Pancreatic cancer is a big health issue. Knowing when most people get it is key to catching it early. Most pancreatic cancer cases happen to people 55 and older.
But, we’re seeing more cases in younger people too. Looking into how age affects pancreatic cancer risk factors helps us understand this disease better. Understanding when most people are diagnosed is crucial for improving treatment outcomes.
Key Takeaways
- Most people are diagnosed with pancreatic cancer at an older age.
- The majority of cases occur in individuals aged 55 and older.
- There is a concerning increase in pancreatic cancer cases among younger age groups.
- Understanding age distribution is key for early detection and prevention.
- Age is a big risk factor for pancreatic cancer.
Understanding Pancreatic Cancer

Pancreatic cancer is a serious disease with a high death rate worldwide. It’s a complex issue that needs a deep understanding to manage it well.
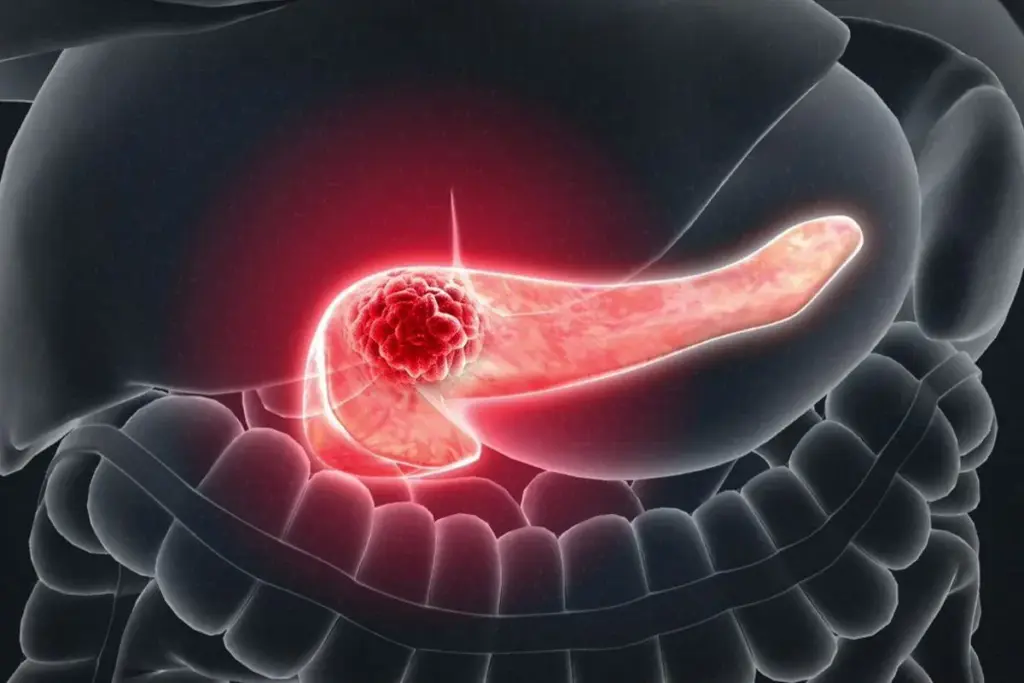
What is Pancreatic Cancer?
Pancreatic cancer starts in the pancreas, a key organ for digestion and blood sugar control. It’s caused by abnormal cells growing out of control in the pancreas. These cells can form tumors, some of which are harmless, but others are dangerous because they can spread to other parts of the body.
Types of Pancreatic Cancer
There are many types of pancreatic cancer, each with its own traits. The main ones are:
- Pancreatic adenocarcinoma
- Pancreatic neuroendocrine tumors (PNETs)
- Pancreatic squamous cell carcinoma
- Other rare types, such as acinar cell carcinoma and pancreatoblastoma
The variety of types shows how complex pancreatic cancer is. This complexity means we need different ways to diagnose and treat it.
Pancreatic Adenocarcinoma: The Most Common Type
Pancreatic adenocarcinoma is the most common type of pancreatic cancer. It starts in the glandular cells of the pancreas. The reasons for pancreatic adenocarcinoma are many, including genetics, environment, and lifestyle. Knowing these causes helps us prevent and catch it early.
Age Distribution of Pancreatic Cancer

It’s important to know how age affects pancreatic cancer. This helps us find risk factors and create better screening plans. Pancreatic cancer primarily affects older adults, making age a significant risk factor.
Median Age at Diagnosis
The median age for pancreatic cancer diagnosis is about 70 years. This means half of patients are diagnosed at or before 70, and the other half after. The prevalence of the disease increases with age, primarily impacting older individuals.
Incidence Rates by Age Group
How often pancreatic cancer happens changes with age. It’s much rarer in younger people, but starts to rise sharply at 55. Here are some incidence rates by age:
- Under 45: Less than 1% of cases
- 45-54: Approximately 10% of cases
- 55-64: Around 25% of cases
- 65-74: About 30% of cases
- 75 and older: Approximately 35% of cases
This shows most pancreatic cancer cases are in people 55 and older.
The 55+ Age Group: Highest Risk Population
People 55 and older face the highest risk of pancreatic cancer. As we get older, our risk goes up because of genetics and environment. So, knowing the age distribution helps target screening and prevention efforts.
Key statistics for this age group include:
- Increased incidence rates
- Higher proportion of diagnosed cases
- Greater need for targeted screening
By focusing on this age group, healthcare can better use resources. They can also work on improving early detection and treatment.
Current Trends in Pancreatic Cancer Diagnosis
Pancreatic cancer rates are changing, with more cases in younger people. This shift makes us look closer at why this is happening.
Rising Incidence in Younger Adults
Young adults, 15 to 34 years old, are seeing more pancreatic cancer. This is surprising because this disease used to mainly affect older people.
Annual Percentage Change in Young Adults
The number of pancreatic cancer cases in young adults is growing fast. It’s up by 4.35% each year. This rapid increase is a big worry, pointing to the need for better ways to find cancer early.
Annual Percentage Change in Older Adults
Adults over 55 are also getting pancreatic cancer more often. Their rate is 1.74% each year. While not as high as in younger adults, it’s a big issue because there are more people in this age group.
Key Trends:
- Increasing incidence among younger adults (15-34 years)
- 4.35% annual percentage change in young adults
- 1.74% annual percentage change in adults over 55
These trends show we need a broad approach to fight pancreatic cancer. We must focus on both the growing number of cases in young adults and the ongoing problem in older adults. This way, we can find better ways to prevent and catch cancer early.
What Causes Pancreatic Cancer
Understanding pancreatic cancer involves looking at genetics, environment, and lifestyle. Knowing these factors helps us find ways to prevent and detect cancer early.
Genetic Factors
Genetic mutations are key in pancreatic cancer. Certain genetic syndromes, like BRCA2 and Lynch syndrome, raise the risk. Also, KRAS gene mutations are common in pancreatic tumors.
Family history matters too. If you have a first-degree relative with pancreatic cancer, you’re at higher risk. We suggest genetic counseling and testing for those with a strong family history.
Environmental Triggers
Some environmental toxins and chemicals raise pancreatic cancer risk. For example, pesticides and heavy metals are linked to higher risk. People working in chemical processing jobs may also face increased risk due to their work environment.
Lifestyle Contributors
Lifestyle choices also play a part in pancreatic cancer risk. Smoking significantly increases risk, more so than for non-smokers. Being overweight and eating too much processed meat and not enough vegetables and fruits also raises risk.
Knowing these lifestyle factors helps us prevent cancer. We advise keeping a healthy weight, quitting smoking, and eating a diet full of fruits, vegetables, and whole grains to lower risk.
Risk Factors for Developing Pancreatic Cancer
Knowing the risk factors for pancreatic cancer is key to preventing and catching it early. This cancer, like many others, is shaped by genetics, environment, and lifestyle. By knowing these factors, we can work on preventing and managing it.
Modifiable Risk Factors
Modifiable risk factors are things we can change. For pancreatic cancer, some important ones include:
- Smoking: Smoking greatly increases the risk of pancreatic cancer. It’s thought to cause 20-30% of cases.
- Obesity: Being overweight or obese raises the risk of pancreatic cancer.
- Diet: Eating a lot of red and processed meats might increase risk. But, a diet full of fruits, veggies, and whole grains might help.
- Physical Activity: Staying active can lower the risk of pancreatic cancer.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. For pancreatic cancer, these include:
- Age: The risk goes up with age, with most cases in people over 65.
- Family History: Having a family history of pancreatic cancer, like in first-degree relatives, raises the risk.
- Genetic Mutations: Certain genetic changes, like in BRCA2, PALB2, and Lynch syndrome genes, also increase the risk.
Age as a Primary Risk Factor
Age is a big risk factor for pancreatic cancer. The risk jumps up after 50, with most cases in 65-74-year-olds. As more people live longer, we expect to see more cases.
It’s vital to understand these risk factors for better prevention and early detection. While some risks can’t be changed, managing the ones we can might lower pancreatic cancer rates.
The Hereditary Component of Pancreatic Cancer
It’s important to know about the hereditary aspects of pancreatic cancer. This knowledge helps identify those at higher risk. Pancreatic cancer, like many cancers, can be influenced by genetic factors passed down in families.
Genetic Mutations Associated with Pancreatic Cancer
Certain genetic mutations can greatly increase the risk of pancreatic cancer. These mutations can be inherited or occur on their own. Some well-known genetic mutations linked to pancreatic cancer include:
- BRCA2: Mutations in the BRCA2 gene raise the risk of pancreatic, breast, and ovarian cancers.
- STK11: This mutation is linked to Peutz-Jeghers syndrome, significantly increasing the risk of various cancers, including pancreatic cancer.
- PRSS1: Mutations in this gene are associated with hereditary pancreatitis, which can increase the risk of pancreatic cancer.
Family History Implications
A family history of pancreatic cancer is a significant risk factor. Those with a first-degree relative (parent, sibling, or child) diagnosed with pancreatic cancer are at higher risk. The risk increases if multiple family members have been diagnosed.
|
Family History |
Relative Risk |
|---|---|
|
No family history |
1.0 |
|
One first-degree relative with pancreatic cancer |
1.8-2.4 |
|
Two or more first-degree relatives with pancreatic cancer |
6.4-9.0 |
Genetic Testing and Counseling
For those with a significant family history of pancreatic cancer, genetic testing and counseling are invaluable. These services help identify genetic mutations and assess the risk of developing pancreatic cancer. Counseling also provides support and guidance on preventive measures and surveillance strategies.
We recommend that individuals with a concerning family history consult with a healthcare professional or a genetic counselor. Discussing their risks and the benefits of genetic testing can be very helpful.
Pancreatic Cancer in Different Demographics
Understanding pancreatic cancer in different groups is key to fighting it. We look at how demographics affect who gets the disease and how well they do. This helps us make treatments that fit each group’s needs.
Gender Differences
Studies show men are more likely to get pancreatic cancer than women. It’s thought that lifestyle, genes, and hormones play a part in this difference. For example, some genetic changes linked to the disease are more common in men.
Racial and Ethnic Variations
There are big differences in who gets pancreatic cancer based on race and ethnicity. African Americans face a higher risk than many other groups in the U.S. This is likely due to genetics, environment, and social factors. Knowing these differences helps us create better prevention plans.
Geographical Distribution in the United States
In the U.S., where you live can affect your risk of pancreatic cancer. Places with more smokers, obese people, and other risk factors see more cases. This shows why local health efforts are so important.
Looking at pancreatic cancer in different groups helps us understand it better. This knowledge is vital for making treatments that really work for everyone.
Early Detection Challenges
Finding pancreatic cancer early is a big challenge in medicine. This cancer often doesn’t show symptoms until it’s too late. We’ll look at why it’s hard to catch early, who should get screened, and new tech that might help.
Why Pancreatic Cancer Is Often Diagnosed Late
Pancreatic cancer is hard to spot early because its symptoms are vague. The pancreas is deep inside the body. Tumors can grow big before they cause noticeable problems.
Late Diagnosis Factors:
- Non-specific symptoms
- Location of the pancreas
- Lack of effective screening tests for the general population
Screening Recommendations by Age Group
Screening for pancreatic cancer isn’t common for everyone. But, some people at high risk might need it.
|
Age Group |
Screening Recommendations |
|---|---|
|
40-49 years |
Those with a strong family history or genetic risk should start screening early. |
|
50-59 years |
High-risk folks should get checked regularly with tests like endoscopic ultrasound (EUS) or MRI. |
|
60+ years |
Keep screening for those at high risk, with how often to check decided by their doctor. |
Emerging Detection Technologies
New tech is promising for catching pancreatic cancer early.
Some of these include:
- Liquid biopsies to find tumor DNA in blood
- Advanced imaging like MRI and PET scans
- AI to analyze images and health data
Survival Rates and Prognosis by Age
Knowing survival rates and prognosis is key for those with pancreatic cancer. The outlook for pancreatic cancer patients is tough. This is because it’s often diagnosed late and is aggressive. Yet, survival chances can change a lot based on age and the type of cancer.
Overall Five-Year Survival Rate
The five-year survival rate for pancreatic cancer is about 13%. This means 13% of patients live at least five years after being diagnosed. It’s a key number for understanding what to expect after diagnosis.
Pancreatic Adenocarcinoma’s Five-Year Survival Rate
Pancreatic adenocarcinoma, the most common pancreatic cancer, has a five-year survival rate of about 8%. This type is very aggressive and often found late. This makes its survival rate lower than the overall pancreatic cancer average.
How Age Affects Treatment Outcomes
Age is a big factor in how well pancreatic cancer patients do. Younger patients usually have better survival rates. They often have fewer health problems and respond better to treatments. Older patients, on the other hand, may face more challenges due to age-related health issues.
Age is just one factor that affects treatment outcomes. Other important factors include the cancer’s stage, type, and the patient’s overall health. Knowing these helps doctors create treatment plans that fit each patient’s needs. This can help improve their chances of doing well.
Treatment Approaches Across Age Groups
Age is key in treating pancreatic cancer. It affects the treatment choice and how well the patient does. We need to look at how age changes how treatments work and how well they are tolerated.
Standard Treatment Protocols
For pancreatic cancer, treatments usually include surgery, chemotherapy, and radiation. The goal is to remove the tumor and then kill any left-over cancer cells. Chemotherapy is often used first to make the tumor smaller.
When the cancer is advanced, the focus is on making the patient comfortable. Palliative chemotherapy and other treatments help manage pain and symptoms.
Age-Specific Treatment Considerations
Older adults face unique challenges in treatment. Their health and other conditions must be considered. They might need less chemotherapy or different treatments because of side effects.
Younger patients can usually handle more aggressive treatments. Their plans include new therapies and aim to reduce long-term side effects.
Multidisciplinary Care Approaches
Treating pancreatic cancer involves a team of experts. This team includes surgeons, oncologists, and more. They work together to create a treatment plan that fits the patient’s needs.
Considering the patient’s age and health, we can offer better care. This approach improves outcomes and quality of life during treatment.
Prevention Strategies for Pancreatic Cancer
Preventing pancreatic cancer involves lifestyle changes, health screenings, and managing risk factors. These steps can lower your chance of getting pancreatic cancer.
Lifestyle Modifications
Changing your lifestyle can greatly reduce pancreatic cancer risk. Here are some important changes:
- Dietary Changes: Eat more fruits, vegetables, and whole grains to help lower risk.
- Physical Activity: Regular exercise can also reduce your risk.
- Smoking Cessation: Quitting smoking is key, as it’s a big risk factor.
- Maintaining a Healthy Weight: Staying at a healthy weight through diet and exercise is important.
Regular Health Screenings
Regular health checks are key for early detection and prevention. While there’s no specific test for pancreatic cancer, some people may benefit from:
- Genetic Testing: If you have a family history or genetic risk.
- Imaging Tests: CT scans or MRI can spot abnormalities.
Talking to your healthcare provider about screenings can help find the right approach.
Managing Known Risk Factors
If you have known risk factors, managing them is critical. This includes:
- Diabetes Management: Proper diabetes care can lower your risk.
- Family History Awareness: Knowing your family history and talking to your doctor.
- Genetic Counseling: If you have a genetic risk.
By managing these risk factors, you can lower your chance of getting pancreatic cancer.
Future Projections and Research Directions
Looking ahead, pancreatic cancer will remain a big health issue worldwide. It deeply affects patients and their families. So, it’s key to know what the future holds and what research is needed.
Projected 67,440 New Cases in 2025
Experts predict 67,440 new pancreatic cancer cases by 2025. This rise shows we need more research on causes and better treatments. More cases mean we must invest in pancreatic cancer research.
“The growing burden of pancreatic cancer needs a full approach,” says a top expert. “We must keep funding research and aim to better treat patients.”
The 0.9% Annual Increase From 2013
From 2013 to now, pancreatic cancer cases have gone up by 0.9% each year. This shows pancreatic cancer is getting more common. We need better awareness and early detection.
Emerging Research and Possible Breakthroughs
New research in pancreatic cancer is looking at new treatments and early detection markers. Breakthroughs could greatly help patients live longer. Genetic testing and counseling are also getting better, helping those with a family history.
Some exciting research areas include:
- Studying genetics in pancreatic cancer
- Exploring new treatments like immunotherapy
- Working on better early detection with biomarkers
As we go forward, more research funding is vital. Together, we can better understand and treat pancreatic cancer.
Conclusion
Understanding pancreatic cancer is key to catching it early and treating it well. We’ve looked at how age, risk factors, and prevention play a role. Most cases happen in people over 55, with rates going up a lot in this age.
A detailed look at pancreatic cancer shows why it’s important to know about risk factors. These include genetic changes, lifestyle choices, and environmental causes. Knowing these can help people prevent and catch it early.
In summary, pancreatic cancer is a big health issue, mainly for older adults. By putting together what we’ve learned, we can grasp the disease’s complexity. This understanding drives the need for more research into treatments and ways to prevent it.
FAQ
What is the most common age group for pancreatic cancer diagnosis?
Most cases of pancreatic cancer happen to people aged 55 and older.
What is pancreatic adenocarcinoma?
Pancreatic adenocarcinoma is the most common pancreatic cancer type. It makes up most cases.
Is pancreatic cancer hereditary?
Yes, some genetic mutations and family history can raise your risk of pancreatic cancer.
What are the risk factors for developing pancreatic cancer?
Risk factors include age, genetics, environmental factors, lifestyle, and family history.
Can pancreatic cancer be prevented?
There’s no sure way to prevent it. But managing risks, making lifestyle changes, and getting regular check-ups can help lower your risk.
How does age affect the treatment outcomes for pancreatic cancer?
Age can affect treatment results. Getting treatment early is key to better outcomes.
What are the current trends in pancreatic cancer diagnosis?
There’s a growing trend of pancreatic cancer in younger adults. The number of cases is going up every year.
What are the symptoms of pancreatic cancer?
The article doesn’t directly answer this. But knowing the causes, risks, and age groups can help spot symptoms in those at higher risk.
How common is pancreatic cancer?
Pancreatic cancer is a big health issue. It’s expected to increase, with 67,440 new cases in 2025.
What are the treatment approaches for pancreatic cancer?
Treatments include standard methods, age-specific plans, and team care.
Can genetic testing help identify individuals at higher risk for pancreatic cancer?
Yes, genetic testing and counseling can find people with genetic mutations linked to pancreatic cancer.
Are there any emerging detection technologies for pancreatic cancer?
Yes, new detection technologies could improve early detection rates.
What is the overall five-year survival rate for pancreatic cancer?
The five-year survival rate is about 13%. Pancreatic adenocarcinoma’s rate is around 8%.
How does pancreatic cancer incidence vary across different demographics?
Pancreatic cancer rates differ by gender, race, ethnicity, and location.
Reference List
- “Pancreatic Cancer Mortality Trends”
- “Pancreatic Cancer Diagnoses and Mortality Rates Climb”
- “Study Finds Increased Rates of Pancreatic and Colon Cancer Among Young People”
- “SEER Cancer Stat Facts: Pancreas Cancer”
- “Key Statistics About Pancreatic Cancer”
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK518996/






