Last Updated on November 27, 2025 by Bilal Hasdemir
Robotic urologic surgery has transformed how prostate cancer is treated. This advanced approach means less pain, less blood loss, and a much faster recovery from prostate surgery compared to traditional methods.
Patients undergoing robotic prostatectomy benefit from shorter hospital stays and quicker return to daily activities, which makes recovery from prostate surgery smoother and less stressful. Understanding the advantages of robotic urologic surgery can help patients prepare mentally and physically for recovery from prostate surgery.
Doctors emphasize that following post-operative instructions and attending follow-up visits are key to successful recovery from prostate surgery. With robotic techniques, patients often experience less discomfort and faster healing, making this approach a preferred option for many men.
Key Takeaways
- Robotic urologic surgery is a minimally invasive approach for treating urological conditions.
- It enables surgeons to perform precise operations with less pain and blood loss.
- Robotic-assisted surgery leads to quicker recovery times.
- Understanding the recovery process is key for patients undergoing prostate surgery.
- Robotic prostatectomy is a top choice for prostate removal.
Technology for better control and vision. This method is more precise and less invasive than old surgery techniques.
Definition and Basic Concepts
It helps surgeons do complex urologic procedures with more skill. The system has a 3D camera and endo-wrist instruments that move like a human hand.
The main idea is to make surgery less invasive but more precise. The robotic system gives a clear, 3D view of the area being operated on. It also has instruments that can bend and rotate, something human hands can’t do.
Historical Development of Robotic Surgery in Urology
Better results for patients. For example, robotic-assisted laparoscopic prostatectomy (RALP) is now common. It reduces blood loss, pain, and recovery time.
The Evolution of Prostate Surgery Techniques
Prostate surgery has seen big changes, moving from open surgery to laparoscopic and robotic-assisted methods. These new techniques aim to improve patient results, cut down recovery times, and boost surgical accuracy.
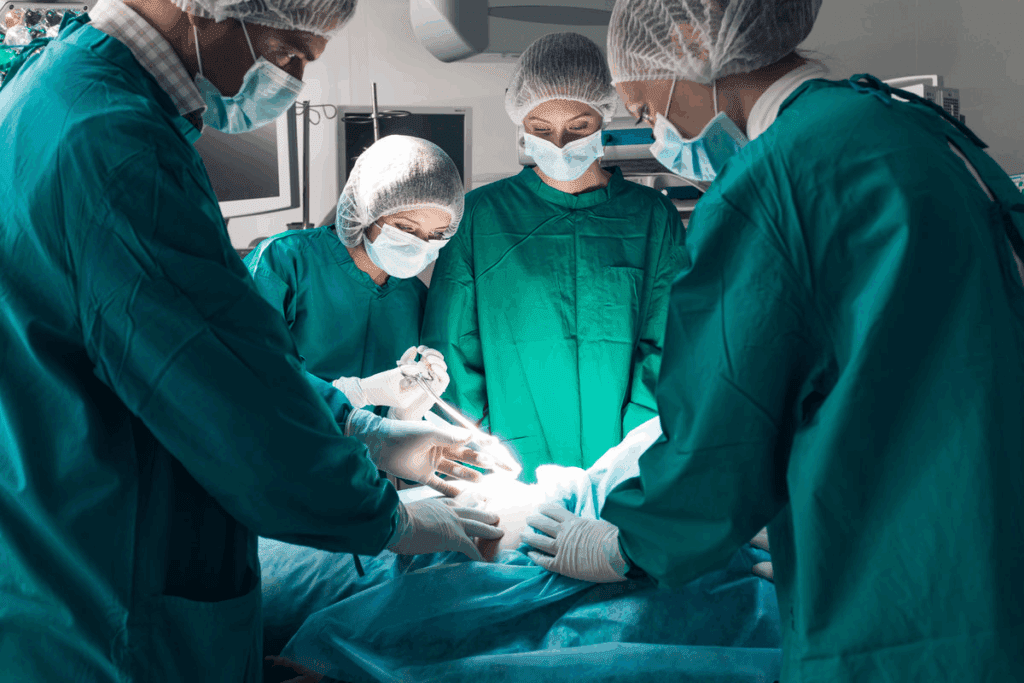
Traditional Open Prostatectomy
Open prostatectomy used to be the main way to operate on the prostate. It involves a big cut to reach the gland. This method can cause a lot of postoperative pain, longer hospital stays, and more risks.
Laparoscopic Approaches
Laparoscopic prostate surgery uses small cuts for instruments and a camera. It leads to less postoperative pain and faster healing than open surgery. But, it needs a lot of skill and takes time to learn.
Introduction of Robotic-Assisted Techniques
Robotic-assisted surgery in prostate operations is a big step forward. It brings the benefits of minimally invasive surgery with the chance for fewer problems and quicker healing.
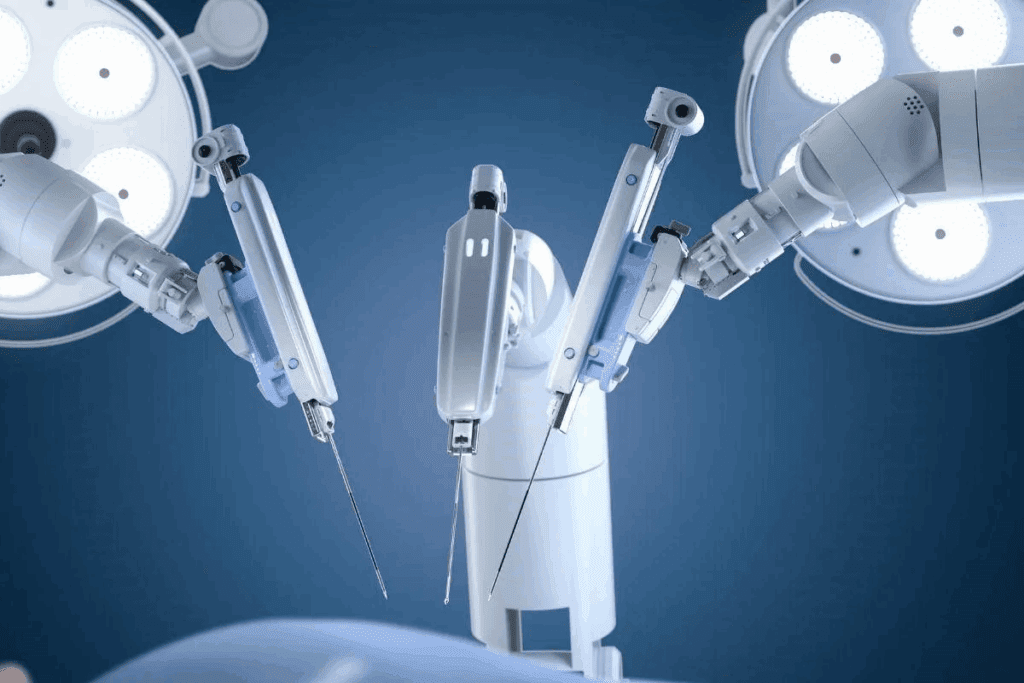
Components and Technology
The patient-side robotic cart has endo-wrist instruments that move like a human wrist. They can move more than traditional laparoscopic tools.
The image processing stack sends 3D high-definition images to the surgeon’s console. This tech, along with the enhanced endo-wrist dexterity, makes surgery more precise and less invasive.
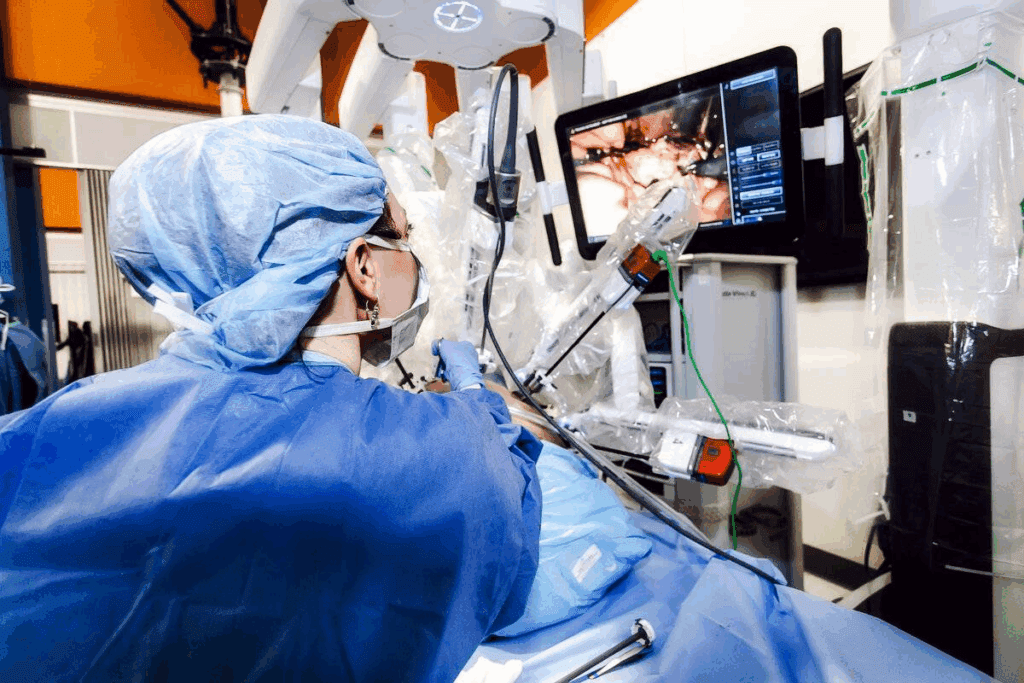
How the Surgeon Controls the Robot
The surgeon uses the console to control the Da Vinci robot. They sit comfortably and look through a 3D viewer. The console has hand controls and foot pedals for precise control.
The system’s motion scaling and tremor filtration features improve control. This makes movements smooth and precise.
- The surgeon’s hand movements are translated into precise movements of the robotic instruments.
- The system provides real-time feedback, improving the surgeon’s control over the instruments.
- The ergonomic design of the console reduces surgeon fatigue during long procedures.
Understanding how the Da Vinci Surgical System works shows why it’s a top choice for urologic surgery.
Robotic-assisted laparoscopic procedures are becoming more common in urology. They improve patient outcomes by being more precise and less invasive. This means doctors can do more complex surgeries with better results.
Robotic-Assisted Laparoscopic Prostatectomy (RALP)
Robotic-Assisted Laparoscopic Prostatectomy (RALP) is a top choice for prostate cancer treatment. It uses a robotic system for a clear view of the area being operated on. The benefits include:
- Less blood loss during surgery
- Reduced risk of complications
- Faster recovery times
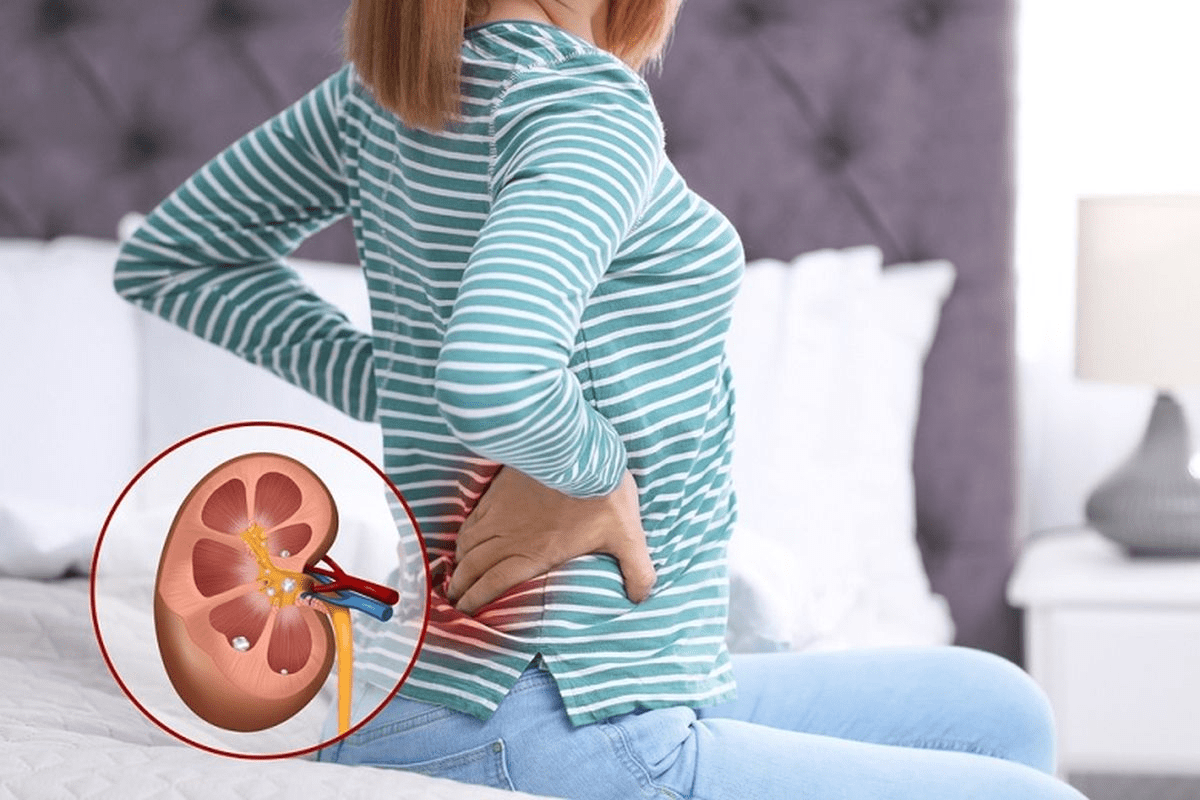
Other robotic surgeries include partial nephrectomy and ureteral reconstructive surgery. These use robotic systems for precision in treating kidney cancer and ureteral obstruction.
Partial Nephrectomy removes part of the kidney with cancer, saving the rest. It’s vital for kidney tumor patients.
Ureteral Reconstructive Surgery fixes damaged or blocked ureters. It ensures urine flows correctly from the kidneys to the bladder.
Robotic surgery is suggested for prostate and kidney cancer. The choice depends on cancer stage, patient health, and surgeon skill.
It leads to better results and quicker recovery.
In summary, robotic urologic procedures are a big step forward. They offer patients less invasive options with faster recovery and fewer complications.
Benefits of Robotic Prostatectomy
Robotic prostatectomy offers many benefits. These include better surgical precision, less blood loss, and quicker recovery times. This method is more precise than traditional surgery, leading to better results for patients.
Enhanced Surgical Precision
Robotic prostatectomy brings enhanced surgical precision thanks to advanced technology. The robotic arms can make very precise movements. This allows for more accurate removal of the prostate gland.
Reduced Blood Loss and Tissue Trauma
Robotic prostatectomy also means reduced blood loss and tissue trauma. The procedure is minimally invasive, leading to less bleeding and tissue damage. UC Davis Health found that patients have less pain and recover faster.
Faster Recovery Times
Robotic prostatectomy leads to faster recovery times. Its minimally invasive nature means less pain and quicker return to normal activities. A study showed robotic-assisted prostatectomy results in shorter hospital stays and faster recovery.
| Benefits | Robotic Prostatectomy | Traditional Prostatectomy |
| Surgical Precision | High | Moderate |
| Blood Loss | Minimal | Significant |
| Recovery Time | Faster | Longer |
Potential Risks and Complications
Robotic prostatectomy, like any surgery, has risks and complications. It’s important to know about them and talk to a doctor. Robotic surgery has many benefits, but it’s not risk-free.
Common Side Effects
Side effects of robotic prostatectomy include urinary incontinence and erectile dysfunction. These issues are usually temporary. Urinary incontinence can be mild or severe. Erectile dysfunction can also vary, depending on several factors.
| Side Effect | Description | Typical Recovery Time |
| Urinary Incontinence | Loss of bladder control ranging from mild leakage | Several months |
| Erectile Dysfunction | Difficulty achieving or maintaining an erection | Variable, up to a year or more |
Rare but Serious Complications
Though rare, serious complications can happen. These include infection, bleeding, and damage to nearby organs. Infection is treated with antibiotics, but sometimes it needs hospital care. Bleeding might require blood transfusions or more surgery. Damage to organs is rare but serious.
It’s key to understand these risks before deciding on robotic prostatectomy. Talking to your doctor about your specific risks is important.
Before robotic prostate surgery, it’s key to know what to do. Getting ready right can make surgery and recovery better.
Medical Evaluations and Tests
Patients need to go through detailed medical checks. These tests help find any health issues and make sure you’re ready for surgery.
- Cardiovascular assessment: This checks your heart health and spots any surgery risks.
- Blood tests: They look for infections, blood type, and more.
- Imaging tests: MRI or CT scans give clear pictures of your prostate and nearby areas.
These evaluations are essential for ensuring a smooth surgical experience.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before surgery can help. It can lower risks and help you heal faster.
- Stop smoking: Quitting smoking is a big help to avoid complications.
- Maintain a healthy diet: Eating well can boost your recovery.
- Exercise regularly: Some exercise can make you stronger and healthier.
Temple Health advises talking to your doctor about your lifestyle. They can give you advice tailored to you.
What to Expect the Day Before Surgery
The day before surgery is all about getting ready.
- Follow preoperative instructions: This includes fasting, bowel prep, and other doctor’s orders.
- Arrange for post-surgery care: Make sure someone can help with daily tasks and support you early on.
By following these steps, you can prepare well for robotic prostate surgery and recovery.
The Robotic Prostatectomy Procedure Step by Step
It’s important for patients to know about the robotic prostatectomy procedure. This surgery has many steps, from the start to the end.
Anesthesia and Initial Setup
The surgery starts with general anesthesia to keep the patient comfortable. The patient is then placed in a way that helps the surgeon access the prostate gland. The da Vinci Surgical System is set up, with its arms calibrated and ready.
The surgical team makes sure everything is ready. They check that the patient is prepared for the surgery. This setup is key for a successful surgery.
Surgical Approach and Technique
The surgeon uses the da Vinci Surgical System to do the surgery. They make small cuts and remove the prostate gland carefully. This system helps the surgeon be more precise.
The surgeon also tries to save important nerves and blood vessels. This is important for the patient’s urinary and sexual health after surgery. The robotic-assisted technique allows for a more detailed surgery than traditional methods.
Completion and Closure
After removing the prostate gland, the surgeon reconnects the bladder to the urethra. This is called the urethrovesical anastomosis. It’s a critical step for healing and urinary function.
After finishing the anastomosis, the team closes the incisions. The patient then goes to the recovery room for care. The whole robotic prostatectomy procedure needs a team of healthcare professionals for the best results.
How Long Does Robotic Prostate Surgery Take?
Average Duration of the Procedure
On average, robotic prostate surgery lasts between 2 to 4 hours. But, this can change based on the patient’s condition and the team’s skill.
Factors Affecting Surgical Time
| Factor | Impact on Surgical Time |
| Surgeon’s Experience | More experienced surgeons tend to complete the procedure more quickly. |
| Prostate Size | Larger prostates can increase surgical time due to the complexity of the procedure. |
| Patient’s Health | Patients with certain health conditions may require more time for preparation and surgery. |
Recovery From Prostate Surgery: The First Days
Knowing what to expect in the first days after robotic prostate surgery can make recovery easier. This initial period is key for a smooth recovery.
The exact time depends on health and surgery specifics.
Managing pain well is very important in the first days. Patients get a mix of medicines to help with pain and discomfort.
“The key to successful recovery is managing pain effectively and being proactive about post-operative care.”
Initial Mobility and Care
Moving around is encouraged to avoid problems like blood clots and to help healing. Patients start with short walks and then do more.
- Take short walks around the house
- Avoid strenuous activities
- Follow the healthcare team’s instructions for post-operative care
Catheter Management
A catheter is used to drain urine from the bladder during surgery. It stays in for about 1-2 weeks, as decided by the surgeon.
| Day | Catheter Status | Care Instructions |
| 1-2 | In place | Monitor for any signs of infection or blockage |
| 7-14 | Removed | Follow up with healthcare provider for removal |
Proper care of the catheter is vital to avoid infections and ensure a smooth recovery. Patients must follow their healthcare team’s specific instructions.
Recovery From Prostate Surgery: Weeks 1-4
Recovering from prostate surgery takes time and following certain guidelines. In the first four weeks, patients go through big changes. They need to get used to new routines.
Physical Limitations and Activity Guidelines
In the first weeks after surgery, Patients should avoid lifting heavy objects or engaging in strenuous activities during recovery. Temple Health recommends not lifting more than 10 pounds. They should also avoid activities that might strain the pelvic area.
Patients can start with short walks and light exercises as they get better. It’s important to follow a plan for activities to avoid problems and help with healing. They should listen to their body and rest when needed.
Managing Urinary Function
It’s also important to know about using a catheter after surgery. Knowing how to use it and when to look out for problems is essential.
Follow-up Appointments and Care
Follow-up appointments are very important. They let doctors check how you’re doing and answer any questions. They also help remove any catheters or stitches when it’s time.
Keeping a log of your recovery is helpful. Write down any changes, pain levels, and concerns. This information is very useful during your follow-up visits.
Long-Term Recovery and Rehabilitation
Recovery and rehabilitation are key after robotic prostate surgery. They help patients regain strength and manage side effects. This phase also improves their quality of life.
Sexual Function Recovery Timeline
Recovering sexual function after robotic prostatectomy takes time. Most patients start seeing improvements in 6 to 12 months. But, full recovery can take up to 2 years. Age, preoperative function, and the surgeon’s skill play a role.
Nerve-sparing techniques can help. They aim to keep nerves around the prostate intact. This might lower the risk of erectile dysfunction.
Continence Improvement Timeline
Urinary continence is also important after robotic prostatectomy. Most patients face some incontinence right after surgery. But, big improvements usually come in 3 to 6 months. It can take up to a year or more for full continence.
Kegel exercises are key for urinary continence recovery. They strengthen muscles that help control the bladder.
Physical Therapy and Pelvic Floor Exercises
Physical therapy, like pelvic floor rehabilitation, is vital. Pelvic floor exercises can boost both urinary continence and sexual function. Patients should start these exercises soon after surgery and keep going for months.
| Recovery Aspect | Typical Recovery Timeline | Influencing Factors |
| Sexual Function | 6-24 months | Age, preoperative erectile function, surgical technique |
| Urinary Continence | 3-12 months | Pelvic floor muscle strength, overall health |
Knowing the recovery process helps patients prepare. Following a rehabilitation plan, including physical therapy and pelvic floor exercises, can greatly improve outcomes.
Comparing Recovery: Robotic vs. Traditional Approaches
It’s important to know how robotic and traditional prostate surgery differ in recovery. The type of surgery affects not just the immediate healing but also long-term health and happiness.
Recovery Time Differences
Key differences in recovery time include:
- Shorter hospital stays
- Faster return to normal activities
- Less post-operative pain
| Recovery Aspect | Robotic-Assisted Surgery | Traditional Open Surgery |
| 1-2 days | 3-5 days | |
| Return to Normal Activities | 1-2 weeks | 4-6 weeks |
| Post-Operative Pain Level | Lower | Higher |
Quality of Life Outcomes
The type of surgery greatly affects life after prostate surgery. Robotic surgery, being precise and less invasive, leads to better life quality. Patients often have less urinary issues and better sex life than those with traditional surgery.
Studies have shown robotic systems’ advanced technology allows for more precise nerve-sparing. This results in better control over urination and sex life after surgery.
In conclusion, robotic surgery beats traditional methods in recovery time and life quality. As technology advances, these benefits will grow. Making the right choice about surgery is more important than ever.
Technological Advancements in Robotic Urology
Robotic technology is changing urologic surgery. New tech in robotic urology is making surgeries better and changing how they’re done.
Latest Innovations in Robotic Systems
New robotic systems are making surgeries more precise and skilled. Temple Health says these updates improve how surgeons see and do things. Enhanced visualization and improved dexterity are big wins.
“The future of surgery is in the hands of robotics, where precision and minimal invasiveness are redefining patient care.”
Impact on Surgical Outcomes and Recovery
These tech updates have greatly improved surgery results and recovery. Studies show patients have less blood loss, reduced pain, and faster recovery times with robotic surgery.
- Reduced hospital stay duration
- Minimal scarring
- Less postoperative pain
These gains come from robotic surgery’s precision and less invasiveness. So, patients can get back to their lives faster, improving their quality of life.
Robotic urologic surgery is growing fast, thanks to new tech and techniques. This field is promising for better patient care and life quality. As new ideas come up, treatments for urologic issues will get even better.
The Da Vinci Surgical System has been a big step forward. It brings more precision and less invasiveness. With robotic urology getting better, surgeons can give patients the best care. This means shorter recovery times and a better life quality.
It’s important for patients and doctors to keep up with robotic urology news. As this field expands, we’ll see even better results and care. The future of robotic urologic surgery looks bright, with exciting breakthroughs ahead.
FAQ
How long does robotic prostate surgery take?
Robotic prostate surgery usually takes 2-3 hours. But, it can take longer or shorter depending on the case and the surgeon.
What are the benefits of robotic prostatectomy?
Robotic prostatectomy offers many benefits. It gives better precision, less blood loss, and faster recovery. Patients also see better results.
What are the possible risks and complications of robotic prostatectomy?
There are risks and complications. These include problems like not being able to urinate or have an erection. Rare but serious issues like infection and bleeding can also happen.
How do I prepare for robotic prostate surgery?
To get ready, you’ll need medical checks and tests. You’ll also need to make lifestyle changes and follow your doctor’s instructions.
What can I expect during the recovery process after prostate surgery?
You might feel pain, discomfort, and have urinary issues at first. But, these problems usually get better with time and proper care.
How long does it take to recover from robotic prostate surgery?
Recovery times vary. Most people can get back to normal in 1-4 weeks. But, it can take months to fully recover.
What is the difference between robotic and traditional open prostatectomy?
Robotic surgery is less invasive. It leads to faster recovery, less pain, and less blood loss than traditional open surgery.
Will I experience urinary incontinence after robotic prostatectomy?
Yes, urinary incontinence is a possible side effect. But, most people see big improvements with exercises and physical therapy.
How will robotic prostatectomy affect my sexual function?
It can affect sexual function, but how much varies. Factors like age, health, and the surgeon’s skill play a role.
What are the latest advancements in robotic urology?
New advancements include better robotic systems. These offer more precision and better outcomes, making recovery faster.
Is robotic urologic surgery the future of prostate surgery?
Yes, it’s becoming more popular. It’s expected to keep improving patient outcomes and quality of life.
Reference
- Ko, Y. H. (2018). Functional recovery after radical prostatectomy for prostate cancer. Yeungnam University College of Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC6784702/