Last Updated on November 26, 2025 by Bilal Hasdemir

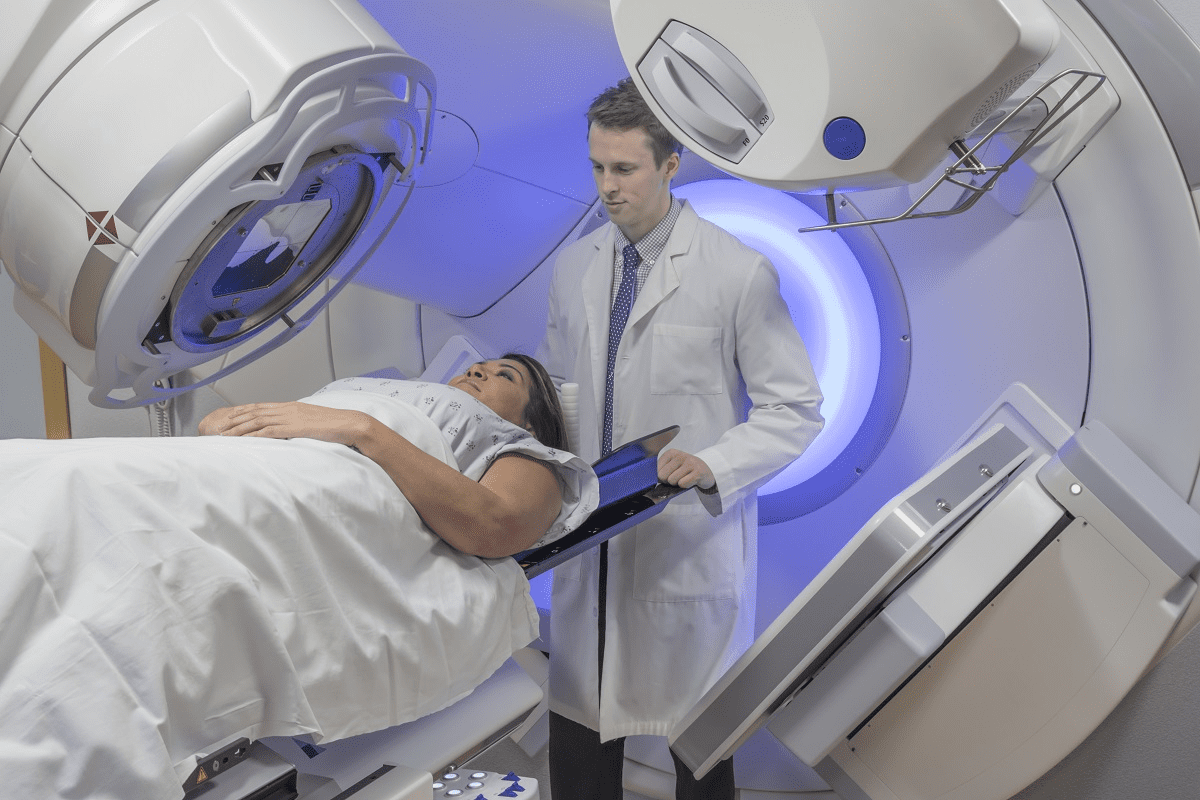
At Liv Hospital, we know how vital effective treatment is for breast cancer. Our hospital is dedicated to top-notch healthcare for all patients, including those from abroad. We provide chemotherapy options like AC-T, FEC, and docetaxel with carboplatin. This ensures each patient gets care tailored to their needs.
It’s key to grasp chemotherapy regimens to manage breast cancer well. Our methods follow the latest research and treatment guidelines. In this piece, we’ll explore six major chemotherapy treatments and their drugs.
Key Takeaways
- AC-T is a common chemotherapy regimen used for breast cancer treatment.
- FEC is another chemotherapy regimen that combines different drugs.
- Docetaxel with carboplatin is used for personalized treatment plans.
- Liv Hospital offers cutting-edge chemotherapy regimens for high-quality care.
- Understanding chemotherapy regimens is key for effective breast cancer management.
Understanding Breast Cancer Chemotherapy
Chemotherapy is key in treating breast cancer. It targets fast-growing cancer cells. This treatment aims to destroy cancer cells, shrink tumors, stop cancer from coming back, and boost survival chances.
How Chemotherapy Targets Cancer Cells
Chemotherapy attacks cells that grow quickly, like most cancer cells. The drugs in chemotherapy aim to:
- Stop cancer cells from dividing and growing
- Block the ways cancer cells use to grow and live
- Kill cancer cells, making tumors smaller
This way, chemotherapy controls cancer growth and spread.
The Role of Chemotherapy in Breast Cancer Treatment
Chemotherapy is vital in breast cancer treatment. It has several roles:
- Shrinks tumors before surgery (neoadjuvant chemotherapy)
- Kills any leftover cancer cells after surgery (adjuvant chemotherapy)
- Treats cancer that has spread to other areas
We pick the best chemotherapy for each patient. Our oncologists talk with patients about the treatment’s benefits and side effects. This helps patients make smart choices about their care.
Knowing how chemotherapy works and its role in breast cancer treatment helps patients. It lets them understand their treatment options better and make informed decisions.
Factors That Determine Breast Cancer Chemotherapy Regimens

Choosing the right breast cancer chemotherapy regimen is complex. At Liv Hospital, we look at many factors to find the best treatment for our patients.
Cancer Stage and Type Considerations
The stage and type of breast cancer are key. We check if the cancer is invasive or not, its size, and if it has spread. This helps us tailor the treatment to the cancer’s specific needs.
- Cancer stage: Early-stage or advanced
- Cancer type: Invasive ductal carcinoma, invasive lobular carcinoma, or other types
- Tumor size and lymph node involvement
Hormone Receptor and HER2 Status
The hormone receptor and HER2 status are also important. We test for estrogen and progesterone receptors, and for HER2 protein or gene amplification. This information helps us choose targeted therapies that work best.
Knowing if these receptors are present or not changes the treatment plan. For example, HER2-positive tumors might get targeted therapies that attack the HER2 proteins.
Patient Health and Previous Treatments
A patient’s health and past treatments matter too. We look at their medical history, current health, and any past chemotherapy or treatments. This helps us reduce side effects and make the treatment more effective.
- Assessing the patient’s overall health and medical history
- Reviewing previous treatments and their outcomes
- Considering possible interactions with other medications
We carefully consider these factors to create a treatment plan that meets each patient’s needs. Our aim is to offer the most effective chemotherapy regimen with fewer side effects and better quality of life.
AC-T Regimen: Adriamycin, Cytoxan, and Taxol
The AC-T regimen is a key treatment for high-risk breast cancer. It combines Adriamycin, Cytoxan, and Taxol. Each drug fights cancer in its own way.
Adriamycin (Doxorubicin): Mechanism and Dosing
Adriamycin, or doxorubicin, is a powerful drug. It stops cancer cells from making DNA and RNA. It’s given at 60 mg/m every 2-3 weeks, based on body size.
Cytoxan (Cyclophosphamide): Function and Administration
Cytoxan, or cyclophosphamide, damages DNA in cancer cells. It’s given through an IV, often with other drugs. It’s usually 600 mg/m on day 1 of each cycle.
Taxol (Paclitaxel): Role and Schedule
Taxol, or paclitaxel, stops cells from dividing by stabilizing microtubules. It’s given after Adriamycin and Cytoxan. Paclitaxel is 175 mg/m every 3 weeks for 3-4 cycles.
When AC-T Is Recommended for High-Risk Cases
We suggest AC-T for high-risk breast cancer. This includes big tumors, lymph node involvement, or aggressive tumors.
“The AC-T regimen has been shown to improve survival rates and reduce recurrence in high-risk breast cancer patients,”
It’s a great choice for those at high risk of cancer coming back.
Knowing about the AC-T regimen helps doctors create better treatment plans. This improves patient outcomes.
TC Regimen: Taxotere and Cyclophosphamide Combination
The TC regimen combines Taxotere (docetaxel) and Cyclophosphamide to fight breast cancer. It uses both drugs’ strengths to target and kill cancer cells.
Taxotere (Docetaxel): Properties and Effectiveness
Taxotere stops cells from dividing by stabilizing microtubules. This leads to cell death, which is key in fighting cancer. It’s very effective, even more so when paired with Cyclophosphamide.
Key benefits of Taxotere include:
- High efficacy in targeting rapidly dividing cancer cells
- Synergistic effect when combined with Cyclophosphamide
- Ability to be used in various stages of breast cancer treatment
Cyclophosphamide’s Role in TC Protocol
Cyclophosphamide damages DNA in cancer cells, stopping them from reproducing. It works well with Taxotere in the TC regimen. Together, they target cancer cells in different ways, making treatment more effective.
The combination of Taxotere and Cyclophosphamide offers a complete approach to treating breast cancer. It tackles both the rapid growth and genetic issues of cancer cells.
| Drug | Mechanism of Action | Key Benefits |
|---|---|---|
| Taxotere (Docetaxel) | Stabilizes microtubules, preventing cell division | High efficacy, synergistic effect with Cyclophosphamide |
| Cyclophosphamide | Damages DNA, preventing cancer cell reproduction | Effective against a wide range of cancer cells, complements Taxotere |
Patient Selection and Treatment Duration
We choose patients for the TC regimen based on their needs and medical history. We look at the cancer’s stage, type, hormone receptor status, and overall health.
The treatment’s length depends on how well the patient responds and tolerates it. The TC regimen is given in cycles, each lasting a few weeks. We watch patients closely to adjust the treatment and manage side effects.
FEC Regimen: 5-Fluorouracil, Epirubicin, and Cyclophosphamide
The FEC regimen is a common treatment for breast cancer. It includes 5-Fluorouracil, Epirubicin, and Cyclophosphamide. This mix is key for treating certain types of breast cancer.
5-Fluorouracil: Mechanism and Effects
5-Fluorouracil stops cancer cells from making DNA. This stops them from growing and eventually kills them. It’s a big part of the FEC regimen, targeting fast-growing cancer cells.
Epirubicin: Function and Cardiac Considerations
Epirubicin works by messing with DNA, which stops cancer cells from making more. But, it can harm the heart. So, doctors closely watch the heart during treatment.
Cyclophosphamide: Dosing in FEC Protocol
Cyclophosphamide damages DNA, stopping cancer cells from growing. The dose depends on the patient and treatment goals. It’s given in a specific schedule.
Clinical Applications and Effectiveness of FEC
The FEC regimen is used in many breast cancer treatments. Studies show it works well. It’s a good choice for many patients.
| Component | Mechanism | Role in FEC Regimen |
|---|---|---|
| 5-Fluorouracil | Inhibits thymidylate synthase, interfering with DNA synthesis | Targets rapidly dividing cancer cells |
| Epirubicin | Intercalates DNA, inhibiting topoisomerase II | Disrupts DNA replication and transcription |
| Cyclophosphamide | Damages DNA, preventing cell reproduction | Prevents cancer cell growth and proliferation |
Knowing how the FEC regimen works helps doctors make treatment plans. This makes treatment better for breast cancer patients.
CMF Regimen: A Traditional Approach
The CMF regimen combines Cyclophosphamide, Methotrexate, and 5-Fluorouracil to treat breast cancer. It has been a key treatment for many breast cancer stages.
Cyclophosphamide in CMF Protocol
Cyclophosphamide is a key part of the CMF regimen. It damages cancer cells’ DNA, stopping them from growing. Cyclophosphamide’s role is vital in making the other drugs work better.
Methotrexate: Mechanism and Administration
Methotrexate is another important drug in the CMF protocol. It stops cancer cells from growing by blocking DNA synthesis. We give Methotrexate through an IV on certain days of the cycle.
5-Fluorouracil: Scheduling and Dosage
5-Fluorouracil is the third part of the CMF regimen. It stops DNA synthesis by blocking thymidylate synthase. The dose and schedule of 5-Fluorouracil depend on the patient’s health and the treatment plan. For more on chemotherapy cycles, see Liv Hospital’s guide on chemotherapy rounds.
Here’s how the CMF regimen works:
| Drug | Dose | Administration Route | Frequency |
|---|---|---|---|
| Cyclophosphamide | 100 mg/m² | Oral | Days 1-14 |
| Methotrexate | 40 mg/m² | Intravenous | Days 1 & 8 |
| 5-Fluorouracil | 600 mg/m² | Intravenous | Days 1 & 8 |
Docetaxel and Carboplatin for Triple-Negative Breast Cancer
Triple-negative breast cancer treatment often includes Docetaxel and Carboplatin. This cancer type doesn’t have estrogen or progesterone receptors or too much HER2 protein. So, chemotherapy is a key treatment.
Triple-Negative Breast Cancer Characteristics
Triple-negative breast cancer makes up 10-15% of all breast cancers. It grows and spreads quickly. It’s more common in young women and those with a BRCA1 mutation. This cancer needs effective treatment fast.
Docetaxel’s Mechanism and Effectiveness
Docetaxel is a taxane drug that stops cancer cells from dividing. It does this by messing with the cell’s microtubules. Studies show it works well against triple-negative breast cancer.
Carboplatin’s Role in Targeting DNA Repair
Carboplatin is a drug that messes with DNA replication. It forms adducts with DNA, stopping cancer cells from fixing DNA damage. This leads to cell death. It’s very useful in triple-negative breast cancer, even with BRCA mutations.
Treatment Schedule and Response Rates
Docetaxel and Carboplatin are given every three weeks for 4-6 cycles. The schedule can change based on how well the patient does. Research shows this combo can help many patients with triple-negative breast cancer.
| Study | Number of Patients | Overall Response Rate |
|---|---|---|
| Study 1 | 100 | 60% |
| Study 2 | 150 | 55% |
| Study 3 | 200 | 65% |
Dose-Dense Chemotherapy Approaches
Dose-dense chemotherapy is a new way to fight breast cancer. It means giving chemotherapy more often to pack a bigger punch. This method aims to kill more cancer cells and help patients live longer.
The Science Behind Dose-Dense Treatment
Dose-dense chemotherapy works by attacking cancer cells quickly. It’s based on the idea that cancer grows faster when it’s not stopped often. This way, the treatment can keep up with the cancer’s growth.
By giving chemotherapy more frequently, we can make it more effective. This is very important for people with aggressive breast cancer. They might see the biggest benefits from this treatment.
Common Dose-Dense Protocols (AC-T, EC)
There are two main dose-dense chemotherapy plans: AC-T and EC. AC-T uses Adriamycin, Cytoxan, and Taxol. EC uses Epirubicin and Cyclophosphamide. Both are designed to fight breast cancer hard.
The AC-T plan is a strong dose-dense option. It combines Adriamycin, Cytoxan, and Taxol. This mix is meant to hit breast cancer cells hard and lower the chance of it coming back.
| Regimen | Drugs | Administration Schedule |
|---|---|---|
| AC-T | Adriamycin, Cytoxan, Taxol | Every 2 weeks |
| EC | Epirubicin, Cyclophosphamide | Every 2 weeks |
Benefits, Risks, and Support Medications
Dose-dense chemotherapy has many good points. It can lead to better survival rates and lower chances of cancer coming back. But, it also has downsides like more side effects and risks of serious problems.
To lessen these risks, we use medicines like G-CSF. This helps manage side effects and keeps patients safe. Watching patients closely and giving them the right care is key to making dose-dense chemotherapy work well.
Understanding dose-dense chemotherapy helps us treat breast cancer better. We aim to give each patient the best care possible. This means using the latest in chemotherapy to help them live longer and better.
Managing Side Effects of Breast Cancer Chemotherapy
At Liv Hospital, we focus on the side effects of breast cancer chemotherapy. We want to make sure our patients get the best care. Chemotherapy is effective but can cause tough side effects that affect patients’ lives.
Common Physical Side Effects and Management
Physical side effects from breast cancer chemotherapy are common. These can include:
- Fatigue: Persistent tiredness that can be managed with rest, exercise, and nutritional support.
- Nausea and Vomiting: Controlled with antiemetic medications and dietary adjustments.
- Hair Loss: A distressing side effect for many, for which we offer counseling and support.
We work with our patients to create plans for managing these side effects. This helps improve their comfort and well-being during treatment.
Emotional and Psychological Support
The emotional and psychological effects of chemotherapy should not be ignored. Patients often feel anxious, depressed, and worried about the future. Our team provides:
- Counseling: To help patients cope with their emotions and adjust to their diagnosis.
- Support Groups: Where patients can share their experiences and find solidarity with others undergoing similar treatments.
By focusing on the emotional and psychological aspects, we help our patients stay positive and resilient.
Supportive Medications and Therapies
We use supportive medications and therapies to reduce side effects and improve comfort. These include:
- Growth Factors: To reduce the risk of infection and support blood cell recovery.
- Pain Management: Tailored to each patient’s needs to ensure effective pain relief.
Our approach is holistic. We combine conventional treatments with supportive care to improve patient outcomes.
Self-Care Strategies During Treatment
Self-care is key in managing chemotherapy side effects. We encourage our patients to:
- Stay Hydrated: Drinking plenty of water to help flush out toxins.
- Maintain a Balanced Diet: Eating nutritious foods to support their body’s needs during treatment.
- Exercise Regularly: Gentle exercise can help reduce fatigue and improve mood.
By following these self-care strategies, patients can actively participate in their recovery and well-being.
Liv Hospital’s Approach to Breast Cancer Chemotherapy Regimens
At Liv Hospital, we focus on giving each patient the best chemotherapy plans. We make sure our treatments are top-notch and fit each person’s needs. This way, our patients get the best care possible.
Internationally Competitive Treatment Protocols
We always keep up with the latest in breast cancer treatment. Our doctors work with experts worldwide to use the best treatments. This means our patients get new therapies that might not be available elsewhere.
Our treatment plans are flexible. We can change the chemotherapy if needed, based on how the patient responds and any side effects.
Personalized Regimen Selection Process
Every patient’s fight against breast cancer is different. That’s why we focus on personalized care at Liv Hospital. Our skilled oncologists work with each patient to pick a treatment plan that fits their needs, medical history, and preferences.
“Personalized medicine is not just a buzzword; it’s a commitment to treating the individual, not just the disease.”
Patient Support During Chemotherapy
Chemotherapy can be tough, both physically and emotionally. That’s why we offer lots of support to our patients. We help with emotional and psychological counseling, nutrition, and managing side effects.
We want our patients to feel supported and cared for. By using advanced treatments and caring for our patients, we aim for the best results.
At Liv Hospital, we are dedicated to making a positive impact on the lives of our patients and their families.
Conclusion: Making Informed Decisions About Chemotherapy
Breast cancer chemotherapy regimens are key in managing different types of breast cancer. At Liv Hospital, we have various chemotherapy options. These include AC-T, FEC, and docetaxel with carboplatin. We aim to give personalized and high-quality care to our patients.
Understanding the different chemotherapy regimens helps patients make informed choices. We provide detailed support and care during their treatment. This ensures they get the best results.
Choosing the right chemotherapy is vital for breast cancer patients. We work with our patients to find the best regimen. We consider their individual needs and health status.
FAQ
What is chemotherapy, and how does it work in treating breast cancer?
Chemotherapy uses drugs to fight cancer cells. It targets fast-growing cells, shrinking tumors and preventing cancer from coming back. This helps improve survival chances.
What factors determine the most suitable breast cancer chemotherapy regimen?
The right chemotherapy depends on several things. These include the cancer’s stage and type, hormone receptor and HER2 status, and the patient’s health and past treatments.
What is the AC-T chemotherapy regimen, and when is it recommended?
The AC-T regimen combines Adriamycin, Cytoxan, and Taxol. It’s best for high-risk breast cancer patients. It boosts survival rates and lowers the chance of cancer coming back.
What is the TC regimen, and how does it work?
The TC regimen mixes Taxotere and Cyclophosphamide. Taxotere stops cells from dividing, while Cyclophosphamide damages DNA. This stops cancer cells from growing.
What is the FEC regimen used for in breast cancer treatment?
The FEC regimen includes 5-Fluorouracil, Epirubicin, and Cyclophosphamide. It’s used in both early and late stages of breast cancer treatment.
How is triple-negative breast cancer treated with chemotherapy?
Triple-negative breast cancer is treated with Docetaxel and Carboplatin. Docetaxel stops cells from dividing, and Carboplatin damages DNA. This stops cancer cells from growing.
What is dose-dense chemotherapy, and what are its benefits and risks?
Dose-dense chemotherapy gives chemotherapy more often to increase the dose. It can improve survival and lower recurrence rates. But, it can also increase side effects and toxicity.
How are side effects of breast cancer chemotherapy managed?
Side effects are managed with various supportive measures. These include medications, therapies, emotional support, and self-care. They help patients stay well during treatment.
What kind of support can patients expect during chemotherapy at Liv Hospital?
At Liv Hospital, patients get full support during chemotherapy. This includes emotional support, medications, and therapies for side effects. They also learn self-care strategies to stay well.