and get support from others who have gone through similar surgeries. |
| Counseling Services | Professional counseling to help with anxiety, depression, and body image issues. |
| Online Resources | Websites and forums that offer information and support for patients recovering from prostate surgery. |
Using these resources can greatly help patients deal with the mind’s response to prostate surgery.
Conclusion
Prostate surgery, or prostatectomy, is a big medical step. It involves taking out the prostate gland. It’s key for patients to know the risks and complications of this surgery.
We’ve talked about prostate surgery a lot in this article. We covered the different types of surgeries, immediate risks, and complications during recovery. We also looked at how removing the prostate affects the body and why post-operative care is so important.
Understanding these risks allows patients to better prepare for the surgery and its potential outcomes.
Knowing about prostate surgery and its possible complications helps patients make better choices. It also prepares them for what to expect during recovery.
FAQ
What is the immediate danger after prostate surgery?
Right after prostate surgery, you might face bleeding, infection, and heart problems.
What is the function of the prostate gland?
The prostate gland is key in the male body. It makes fluids that are part of semen.
Can you live without a prostate?
Yes, living without a prostate is possible. But, you might need to make some lifestyle changes and deal with side effects.
What are the different types of prostate surgical procedures?
There are several types. These include radical prostatectomy, simple prostatectomy, robotic-assisted laparoscopic prostatectomy, and open prostatectomy.
What are the risks associated with prostate surgery?
Risks include problems with anesthesia, bleeding, injury to organs, infections, and heart issues.
How is pain managed after prostate surgery?
Pain management uses medicines and non-medical ways to ease discomfort.
What are the signs of internal bleeding after prostate surgery?
Look out for severe pain, swelling, or bruising at the site. Also, watch for heavy bleeding or discharge.
How can infection be prevented after prostate surgery?
Use antibiotics, take care of your wound, and watch for infection signs.
What are the urinary complications that can occur after prostatectomy?
You might face urinary retention, infections, or leakage at the site.
How long does it take to recover from prostate surgery?
Recovery time varies. Most men can get back to normal in a few weeks to months.
When can I drive after prostate surgery?
You can’t drive for a few days to a week. It depends on how you’re feeling and your meds.
What are the psychological impacts of prostate surgery?
You might feel anxious, depressed, or have body image issues. There are ways to cope and get support.
How is the catheter managed after prostate surgery?
Proper care and monitoring are key to avoid infections or blockages.
What are the dietary considerations after prostate surgery?
Stay hydrated, eat a balanced diet, and avoid foods that might irritate your urinary tract.
When can I resume exercise after prostate surgery?
Wait a few weeks before starting strenuous activities. Gradually increase your exercise levels.
What are the signs that I should go to the emergency room after prostate surgery?
Go to the emergency room for severe pain, heavy bleeding, trouble urinating, fever, or other serious symptoms.
How is the risk of blood clots minimized after prostate surgery?
Use early movement, compression stockings, and anticoagulant meds to prevent blood clots.
Can prostate surgery affect sexual function?
Yes, surgery can affect sex life. But, the impact varies, and some men might see improvements over time.
What are the benefits of robotic-assisted laparoscopic prostatectomy?
It offers smaller cuts, less blood loss, less pain, and quicker recovery than open surgery.
How is the prostate gland removed during surgery?
The removal method depends on the surgery type. Options include open, laparoscopic, or robotic-assisted techniques.
Reference
- Clements, M. B., et al. (2021). Characterization of symptoms after radical prostatectomy using patient-reported outcomes: Relation to postoperative complications. Journal of Patient-Reported Outcomes. https://pmc.ncbi.nlm.nih.gov/articles/PMC9172597/





