
Recovering from breast cancer surgery, like mastectomy, is a unique journey. It depends on the surgery type, the patient’s health, and following care instructions.
At LIV Hospital, we focus on top-notch healthcare and support for our international patients. Our team knows how vital personalized care is during recovery. Studies show recovery times vary a lot. Some patients get back to normal quickly, while others may need weeks or months.
A study explains how recovery differs with different surgeries. Knowing this helps patients make better choices and get the best results.
Key Takeaways
- Recovery times vary significantly based on the type of mastectomy and reconstruction surgery.
- Patient health and adherence to post-operative care play a critical role in the healing process.
- LIV Hospital provides extensive support for international patients throughout their recovery journey.
- Informed choices and expert care are essential for optimal recovery outcomes.
- Different surgical procedures result in varying levels of pain and physical morbidity.
Understanding Mastectomy: Types and Indications
It’s important for patients to know about the different mastectomy procedures. A mastectomy is a surgery to remove one or both breasts. This is done to treat or prevent breast cancer.
Different Types of Mastectomy Procedures
Mastectomy procedures vary based on how much breast tissue is removed and if lymph nodes are involved. The main types include:
- Total (Simple) Mastectomy: This involves removing the entire breast, including the nipple, areola, and most of the skin.
Total (Simple) Mastectomy
- This procedure is often recommended for patients with early-stage breast cancer or those at high risk.
- Modified Radical Mastectomy: This includes removing the breast tissue and some lymph nodes under the arm.
Modified Radical Mastectomy
- This type is commonly used for patients with invasive breast cancer. It helps check if cancer has spread to lymph nodes.
- Bilateral Mastectomy: This involves removing both breasts, either as a preventive measure or as a treatment for breast cancer.
Bilateral Mastectomy
- A bilateral mastectomy, also known as a double mastectomy, is for patients at high risk of breast cancer. It’s also for those diagnosed with cancer in one breast and at risk in the other.
When a Mastectomy Is Recommended
A mastectomy is recommended based on several factors. These include the stage and type of breast cancer, the tumor’s size, and the patient’s health and preferences. Studies show about 68–73% of women return to work within 3–4 months after surgery.
Mastectomy vs. Lumpectomy: Understanding Your Options
Patients diagnosed with breast cancer often face a choice between mastectomy and lumpectomy. A lumpectomy removes the tumor and a small margin of tissue. A mastectomy removes the breast tissue.
The choice depends on the cancer’s stage, the patient’s breast size, and personal preferences.
Preparing for Your Mastectomy Surgery

Getting ready for mastectomy surgery means thinking about your body, mind, and daily life. We help our patients get ready in every way to make recovery easier.
Physical Preparation Steps
Being physically ready is key for a good surgery. This means:
- Eating well and getting the right nutrients
- Drinking plenty of water
- Doing gentle exercises as your doctor suggests
We give you personal tips to keep your body healthy before surgery.
Emotional and Mental Readiness
Getting emotionally ready is just as important. We suggest:
- Talking to loved ones or joining support groups
- Trying stress-relieving activities like meditation
- Telling your healthcare team about your feelings
Setting Up Your Home for Recovery
Having a cozy place to recover is essential. This includes:
Essential Items for Post-Surgery Comfort
- Wearing comfy clothes, like front-closure bras and loose shirts
- Using pillows and cushions for support
- Having things to do, like books or a tablet
Creating a Support Network
A strong support network helps a lot during recovery. We advise you to:
- Have someone stay with you for a few days after surgery
- Make a list of emergency contacts
- Talk about your recovery plan with your support group
|
Preparation Aspect |
Actions to Take |
|---|---|
|
Physical Preparation |
Healthy diet, hydration, gentle exercises |
|
Emotional Readiness |
Seek support, practice stress reduction, discuss feelings with healthcare team |
|
Home Setup |
Comfortable clothing, supportive pillows, entertainment |
By preparing well for your mastectomy surgery, you can avoid problems and recover better. Our team is here to support you every step of the way.
The Mastectomy Procedure: What to Expect
As you prepare for mastectomy surgery, knowing what to expect can help ease your worries. We’ll guide you through the mastectomy process, from before surgery to after. This includes everything from pre-surgery steps to post-operative care.
Pre-Surgery Protocols
Before surgery, our team will help you with several steps. You’ll have pre-operative testing like blood work and imaging. We’ll also talk about medication management and fasting instructions.
During the Surgery
The mastectomy procedure involves removing the breast tissue. Our surgeons use advanced techniques for the best results. The surgery can last several hours, depending on the case.
Immediate Post-Operative Care
After surgery, you’ll go to the recovery room. Our team will watch over you closely. This includes:
- Hospital Stay Duration: Your hospital stay will depend on your health and surgery details.
- Initial Pain Management: We’ll help manage pain with medications and other methods.
Hospital Stay Duration
Most people stay in the hospital for 1 to 3 days after a mastectomy. This lets our team check on your recovery and address any issues.
Initial Pain Management
Managing pain after mastectomy is key. We’ll use a plan tailored to you, including medication and other treatments.
Initial Recovery Phase: The First Week After Mastectomy
The first week after mastectomy is very important. It’s a time to manage pain, ensure wounds heal well, and avoid complications. Patients must pay close attention to their recovery during this period.
Managing Pain and Discomfort
Managing pain well is key in the early recovery phase. Follow the pain management plan given by your healthcare team. This might include medication and other treatments.
- Take pain medication as directed to manage discomfort.
- Use relaxation techniques such as deep breathing or meditation to help alleviate pain.
Wound Care and Drainage Management
Good wound care is vital to avoid infection and help wounds heal. Your healthcare team will teach you how to care for your surgical site and manage any drains.
- Keep the surgical site clean and dry.
- Monitor for signs of infection, such as redness, swelling, or increased drainage.
Activity Restrictions and Limitations
Knowing what activities to avoid is important for a smooth recovery. Avoid heavy lifting, bending, or strenuous activities.
Safe Movement Techniques
Using safe movement techniques can help reduce discomfort and prevent injury. When getting out of bed, it’s helpful to:
- Move slowly and deliberately.
- Use support, such as pillows or a walker, if necessary.
When to Call Your Doctor
It’s important to know when to seek medical attention. Call your doctor if you experience:
- Increased pain or swelling.
- Signs of infection, such as fever or redness around the surgical site.
- Any concerns about your recovery or wound healing.
Weeks 2-6: The Crucial Healing Period
The time from weeks 2-6 after mastectomy is key for healing. Patients go through big physical changes and reach important healing points.
Physical Changes and Healing Milestones
As the body heals, patients see many changes. They might feel less pain, see swelling go down, and feel sensations return. It’s important to watch these changes closely for a smooth recovery.
Studies show patients with autologous reconstruction feel less pain than those with implants at three months. Knowing this can help set realistic healing expectations.
Gradually Increasing Activities
In weeks 2-6, it’s vital to start doing more to help healing. Gentle exercises help keep muscles strong and joints moving. Always follow what your doctor says to avoid too much strain.
- Start with short walks and gradually increase the distance
- Perform gentle stretching exercises as recommended
- Avoid heavy lifting or bending
Follow-up Appointments and What to Expect
Appointments in weeks 2-6 are key for checking on healing. Doctors can check the site, remove drains, and talk about any issues.
Typical Timeline for Returning to Work
When to go back to work varies based on the job and how fast you heal. Usually, it’s 4-6 weeks, but it might take longer for hard jobs.
|
Job Type |
Typical Return to Work Timeline |
|---|---|
|
Desk Job |
4-6 weeks |
|
Physically Demanding Job |
6-8 weeks or more |
Managing Ongoing Swelling and Discomfort
Swelling and discomfort can last weeks 2-6. It’s important to manage these to improve life quality. Elevation, compression, and pain meds can help.
“Understanding the healing process and what to expect during the critical healing period can help patients plan and recover effectively.”
Knowing about physical changes, healing milestones, and activity guidelines helps patients recover better. Regular check-ups and knowing what to expect make the healing process better.
Long-term Recovery: Months 1-6 After Mastectomy
After surgery, patients start a long recovery phase. This phase focuses on physical healing, emotional adjustment, and getting back to normal life. At LIV Hospital, we offer full support during this important time.
Return to Work Statistics and Considerations
Going back to work after mastectomy is a big step. Many patients can return to their jobs a few months later.
The 68-73% Return Rate Within 3-4 Months
Studies say 68% to 73% of patients go back to work in 3 to 4 months. This shows how recovery times can vary and why care should be tailored to each person.
Workplace Accommodations
Employers can help a lot when employees return to work. They can offer flexible hours, change job tasks, or reduce workloads temporarily.
Physical Therapy and Rehabilitation
Physical therapy is key for long-term recovery after mastectomy. It helps patients get stronger, move better, and avoid problems like lymphedema.
Monitoring for Complications
Even with a good recovery, it’s important to watch for complications. Regular check-ups with doctors can catch any issues early.
Signs of Healthy vs. Problematic Recovery
Patients should know the signs of a good recovery, like better mobility and less pain. They should also watch for warning signs of problems, like swelling, severe pain, or infection.
Understanding long-term recovery helps patients after mastectomy. At LIV Hospital, we offer a team approach to care and support every step of the way.
Factors Affecting Mastectomy Recovery Outcomes
Knowing what affects mastectomy recovery is key for better care. Recovery from mastectomy surgery is complex. It depends on many factors, both personal and surgical.
Surgical Technique and Procedure Type
The type of mastectomy and the surgical method used greatly impact recovery. Different surgeries vary in complexity and invasiveness. This can change how long it takes to heal and the risk of complications.
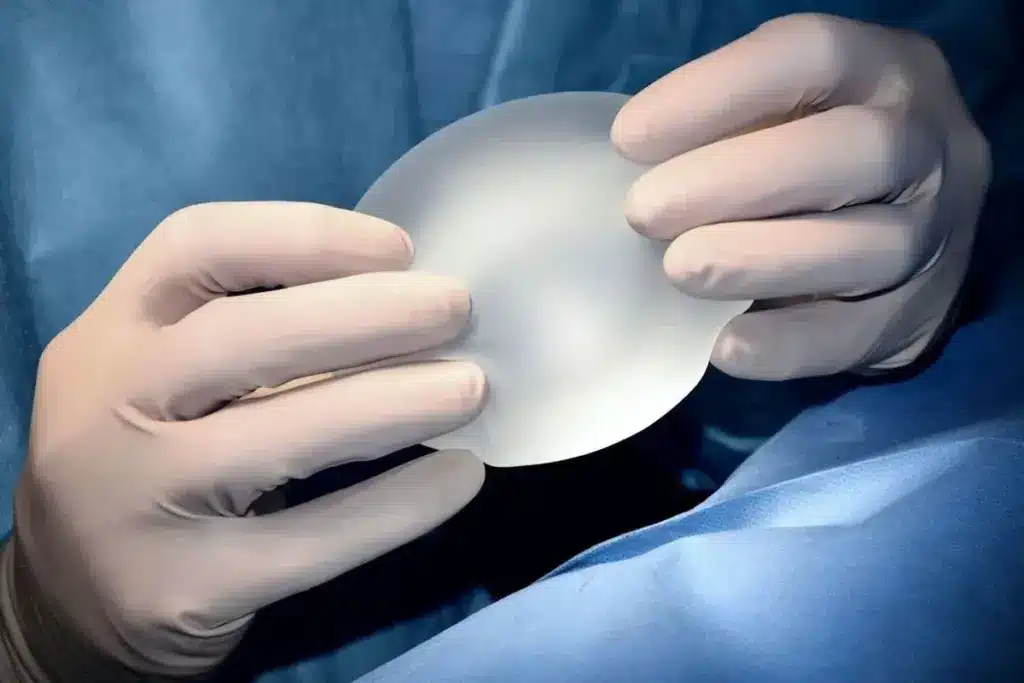
Implant vs. Autologous Reconstruction Recovery Differences
Choosing between implant-based and autologous reconstruction affects recovery. Implant reconstruction often means shorter surgery and recovery times. On the other hand, autologous reconstruction may need longer surgery and recovery due to its complexity.
|
Reconstruction Type |
Surgery Time |
Recovery Time |
|---|---|---|
|
Implant Reconstruction |
Shorter |
Shorter |
|
Autologous Reconstruction |
Longer |
Longer |
Age and Overall Health Considerations
A patient’s age and health are very important for mastectomy recovery. Older patients or those with health issues may need more time to recover. They might also face a higher risk of complications.
Individual Healing Ability and Genetics
Genetics can affect how well someone heals after surgery. Knowing this can help tailor post-operative care to each patient.
Adherence to Post-Operative Care Instructions
It’s vital to follow the surgeon’s post-operative care instructions for the best recovery. This includes proper wound care, managing pain, and following activity restrictions.
Physical Rehabilitation After Mastectomy
Physical rehabilitation is key after a mastectomy. It helps patients regain strength and health. A good rehabilitation plan makes recovery better.
Managing Lymphedema Risk
Lymphedema is a risk after mastectomy, causing swelling. To avoid it, patients should not lift heavy things. Early detection and intervention are vital. Patients should watch for swelling and tell their doctor if they notice it.
Exercises for Strength and Mobility
Exercises are important for getting strong and moving well after surgery. They are made just for the person’s needs.
Early Phase Exercises
At first, simple exercises like shoulder rolls and arm raises are good. Start slow and get more intense as you heal.
Progressive Strength Training
When you’re healing, you can do harder exercises. This might include resistance bands or light weights.
Scar Management and Breast Reconstruction Considerations
Managing scars well is important. Massage and silicone gel sheets can help. For those thinking about breast reconstruction, a good plan is key. We help patients create a plan that meets their needs.
LIV Hospital’s Multidisciplinary Approach to Mastectomy Care
At LIV Hospital, we’re proud of our mastectomy care. We use a team effort to help patients from start to finish. Our goal is to give the best care possible.
State-of-the-Art Surgical Techniques
We use the newest surgical methods and tools for mastectomy patients. Our surgeons are experts in oncoplastic surgery and nipple-sparing mastectomy. They focus on combining advanced techniques with caring for patients.
Comprehensive Recovery Support Services
Recovering from mastectomy surgery is key. We offer many support services to help patients get better. These include:
- Specialized Physical Therapy Programs to help patients regain strength and mobility.
- Psychological Support Resources to help with the emotional side of mastectomy and recovery.
Patient-Centered Care Philosophy
At LIV Hospital, we put patients first. We customize our care to meet each patient’s needs. This ensures they get the support they need during treatment.
We’re always working to improve our care and follow ethical, team-based care paths. Our mission is to provide top-notch healthcare with full support for international patients. We aim to make every patient’s experience as smooth and supportive as possible.
“The care I received at LIV Hospital was exceptional. From the initial consultation through recovery, the team was supportive and professional.”
Conclusion: Embracing Life After Mastectomy
Recovering from mastectomy is a journey that needs support and care. At LIV Hospital, we offer top-notch healthcare and support for international patients. Our team works together to help patients through every step of recovery.
Mastectomy recovery has many stages, from the first steps to long-term healing. Knowing what affects recovery helps patients prepare. Our team at LIV Hospital is here to guide and support you every step of the way.
With the right care and support, patients can overcome mastectomy recovery challenges. We encourage patients to be active in their recovery. Working with your healthcare team, you can achieve the best results and truly enjoy life after mastectomy.
FAQ
What is a mastectomy, and what are the different types of mastectomy procedures?
A mastectomy is a surgery to remove one or both breasts, often for breast cancer. There are several types, like total (simple) mastectomy, modified radical mastectomy, and bilateral mastectomy.
What is the difference between a mastectomy and a lumpectomy?
A mastectomy removes the whole breast, while a lumpectomy takes out part of it. The choice depends on the cancer’s stage and type, and the patient’s health.
How long does it take to recover from a mastectomy?
Recovery time varies based on health, age, and surgery type. Generally, it takes weeks to months to fully recover.
What are the common complications associated with mastectomy surgery?
Common issues include infection, bleeding, and lymphedema. Knowing the signs and telling your doctor quickly is important.
How can I manage pain and discomfort after a mastectomy?
Manage pain with medication, rest, and gentle exercise. Follow your doctor’s advice and report any issues.
What is lymphedema, and how can I manage the risk after a mastectomy?
Lymphedema is swelling due to lymph node removal. Avoid heavy lifting and do exercises as advised by your doctor to reduce risk.
Can I undergo breast reconstruction after a mastectomy?
Yes, many patients choose breast reconstruction after a mastectomy. The timing and type depend on your health and the surgery type. Talk to your doctor about options.
How will a mastectomy affect my ability to return to work?
Returning to work after a mastectomy varies by job, health, and surgery extent. Discuss plans with your doctor and employer.
What kind of support services are available during mastectomy recovery?
LIV Hospital offers physical therapy, psychological support, and education for mastectomy patients. Use these resources for a better recovery.
What are the signs of healthy versus problematic recovery after a mastectomy?
Look for signs of healthy recovery like symptom improvement and wound healing. Watch for signs of complications like pain, redness, or swelling. Report any concerns to your doctor.
References
National Center for Biotechnology Information (NCBI): https://pmc.ncbi.nlm.nih.gov/articles/PMC11931387/





