Primary hepatobiliary cancers are a big worry globally. They mainly include hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (iCCA).
These cancers are becoming more common. They cause hundreds of thousands of deaths each year. It’s important to know about them early and get the best care possible.
Liv Hospital is dedicated to giving top-notch care to those dealing with these serious diseases.
Key Takeaways
- Primary hepatobiliary cancers include HCC and iCCA.
- These cancers are increasingly common worldwide.
- Over 800,000 new cases are diagnosed annually.
- Early awareness and advanced care are key.
- Liv Hospital provides innovative, patient-focused care.
Overview of the Hepatobiliary System
To understand hepatobiliary cancers, we must first know the normal workings of the hepatobiliary system. This system includes the liver, bile ducts, and gallbladder. It’s key for digestion, metabolism, and health.
Anatomy and Function of the Liver
The liver is the biggest organ inside us. It does many important jobs. It cleans toxins, makes proteins, and helps with digestion.
The liver gets blood from two sources: the hepatic artery and the portal vein. This setup helps it do its jobs well.
The liver’s main unit is the hepatic lobule. It helps exchange substances between cells and blood. The liver cells, or hepatocytes, handle many metabolic tasks.
|
Liver Function |
Description |
|---|---|
|
Detoxification |
Removes toxins and waste from the blood |
|
Protein Synthesis |
Makes proteins for blood clotting, transport, and more |
|
Bile Production |
Makes bile for fat digestion and vitamin absorption |
Bile Ducts and Gallbladder Structure
The bile ducts and gallbladder are vital for fat digestion. The bile ducts carry bile from the liver to the gallbladder and then to the small intestine.
The gallbladder stores bile, making it more concentrated. It releases bile into the common bile duct when we eat. The common bile duct joins the pancreatic duct at the ampulla of Vater, emptying into the duodenum.
Knowing how bile ducts and the gallbladder work is key to understanding biliary tract cancers. These cancers can happen in any part of this system.
Understanding Hepatobiliary Cancer Types and Classification
Hepatobiliary malignancies are cancers that affect the liver and bile ducts. They come in many forms, each with its own characteristics. This makes it important to classify them for proper diagnosis and treatment.
Definition and Scope of Hepatobiliary Malignancies
Hepatobiliary malignancies are cancers that start in the liver and bile ducts. They are different in how they grow and how they affect people. Knowing about these differences is key for treatment.
Doctors classify these cancers based on where they start and what cells they come from. The main types are:
- Hepatocellular carcinoma (HCC), which starts in liver cells
- Intrahepatic cholangiocarcinoma (iCCA), from the bile ducts inside the liver
- Extrahepatic cholangiocarcinoma, in the bile ducts outside the liver
- Gallbladder cancer, from the gallbladder
Primary vs. Secondary Liver Cancers
There’s a big difference between primary and secondary liver cancers. Primary cancers start in the liver. Secondary cancers spread to the liver from other places.
Primary liver cancers are hepatocellular carcinoma and intrahepatic cholangiocarcinoma. They are linked to things like viral hepatitis and alcohol use. Non-alcoholic steatohepatitis (NASH) is also a risk factor.
Secondary liver cancers come from other cancers, like the colon or breast. Treating primary and secondary cancers is different.
It’s vital for doctors to know about the different types of hepatobiliary cancers. This helps them give the best care. It also helps patients make smart choices about their treatment.
Hepatocellular Carcinoma (HCC): The Predominant Liver Cancer
Hepatocellular carcinoma (HCC) is the main type of liver cancer worldwide. It’s important to understand how it works and what makes it different. HCC is the most common liver cancer, making up a big part of liver cancers.
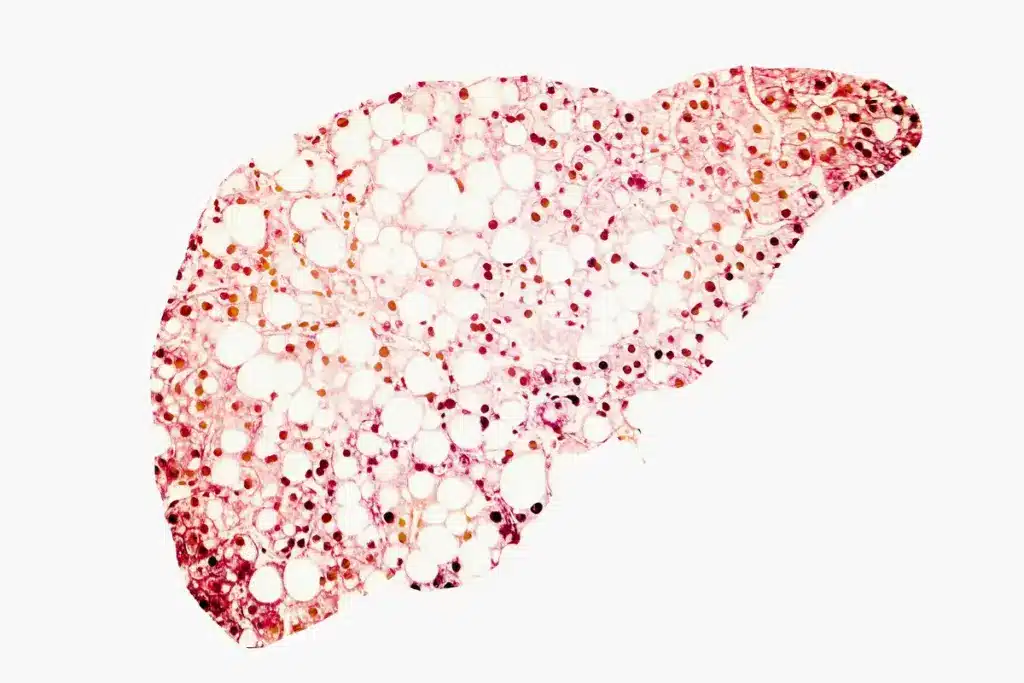
Pathophysiology and Development
HCC develops in a complex way, with many factors involved. Chronic liver disease, caused by hepatitis B or C, alcohol, or NASH, is a big risk. The process starts with liver injury, leading to inflammation and scarring.
This scarring can turn into cirrhosis, a serious liver condition. Cirrhosis can lead to HCC. The changes involve many genetic and molecular steps.
Cellular and Molecular Characteristics
HCC has different cells and molecular changes. Tumors can look very different, from well-differentiated to poorly differentiated. Genetically, HCC has changes in the TP53 and CTNNB1 genes.
These changes affect how the tumor grows and survives. They also make the tumor harder to treat. The Wnt/β-catenin, PI3K/AKT/mTOR, and MAPK/ERK pathways are often altered in HCC.
Growth Patterns and Variants
HCC can grow in different ways, like nodular, massive, or diffuse types. The nodular type is the most common. Knowing how it grows helps doctors plan treatment.
There are also variants of HCC, like fibrolamellar HCC. It’s different because it happens in younger people without liver disease. It has a unique look with fibrous stroma.
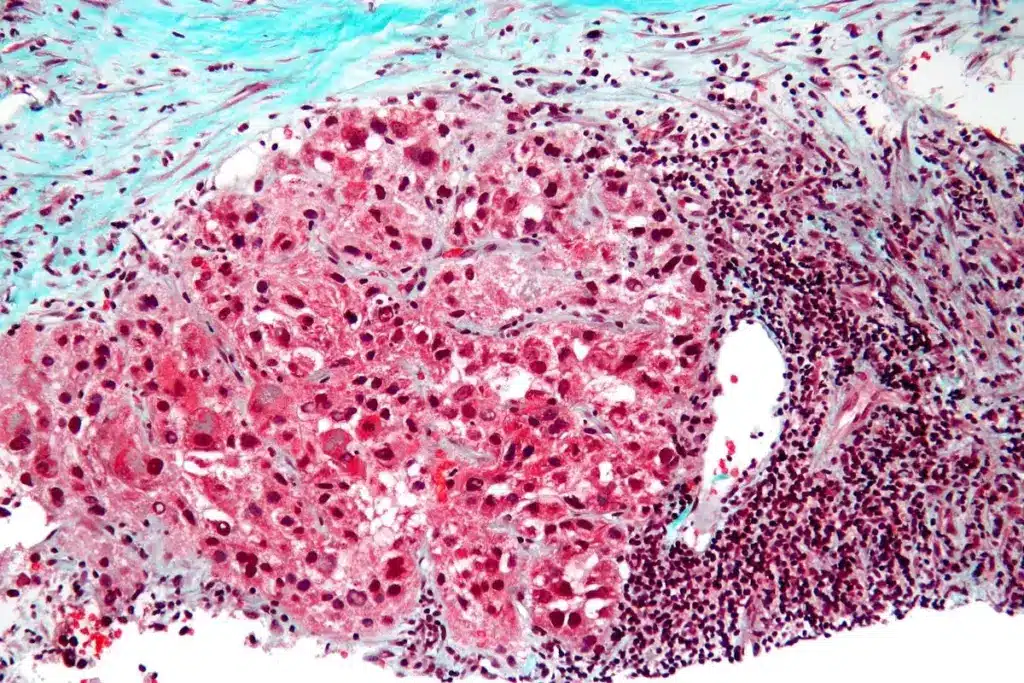
Intrahepatic Cholangiocarcinoma (iCCA): Bile Duct Cancer Within the Liver
iCCA is a cancer that starts in the bile ducts inside the liver. It’s different from other cholangiocarcinomas that start outside the liver. This makes it harder to diagnose and treat.
Pathological Features and Development
The growth of iCCA involves complex processes. Chronic inflammation and bile duct injury are major causes. It often grows quietly, making it hard to catch early.
iCCA has different types, like small duct and large duct. Knowing these types helps doctors find better treatments.
Molecular Subtypes and Genetic Alterations
Research has found different types of iCCA based on genetic changes. These include changes in IDH1/2, FGFR2, and other genes. These changes help the cancer grow and spread.
- IDH mutations are linked to a specific type and might be treated with certain drugs.
- FGFR2 fusions are another genetic change found in iCCA. They could be targets for new treatments.
Learning about these genetic changes helps us understand iCCA better. It also leads to new treatments, improving care for patients.
Global Epidemiology of Hepatobiliary Cancers
Hepatobiliary cancers are a big health problem worldwide, with over 800,000 new cases each year. It’s key to know about these cancers to fight them better.
These cancers happen more in some places than others. This is because of things like where you live, how you live, and your genes.
Worldwide Incidence and Mortality Rates
The number of new cases of these cancers varies a lot around the world. East Asia and parts of Africa have the highest rates. This is because of common infections like hepatitis B and C. In contrast, Western countries have lower rates.
Death rates from these cancers also change a lot by place. In places where health care is hard to get, more people die. This shows we need better ways to find and treat these cancers.
Geographic Variations and Trends
Where you live affects your risk of getting these cancers. Viral infections, eating foods with aflatoxins, and drinking alcohol are big risks. For example, places with lots of hepatitis B virus infections see more liver cancer.
|
Region |
Incidence Rate (per 100,000) |
Mortality Rate (per 100,000) |
|---|---|---|
|
East Asia |
35.5 |
32.1 |
|
Sub-Saharan Africa |
22.1 |
20.5 |
|
Western Europe |
7.3 |
5.6 |
|
North America |
6.8 |
5.1 |
Knowing where these cancers are more common helps us make better health plans. This way, we can help more people with these cancers.
Hepatobiliary Cancer in the United States: Statistics and Projections
It’s important to know about hepatobiliary cancer stats to fight it better in the US. These cancers, like liver and bile duct ones, are tough to beat. They often get diagnosed too late.
Liver cancer is growing fast as a cause of death in the US. For more on liver cancer stats, check outthe American Cancer Society’s liver cancer page.
Current Incidence and Mortality Data
Hepatobiliary cancer rates differ a lot in the US. Liver cancer rates have gone up over the years. The rate of liver cancer has tripled from 1980 to now.
|
Year |
Incidence Rate |
Mortality Rate |
|---|---|---|
|
2010 |
6.8 per 100,000 |
5.1 per 100,000 |
|
2015 |
8.9 per 100,000 |
6.7 per 100,000 |
|
2020 |
11.5 per 100,000 |
8.9 per 100,000 |
Mortality rates for these cancers are also going up. This shows we need better treatments and ways to survive these cancers.
Demographic Patterns and Future Trends
Some groups face higher risks of getting these cancers. This is because of things like viral hepatitis, drinking too much, and fatty liver disease.
Demographic Disparities:
- Males get liver cancer more often than females.
- Hispanic and Asian people get liver cancer more, likely because of hepatitis B.
- People with less money might not get checked or treated early, which can make things worse.
Unless we act, these cancer rates will keep going up. We need to fight hepatitis B and C, drink less, and manage obesity and diabetes to stop this.
Gender Disparities in Hepatobiliary Malignancies
Hepatobiliary malignancies show a clear gender gap, with men more often affected than women. Men are two to three times more likely to get these cancers than women. This highlights a big difference in how susceptible each gender is.
Male Predominance: Underlying Factors
The reason for more men getting these cancers is a mix of genetic, hormonal, and lifestyle factors. Research points to sex hormones as key players in cancer risk.
Sex Hormone Influence: Androgens might help grow liver cancer, while estrogens could protect against it. This hormonal effect could explain why men are more likely to get these cancers.
Hormonal and Genetic Influences
Genetic differences between men and women also play a role. Some genetic mutations are more common in men, making them more at risk for these cancers.
The relationship between hormones and genes is complex. Scientists are working hard to understand how these factors lead to gender disparities in these cancers.
|
Factor |
Men |
Women |
|---|---|---|
|
Hormonal Influence |
Androgens may increase risk |
Estrogens may offer protection |
|
Genetic Mutations |
Higher prevalence of certain mutations |
Lower prevalence |
|
Lifestyle Factors |
Higher rates of alcohol consumption and smoking |
Lower rates of alcohol consumption and smoking |
Knowing these factors is key to creating better prevention and treatment plans for these cancers.
Viral Hepatitis as a Major Risk Factor
Viral hepatitis, like hepatitis B and C, is a big deal in causing liver cancer. Being infected with these viruses for a long time raises your risk of getting liver cancer.
Hepatitis B Virus (HBV) and Carcinogenesis
HBV is a known cause of hepatocellular carcinoma. It does this by getting into the host’s DNA and messing with cell functions. This virus causes long-term inflammation and damage, making it easier for cancer to start.
Hepatitis C Virus (HCV) and Liver Cancer Development
HCV is also a big risk factor for liver cancer. It leads to chronic inflammation and cirrhosis, which can turn into liver cancer. The virus and the host’s immune system have a complex relationship that leads to cancer.
The comparison between HBV and HCV in terms of their association with liver cancer is highlighted in the following table:
|
Virus |
Primary Mechanism |
Cancer Risk |
|---|---|---|
|
HBV |
Integration into host genome, disruption of cellular processes |
High |
|
HCV |
Chronic inflammation, cirrhosis |
High |
It’s important to understand how viral hepatitis leads to liver cancer. This knowledge helps in preventing and treating liver cancer early. Vaccines against HBV and treatments for HCV are key to lowering liver cancer rates worldwide.
Alcohol-Related Hepatobiliary Carcinogenesis
Alcohol-related liver disease is a big problem worldwide. It leads to many liver cancers, like hepatocellular carcinoma (HCC). Alcohol damages the liver in many ways, causing cancer.
Mechanisms of Alcohol-Induced Liver Damage
When the liver breaks down alcohol, it makes a harmful substance called acetaldehyde. This substance hurts liver cells. It also starts inflammation, which can lead to liver damage and cancer.
Drinking alcohol often can cause fatty liver, hepatitis, and cirrhosis. These conditions raise the risk of getting liver cancer.
Alcohol’s breakdown also creates harmful oxygen species. These can damage DNA and upset how cells work. This damage, along with inflammation, helps cancer grow.
Progression from Alcoholic Liver Disease to Cancer
Going from liver disease to cancer involves changes in genes and how cells work. Liver cells get hurt and then fix themselves, leading to mutations. Cirrhosis makes liver cancer more likely because it shows the liver is very damaged.
It’s important to watch for liver cancer early in people who drink a lot. Knowing how alcohol causes liver cancer helps us find ways to prevent it. This can help lower the number of liver cancers worldwide.
Non-Alcoholic Steatohepatitis (NASH) and Emerging Cancer Risk
NASH is a severe form of non-alcoholic fatty liver disease. It’s becoming a major risk factor for liver cancer. This condition causes inflammation and damage to liver cells, leading to cirrhosis and liver cancer.
The causes of NASH are complex. They involve environmental factors, genetic predisposition, and metabolic dysregulation. Knowing these factors helps us find high-risk individuals and take preventive steps.
The Rising Importance of NASH in Cancer Development
The number of people with NASH is growing worldwide. This is because of the rise in obesity and metabolic syndrome. NASH is becoming a big risk factor for liver cancer, the most common type.
Research shows that NASH patients face a higher risk of liver cancer, even without cirrhosis. The chronic inflammation and oxidative stress in NASH start the cancer process.
Metabolic Syndrome and Hepatobiliary Malignancy
Metabolic syndrome is linked to NASH. It includes obesity, high blood pressure, and insulin resistance. Having metabolic syndrome makes the risk of liver cancer worse.
|
Component of Metabolic Syndrome |
Association with Hepatobiliary Malignancy |
|---|---|
|
Obesity |
Increased risk of HCC and other hepatobiliary cancers |
|
Insulin Resistance/Diabetes |
Enhanced carcinogenesis through chronic inflammation and metabolic dysregulation |
|
Dyslipidemia |
Contributes to liver inflammation and damage |
|
Hypertension |
Potential role in promoting tumor growth and progression |
The connection between NASH, metabolic syndrome, and liver cancer is clear. We need to manage these conditions well. Early detection and treatment in people with NASH and metabolic syndrome are key to lowering liver cancer risk.
Clinical Presentation and Diagnostic Challenges
Hepatobiliary malignancies are hard to detect early because they don’t show clear symptoms. Their symptoms can look like other stomach problems, making it tough to figure out what’s wrong.
Early Signs and Symptoms
In the beginning, people with these cancers might feel abdominal discomfort, weight loss, and fatigue. These signs are often thought to be from common issues, which can slow down finding the right diagnosis.
The early signs can also include:
- Nonspecific abdominal pain
- Loss of appetite
- Nausea and vomiting
Advanced Disease Manifestations
When the disease gets worse, symptoms get more obvious. People might see jaundice, pruritus, and significant weight loss. By then, the cancer is often too far along, making treatment harder.
A summary of the advanced disease manifestations is provided in the table below:
|
Symptom |
Description |
|---|---|
|
Jaundice |
Yellowing of the skin and eyes due to bile duct obstruction |
|
Pruritus |
Severe itching, often associated with cholestasis |
|
Significant Weight Loss |
Unintentional weight loss, a common sign of advanced cancer |
Diagnosing hepatobiliary cancers is tough, which is why doctors need to be extra careful. They must use their skills, imaging, and lab tests to catch it early.
Modern Diagnostic Approaches for Hepatobiliary Cancers
Modern diagnostic techniques are key in finding and understanding hepatobiliary cancers. These methods have grown more advanced. They help doctors diagnose these cancers better, leading to better care for patients.
Advanced Imaging Techniques
Advanced imaging is vital for spotting and checking on hepatobiliary cancers. These include:
- Multiphasic Computed Tomography (CT): Gives clear pictures of the liver and bile ducts. It helps find tumors and see how big they are.
- Magnetic Resonance Imaging (MRI): Shows detailed images of soft tissues. It’s great for figuring out liver lesions and checking on blood vessels.
- Positron Emission Tomography (PET): Shows how active tumors are. It’s useful for finding where cancer has spread and how well treatments are working.
Laboratory Tests and Tumor Markers
Laboratory tests and tumor markers are key for diagnosing and keeping an eye on hepatobiliary cancers. Important tests include:
- Alpha-fetoprotein (AFP): High levels are linked to liver cancer.
- Carbohydrate Antigen 19-9 (CA 19-9): Often high in bile duct cancer.
- Liver function tests: Check how well the liver is working and spot problems.
Biopsy and Histopathological Examination
Biopsy and histopathological examination are the top ways to diagnose hepatobiliary cancers. These steps involve:
- Fine-needle aspiration biopsy: Takes tissue samples from suspicious areas.
- Histopathological analysis: Looks at tissue samples to find out if there’s cancer and what type.
Using these modern methods together makes diagnosing hepatobiliary cancers more accurate. This leads to better treatment plans and better care for patients.
Staging and Prognostic Assessment
Accurate staging and prognostic assessment are key for treating hepatobiliary cancers. Staging shows how far the disease has spread. This helps predict outcomes and guide treatment.
TNM Classification and Other Staging Methods
The TNM system looks at tumor size, lymph node involvement, and metastasis. Other systems like Okuda and CLIP score are used for specific cancers. The choice of system affects treatment and prognosis.
The choice of staging system can significantly impact treatment planning and patient prognosis.
Healthcare providers need to know the strengths and weaknesses of each system. This helps them make better decisions for patient care.
Comprehensive Treatment Strategies for Hepatobiliary Cancer
Managing hepatobiliary cancer requires a detailed treatment plan. It combines different methods for the best results. Each patient’s case is unique, so a personalized approach is key.
Surgical Approaches and Liver Transplantation
Surgery and liver transplants can cure early-stage hepatobiliary cancers. The choice of surgery depends on the tumor’s location and the patient’s liver health.
Liver Resection: This surgery removes the tumor and some healthy liver. It aims to get rid of the cancer while keeping enough liver function.
Liver Transplantation: For tumors that can’t be removed or liver disease, a transplant might be an option. It replaces the sick liver with a healthy one from a donor.
|
Surgical Approach |
Indications |
Benefits |
|---|---|---|
|
Liver Resection |
Resectable tumors, adequate liver function |
Potential cure, preserves liver function |
|
Liver Transplantation |
Unresectable tumors, underlying liver disease |
Potential cure, treats underlying liver disease |
Locoregional Therapies
Locoregional therapies target the tumor directly, reducing side effects. They’re good for patients with localized disease who can’t have surgery.
Radiofrequency Ablation (RFA) and Transarterial Chemoembolization (TACE) are common treatments. RFA uses heat to kill tumor cells. TACE delivers chemotherapy directly to the tumor and then blocks blood supply.
Systemic Treatments and Targeted Therapies
Chemotherapy and targeted therapies treat cancer that has spread or can’t be treated locally. These treatments aim to kill cancer cells all over the body.
Targeted Therapies target specific cancer growth drivers. For hepatobiliary cancers, they can reduce harm to normal cells.
Multidisciplinary Care Approach
A team of specialists is essential for managing hepatobiliary cancer. Liv Hospital uses a team approach, ensuring patients get care tailored to their needs.
This team effort leads to personalized treatment plans. It combines the latest in surgery, locoregional therapies, systemic treatments, and supportive care to improve outcomes.
Emerging Therapies and Research Directions
New treatments are changing how we fight liver and bile duct cancers. This is bringing hope to many patients. The field of liver cancer treatment is growing fast, with new ways to help patients.
Immunotherapy Advances
Immunotherapy is a big hope for liver cancer treatment. It uses the body’s immune system to attack cancer cells. This could be a more effective way to treat the disease.
Checkpoint Inhibitors are a type of immunotherapy that looks promising. They help the immune system fight cancer by blocking certain proteins.
- Monoclonal antibodies targeting PD-1/PD-L1 have shown good results in trials.
- Researchers are looking into combining checkpoint inhibitors with other treatments.
Molecular Targeted Agents
Molecular targeted agents are another key area of research. These treatments aim at specific changes in cancer cells that help them grow.
|
Targeted Agent |
Mechanism of Action |
Clinical Application |
|---|---|---|
|
Sorafenib |
Multi-kinase inhibitor |
Advanced hepatocellular carcinoma |
|
Lenvatinib |
Multi-kinase inhibitor |
First-line treatment for unresectable HCC |
Combination Treatment Strategies
Researchers are looking into combining treatments to make them more effective. This could help patients get better results from their treatments.
Combination regimens might mix immunotherapies with targeted agents, chemotherapy, or other treatments. Trials are underway to find the best combinations.
The future of treating liver and bile duct cancers looks bright. New treatments and combinations are being explored. This could lead to better outcomes for patients.
Prevention Strategies and Screening Recommendations
To prevent hepatobiliary cancer, we need to fight viral hepatitis with vaccines. We also need to live healthy and watch for signs of cancer. By doing these things, we can lower our chances of getting this disease.
Vaccination and Viral Hepatitis Control
Getting vaccinated against hepatitis B is key to stopping hepatobiliary cancer. The vaccine helps fight the hepatitis B virus. This virus is a big risk for liver cancer.
The Centers for Disease Control and Prevention (CDC) says, “Hepatitis B vaccine is recommended for all infants at birth, for children and adolescents younger than 19 years who have not been vaccinated, and for adults at risk for HBV infection.”
|
Vaccination Strategy |
Target Population |
Expected Outcome |
|---|---|---|
|
Hepatitis B vaccination at birth |
All newborns |
Reduced HBV infection rates |
|
Catch-up vaccination |
Unvaccinated children and adolescents |
Increased immunity against HBV |
|
Adult vaccination |
Adults at risk for HBV infection |
Prevention of HBV-related liver disease |
Lifestyle Modifications and Risk Reduction
Changing our lifestyle can help prevent hepatobiliary cancers. We should keep a healthy weight, drink less alcohol, and not smoke. These steps are very important.
- Keeping a healthy weight helps avoid non-alcoholic steatohepatitis (NASH), a risk for liver cancer.
- Drinking less alcohol helps prevent liver disease, which can lead to liver cancer.
- Not smoking lowers the risk of many cancers, including those in the liver.
Surveillance in High-Risk Populations
People at high risk for liver cancer should get checked regularly. This includes those with chronic HBV or HCV, cirrhosis, or a family history of liver cancer.
“Surveillance for HCC in high-risk populations can improve early detection and treatment outcomes.”
Checking for liver cancer usually means getting ultrasound scans and blood tests for alpha-fetoprotein (AFP). How often you need these tests depends on your risk and the doctor’s advice.
Conclusion
Hepatobiliary cancers, like hepatocellular carcinoma and intrahepatic cholangiocarcinoma, are big health worries worldwide. It’s key to understand these cancers well to find good ways to prevent and treat them.
The spread of these cancers varies around the globe. Some places have more cases because of viral hepatitis and drinking too much alcohol. In the U.S., liver cancer cases and deaths are going up. This shows we really need to act fast.
New ways to find and understand these cancers have helped a lot. We can now use imaging and lab tests to spot and figure out how serious they are. Treatments range from surgery and liver transplants to medicines that target the cancer.
Research is finding out more about what causes these cancers. New treatments like immunotherapy and targeted medicines might help patients more. By working on prevention, like vaccines and healthy living, and finding cancers early, we can lessen the impact of these diseases. This will help those who have them live better lives.
FAQ
What is hepatobiliary cancer?
Hepatobiliary cancer is a type of cancer that affects the liver, bile ducts, and gallbladder. It includes hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (iCCA).
What are the primary risk factors for developing hepatobiliary cancer?
Main risk factors are viral hepatitis (HBV and HCV), drinking too much alcohol, non-alcoholic steatohepatitis (NASH), and metabolic syndrome.
How is hepatobiliary cancer diagnosed?
Doctors use advanced imaging, lab tests, tumor markers, and biopsies to diagnose it. They examine the tissue under a microscope.
What are the common symptoms of hepatobiliary cancer?
Symptoms include pain in the abdomen, losing weight, jaundice, and feeling very tired. Early signs can be hard to spot.
What are the treatment options for hepatobiliary cancer?
Treatments include surgery, local treatments, and medicines that target cancer cells. A team of doctors usually works together to treat it.
Can hepatobiliary cancer be prevented?
Yes, you can prevent it by getting vaccinated against viral hepatitis, making healthy lifestyle choices, and getting regular check-ups if you’re at high risk.
What is the role of immunotherapy in treating hepatobiliary cancer?
Immunotherapy uses your immune system to fight cancer. It’s a new approach being studied for treating hepatobiliary cancers.
How does the BCLC staging system impact treatment decisions for HCC?
The BCLC staging system helps doctors choose the best treatment for HCC. It looks at the tumor, liver function, and how well the patient can handle treatment.
What is the significance of molecular targeted agents in hepatobiliary cancer treatment?
Molecular targeted agents are a new hope in treating hepatobiliary cancers. They target specific genes or pathways in cancer cells to slow their growth.
Are there any specific screening recommendations for high-risk populations?
Yes, people with chronic viral hepatitis, cirrhosis, or other high-risk conditions should get regular check-ups. This helps catch cancer early.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11374351/[1





