Last Updated on November 27, 2025 by Bilal Hasdemir

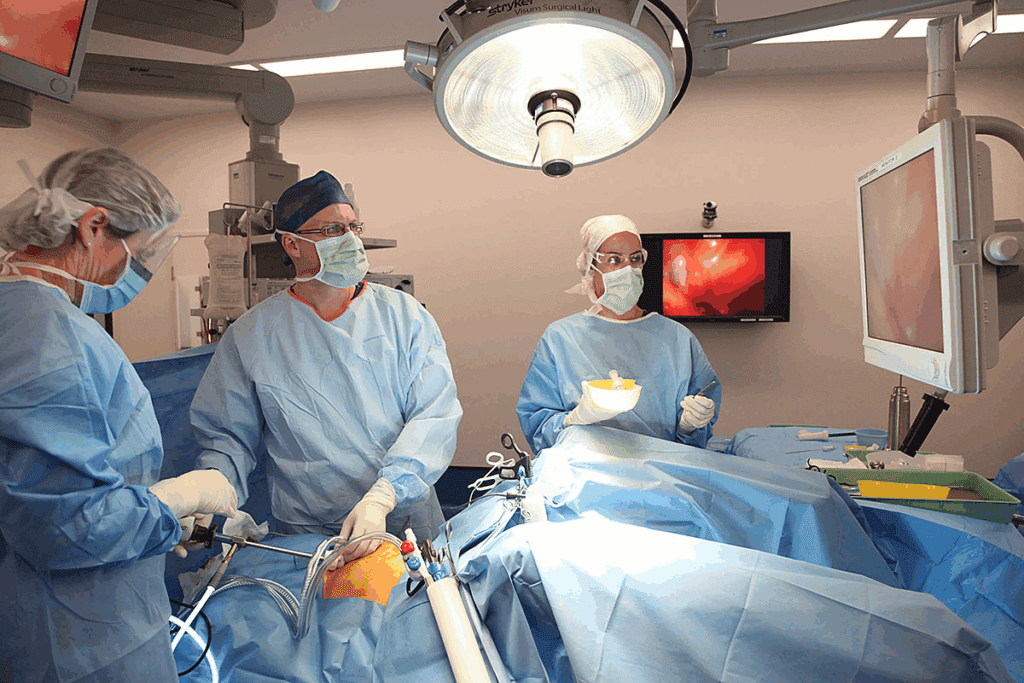
Nearly 600,000 hysterectomies are performed every year in the United States, making it one of the most common surgical procedures. With many types of hysterectomies available, patient safety is always a top priority. One common question is which method is the safest.
A laparoscopic hysterectomy is often considered a safe and effective option. Compared to traditional open surgery, laparoscopic hysterectomy involves smaller incisions, reduced blood loss, and faster recovery times. These benefits make it a preferred choice for many patients and surgeons.
However, the safest approach for each patient depends on individual health, medical history, and specific surgical needs. Consulting with your doctor helps determine whether a laparoscopic hysterectomy is the most suitable option.
By understanding the advantages of a laparoscopic hysterectomy, patients can make informed decisions and prepare for a smoother recovery and better overall outcomes.
Key Takeaways
- Knowing the different types of hysterectomy is key for patient safety.
- Laparoscopic hysterectomy has less risk and faster healing.
- What’s safest varies based on the patient’s health.
- Talking to a healthcare provider about options is crucial.
- Risks differ among various hysterectomy procedures.
Understanding Hysterectomy: Types and Approaches
When thinking about a hysterectomy, it’s key to know the different methods and their effects on health. A hysterectomy is a big surgery that removes the uterus. There are many things to think about when picking the right procedure.
What is a hysterectomy?
A hysterectomy is a surgery to take out the uterus. It’s often done for issues like uterine cancer, fibroids, and heavy bleeding. This surgery can change a woman’s health a lot.
Common reasons for hysterectomy
Hysterectomies are done for many reasons, including:
- Uterine cancer or other cancers affecting the uterus
- Fibroids or other growths in the uterus
- Heavy or irregular menstrual bleeding
- Endometriosis or other chronic pelvic pain conditions
- Uterine prolapse
The most common reason is fibroids. They can cause a lot of pain and health problems.
Different types of hysterectomy procedures
There are many types of hysterectomy surgeries, each with its own benefits and uses:
| Description | Indications | |
| Abdominal Hysterectomy | Removal of the uterus through an abdominal incision | Cancer, large fibroids, complex pelvic conditions |
| Vaginal Hysterectomy | Removal of the uterus through the vagina | Uterine prolapse, smaller fibroids, less complex conditions |
| Laparoscopic Hysterectomy | Minimally invasive removal of the uterus using laparoscopy | Endometriosis, smaller fibroids, desire for less recovery time |
| Robotic Hysterectomy | Minimally invasive removal of the uterus using robotic assistance | Complex conditions, precision required, less recovery time desired |
“The choice of hysterectomy procedure depends on various factors, including the patient’s overall health, the reason for the surgery, and the surgeon’s expertise.”
It’s important for patients to understand these options. This helps them make better choices about their care.
Abdominal Hysterectomy: The Traditional Approach

The abdominal hysterectomy is a common surgery to remove the uterus through the belly. It has been a key method in gynecology for years. It’s a simple way to treat many uterine problems.
How Abdominal Hysterectomy is Performed
The procedure begins with a surgeon making an incision in the abdominal wall to access the uterus. The steps can change based on the patient and surgeon. It usually means cutting the uterus from nearby tissues and taking it out through the belly.
Key Steps in Abdominal Hysterectomy:
- Making an abdominal incision to access the uterus
- Dissecting the uterus from surrounding tissues
- Removing the uterus through the incision
- Closing the incision with sutures or staples
Safety Profile and Risk Factors
Abdominal hysterectomy is generally safe but has risks like infections and blood clots. The safety depends on the patient’s health, the surgery’s reason, and the surgeon’s skill.
| Risk Factor | Description | Mitigation Strategy |
| Infection | Bacterial infection at the surgical site | Prophylactic antibiotics, proper wound care |
| Blood Clots | Formation of clots in the legs or lungs | Early mobilization, anticoagulant medication |
| Injury to Surrounding Organs | Damage to nearby organs during surgery | Precise surgical technique, experience |
Recovery Expectations
Recovery from an abdominal hysterectomy takes longer than other surgeries. Patients usually stay in the hospital for days. They might feel pain, which can be treated with medicine. Recovery can take weeks.
Knowing how to recover is key for patients. They should plan for home care, manage pain, and follow the surgeon’s advice.
Vaginal Hysterectomy: A Natural Opening Approach
Vaginal hysterectomy is a preferred choice for some patients. It has fewer risks and quicker recovery than other surgeries. This method removes the uterus through the vagina, avoiding external cuts.
Procedure Details and Technique
The procedure begins with a surgeon making an incision in the abdominal wall to access the uterus.
The technique needs skill to avoid problems.
This method has less pain and lower infection risk. It’s a good option for many.
Safety Considerations and Complication Rates
Vaginal hysterectomy is generally safe but carries risks. These include bleeding, infection, and damage to nearby organs. Yet, studies show it has fewer complications than abdominal hysterectomy.
| Complication | Vaginal Hysterectomy Rate | Abdominal Hysterectomy Rate |
| Bleeding | 2% | 5% |
| Infection | 1.5% | 3% |
| Injury to Surrounding Organs | 0.5% | 1% |
Ideal Candidates for Vaginal Hysterectomy
Women with a prolapsed uterus or specific gynecological issues are good candidates. The choice depends on the patient’s health and condition.
Recovery Process and Timeline
Recovery from vaginal hysterectomy is quicker than from abdominal surgery. Most women can resume normal activities in 4-6 weeks. Post-operative care includes pain management and follow-up appointments.
The minimally invasive nature of vaginal hysterectomy is appealing. It offers surgical precision and quick recovery.
Laparoscopic Hysterectomy: Minimally Invasive Option
Minimally invasive surgery has changed gynecology a lot. Laparoscopic hysterectomy is a big part of this change. It makes hysterectomies safer and more efficient than old methods.
How Laparoscopic Procedures Work
Laparoscopic hysterectomy uses a thin, lighted tube with a camera. This lets surgeons see the uterus and tissues around it. They make small cuts, which helps the body heal faster.
This method gives a clear view of the area being worked on. It’s great for patients with endometriosis or fibroids. It helps surgeons remove the uterus carefully.
Types of Laparoscopic Hysterectomies
There are a few types of laparoscopic hysterectomies:
- Total Laparoscopic Hysterectomy (TLH): The whole procedure is done through small cuts, and the uterus is removed through the vagina.
- Laparoscopic-Assisted Vaginal Hysterectomy (LAVH): This combines laparoscopic and vaginal methods. Some parts are done through small cuts, and others through the vagina.
- Laparoscopic Supracervical Hysterectomy (LSH): The uterus is removed through small cuts, but the cervix is left in place.
Safety Profile and Advantages
Laparoscopic hysterectomy has many benefits:
- It results in less blood loss and fewer blood transfusions.
- Patients often feel less pain and discomfort after surgery.
- They usually stay in the hospital for less time and recover faster.
- There are smaller cuts, which means less scarring.
This method is generally safer than open surgery. But, like any surgery, there are risks. Patients should talk to their doctor about these.
Recovery and Post-Operative Care
Recovery from laparoscopic hysterectomy is quicker than from open surgery. Patients can usually get back to normal in a few weeks. Care after surgery includes:
- Managing pain with medicine.
- Going to follow-up appointments to check on healing.
- Slowly increasing physical activity.
Knowing the benefits and risks of laparoscopic hysterectomy helps patients make good choices. It’s important to talk to a doctor to find the best option for each person.
Robotic Hysterectomy: Technology-Assisted Surgery
Robotic-assisted hysterectomy uses advanced technology for better results. It uses the da Vinci system for more precise surgery.
The da Vinci Surgical System Explained
The da Vinci system is a high-tech robot for complex surgeries. It has a surgeon’s console, a patient cart, and a 3D vision system. The surgeon’s console lets the doctor control the robotic tools with precision.
Key Features of the da Vinci System:
- High-definition 3D visualization
- Enhanced dexterity and precision
- Improved ergonomics for surgeons
- Reduced tremor and fatigue
Benefits and Limitations of Robotic Assistance
Robotic hysterectomy has many benefits. It reduces blood loss, pain, and hospital stays. But, it also has risks like equipment failure and the need for special training.
The benefits of robotic assistance include:
- Enhanced surgical precision
- Improved patient outcomes
- Reduced recovery time
Safety Considerations for Robotic Procedures
Robotic hysterectomy has safety concerns. These include equipment failure, surgical risks, and the need for skilled surgeons.
| Safety Aspect | Robotic Hysterectomy | Traditional Laparoscopic |
| Equipment Failure | Low | Minimal |
| Surgical Complications | Comparable | Comparable |
| Surgeon Training | Specialized | Standard |
Comparing Robotic vs. Traditional Laparoscopic Approaches
Robotic and traditional laparoscopic hysterectomies differ in several ways. These include precision, recovery time, and cost.
The choice between robotic and traditional laparoscopic surgery depends on many factors. These include the patient’s anatomy, the surgeon’s skill, and the specific needs of the procedure.
Comparing Safety Profiles: Complication Rates
When thinking about a hysterectomy, knowing the possible complications is key. Each type of hysterectomy has its own risks and rates of complications. These depend on the surgery method, the patient’s health, and why the surgery is needed.
Immediate Surgical Complications by Procedure Type
Right after or soon after surgery, some problems can happen. These might be bleeding, damage to nearby organs, or bad reactions to anesthesia. The rates of these issues differ a lot between different hysterectomy methods.
Abdominal hysterectomy often has more immediate problems than vaginal or laparoscopic hysterectomies. This is because abdominal surgery is more invasive. It needs a bigger cut and can cause more damage to tissues.
Post-operative Infection Rates
Infections after surgery are a big worry. The chance of getting an infection varies with the type of hysterectomy. Abdominal hysterectomies usually have a higher risk of infection than less invasive ones.
- Laparoscopic hysterectomies have lower infection rates because they use smaller cuts and cause less tissue damage.
- Vaginal hysterectomies also have a lower risk of infection since they don’t involve making an incision in the abdomen.
Long-term Complications
Long-term problems can include pelvic organ prolapse, urinary incontinence, and adhesions. The risk of these issues depends on the hysterectomy type and the patient’s health.
| Hysterectomy Type | Immediate Complication Rate | Post-operative Infection Rate | Long-term Complication Rate |
| Abdominal | High | Moderate to High | Moderate |
| Vaginal | Low to Moderate | Low | Low to Moderate |
| Laparoscopic | Low to Moderate | Low | Low |
| Robotic | Low | Low | Low |
Mortality Rates Across Different Approaches
Mortality rates for hysterectomy are usually low but can change based on the procedure and patient health. Studies show that abdominal procedures have a higher mortality rate than less invasive methods.
It’s important for patients and doctors to know these safety profiles and complication rates. This helps make the best choice for each person’s situation.
Recovery Time and Hospital Stay Comparison
The type of hysterectomy greatly affects how long you stay in the hospital and how long it takes to recover. Knowing these differences helps patients make better choices about their care.
Hospital Stay Duration by Procedure Type
The length of your hospital stay changes based on the type of hysterectomy. Minimally invasive procedures usually mean shorter stays.
- Abdominal hysterectomy: typically 2-4 days
- Vaginal hysterectomy: often 1-2 days
- Laparoscopic hysterectomy: usually 1-2 days
- Robotic hysterectomy: often same-day discharge or 1 day
Return to Normal Activities Timeline
Recovery times before getting back to normal activities also vary. Minimally invasive surgeries tend to have shorter recovery periods.
- Abdominal hysterectomy: 6-8 weeks
- Vaginal hysterectomy: 4-6 weeks
- Laparoscopic hysterectomy: 2-4 weeks
- Robotic hysterectomy: 2-4 weeks
Pain Management Differences
Pain management is key during recovery. The amount of pain and need for pain meds differ by surgery type.
- Abdominal hysterectomy: often needs more pain meds
- Minimally invasive procedures: usually less pain and fewer meds needed
Impact on Quality of Life During Recovery
The recovery period’s impact on quality of life is significant. Being able to do daily tasks, manage pain, and go back to work affects well-being.
Those who have minimally invasive hysterectomies often recover faster. They also report a better quality of life during recovery.
Special Considerations for High-Risk Patients
High-risk patients need special care during hysterectomy to avoid complications. Health issues like obesity and chronic diseases can affect the safety of the procedure.
Obesity and Hysterectomy Safety
Obesity can make hysterectomy more complicated. Obese patients face higher risks of infection and blood clots. Surgeons must adjust their methods to handle these extra challenges.
Advanced Age Considerations
Older patients may have more health issues, making surgery riskier. It’s key to check their health before surgery. Preoperative evaluation is critical to reduce risks.
Previous Abdominal Surgeries
Patients with past abdominal surgeries may have adhesions or complications. Surgical planning must consider these to achieve the best results.
Chronic Health Conditions and Surgical Risk
Chronic conditions like diabetes and hypertension raise the risk of complications. Managing these before surgery is crucial. Multidisciplinary care from various specialists can improve outcomes.
Healthcare providers can make hysterectomy safer for high-risk patients by assessing risks and adjusting the approach. This helps improve outcomes.
The Role of Surgeon Experience in Safety Outcomes
The safety and success of hysterectomy surgeries depend a lot on the surgeon’s skill. Studies have found that surgeon experience is key to safe outcomes for these surgeries.
Learning Curves for Different Techniques
Different hysterectomy methods have different learning curves. For example, laparoscopic and robotic surgeries need special training and lots of practice to get right. Research shows that surgeons who do more of these surgeries tend to have better results for their patients.
- Laparoscopic hysterectomy needs a lot of practice to get good at.
- Robotic surgery requires precise skills and lots of practice.
- Training programs are crucial for improving surgical skills.
Volume-Outcome Relationship
There’s a clear link between how many surgeries a surgeon does and patient outcomes. Surgeons who do more surgeries have fewer complications and better results. This is because they have more experience and have honed their techniques.
Questions to Ask Your Surgeon About Experience
When thinking about a hysterectomy, it’s important to ask about your surgeon’s experience. Here are some questions to ask:
- How many hysterectomies have you done using the recommended method?
- What’s your complication rate for this surgery?
- Can you share any patient success stories or testimonials?
Finding Specialized Gynecologic Surgeons
Choosing a surgeon who specializes in gynecologic surgery can greatly improve safety. You can ask your primary care doctor for a referral or look for specialists through professional groups.
| Criteria | Importance | How to Evaluate |
| Surgeon Experience | High | Ask about the number of procedures performed. |
| Specialization | High | Check if the surgeon specializes in gynecologic surgery. |
| Patient Reviews | Medium | Read patient testimonials and reviews. |
Cost Comparison and Insurance Considerations
The cost of a hysterectomy can change a lot, depending on the procedure and insurance. It’s key for patients to know this to make good choices about their health.
Procedure Costs by Type
The price of hysterectomies varies with the surgery type. Abdominal hysterectomies cost more because they need longer hospital stays and higher fees. On the other hand, laparoscopic and robotic hysterectomies can be cheaper because they have shorter recovery times and hospital stays.
Insurance Coverage Trends
Insurance for hysterectomies varies a lot. Most plans cover a big part of the cost if it’s medically needed. But, it’s important for patients to check their coverage and any costs they might have to pay.
Long-term Cost Implications
There are costs beyond the surgery itself. Patients might need to pay for hormone replacement therapy (HRT) and face future health issues.
Financial Assistance Options
For those struggling financially, there are help options. Hospitals, non-profit groups, and government programs offer aid to those who qualify.
Knowing the costs of hysterectomy and looking into financial help can help patients manage their care’s financial side.
Emerging Techniques and Future Directions
Medical technology is changing gynecologic surgery. New methods are being found to make hysterectomies safer and more effective.
Single-Incision Laparoscopic Surgery
Single-incision laparoscopic surgery is a big step forward in minimally invasive surgery. It uses just one incision, usually in the belly button. This can mean less scarring and quicker healing.
Research shows it’s safe and works well for patients. But, surgeons need special training to do it.
Natural Orifice Transluminal Endoscopic Surgery (NOTES)
Natural Orifice Transluminal Endoscopic Surgery (NOTES) is even more cutting-edge. It does surgery through natural openings, avoiding external cuts. It’s still new, but could change gynecologic surgery by cutting down recovery time and scarring.
Advancements in Robotic Technology
Robotic surgery is getting better, thanks to new tech. The latest robots offer better views, easier controls, and more flexibility. This makes complex surgeries easier for surgeons.
These updates are expected to lead to better results for patients having robotic hysterectomies.
Outpatient Hysterectomy Procedures
The move towards outpatient hysterectomy procedures is growing. It’s because of better surgery methods and anesthesia. Outpatient hysterectomies let patients go home the same day, cutting down on hospital time and infection risks.
Choosing the right patients and having good after-care plans are key for success.
As these new methods improve, it’s important for everyone to keep up. By using the latest tech and practices, gynecologic surgery can get even better. This means better care and outcomes for patients.
Making the Decision: Which Hysterectomy is Right for You?
Talking to your healthcare provider is key when deciding on a hysterectomy. This talk helps figure out the best option for you, based on your health and needs.
Personal Health Factors to Consider
Several health factors are important when choosing a hysterectomy. These include:
- Overall health: Your current health can affect the procedure choice.
- Previous surgeries: Past surgeries can impact your decision.
- Obesity: Being overweight can change surgical risks and recovery.
- Age: Your age might influence the recommended hysterectomy type.
Discussing Options with Your Healthcare Provider
Talking openly with your healthcare provider about hysterectomy options is crucial. This includes:
- Learning about the different hysterectomy procedures.
- Talking about the surgical risks of each method.
- Understanding the recovery process and timeline.
- Considering any long-term effects of the surgery.
Balancing Safety with Other Priorities
While patient safety is most important, other factors matter too. These include recovery time, scarring, and how the surgery affects your life. You should think about these based on your health and what matters most to you.
“The key to making the right decision is a thorough understanding of your condition and the available surgical options.”
Second Opinions and Shared Decision-Making
Getting a second opinion can offer new insights and confidence. Working with your healthcare provider to make a decision ensures your wishes are considered. This leads to a choice that fits you better.
By looking at your health and talking openly with your healthcare provider, you can choose the right hysterectomy for you.
Conclusion
It’s key to know about the different hysterectomy types and their safety. This helps with patient safety and making informed choices. Patients should think about their health and surgical risks when deciding.
Looking at the latest research is important when picking the safest hysterectomy. New tech, like robotic surgery, has made things better. It cuts down recovery time for many.
The choice of hysterectomy should be a team effort. The patient and doctor should talk about health, reasons for the surgery, and risks. This helps make the best decision.
Putting patient safety and informed decision-making first leads to better care. People can make choices that work best for them.
FAQ
What are the different types of hysterectomy procedures?
There are several types of hysterectomy procedures. These include abdominal, vaginal, laparoscopic, and robotic hysterectomies. Each type has its own benefits and risks. The right choice depends on the patient’s health and the reason for the surgery.
Which type of hysterectomy is considered the safest?
Laparoscopic hysterectomy is often seen as safe and effective. It offers less risk and quicker recovery. However, the safest option depends on the patient’s health and the reason for the surgery.
What are the benefits of minimally invasive hysterectomy?
Minimally invasive methods like laparoscopic and robotic hysterectomies have many benefits. They reduce the risk of complications, cause less pain, and lead to faster recovery.
How long is the recovery time for hysterectomy?
Recovery time varies by the type of hysterectomy. Minimally invasive methods usually mean shorter hospital stays and faster recovery. Abdominal hysterectomy might take longer to recover from.
What are the risks associated with hysterectomy?
Hysterectomy risks include infection, blood loss, and surgical complications. The risk level depends on the procedure and the patient’s health.
How does surgeon experience impact hysterectomy outcomes?
A surgeon’s experience is crucial for safe and successful hysterectomies. Patients should ask about their surgeon’s experience. Seeking specialized care is important if needed.
What are the costs associated with different hysterectomy approaches?
Hysterectomy costs vary by procedure, insurance, and other factors. Patients should talk to their healthcare provider about costs and insurance to understand the financial side.
Are there emerging techniques in hysterectomy surgery?
Yes, gynecologic surgery is evolving with new techniques and technologies. Examples include single-incision laparoscopic surgery and advancements in robotic technology.
How can I make an informed decision about hysterectomy?
Making a decision about hysterectomy requires careful thought. Consider your health, surgical risks, and priorities. Discussing with your healthcare provider is key to making the best choice.
What are the long-term implications of hysterectomy?
Hysterectomy’s long-term effects vary by patient and reason for surgery. Discussing potential long-term effects with your healthcare provider is important to understand what to expect.
Reference
- Pillarisetty, L. S. (2023). Vaginal hysterectomy. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554482/