
In 2020, nearly 252,000 bariatric surgeries were performed in the United States. This number continues to rise as obesity rates increase. For anyone considering weight loss surgery, understanding the Riskiest Bariatric Surgery and its potential complications is crucial.
Studies indicate that not all bariatric procedures carry the same risk. Identifying theRiskiest Bariatric Surgery helps patients and doctors make informed decisions based on health, age, and overall fitness. Some surgeries have higher chances of serious complications, while others are relatively safer.
As more people opt for bariatric surgery, knowing which is the Riskiest Bariatric Surgery allows for careful planning, proper preparation, and improved safety during the procedure. Discussing the risks and benefits with a healthcare provider ensures that patients are aware of the challenges and can take steps to reduce complications.
By being informed about the Riskiest Bariatric Surgery, patients can weigh the benefits against potential risks and choose the best option for their weight loss journey.
Key Takeaways
- Different bariatric surgeries have varying levels of risk.
- Understanding possible complications is key for patients.
- Some bariatric procedures are more prone to severe complications.
- The number of bariatric surgeries in the US is increasing.
- Knowing the risks helps make a better choice.
- Research on bariatric surgery outcomes helps identify risk factors.
Understanding Bariatric Surgery and Its Purpose

Bariatric surgery helps people lose a lot of weight and get healthier. It’s for those who are very overweight and have health problems because of it.
Definition and Types of Bariatric Procedures
Bariatric surgery changes the stomach or intestines to control food intake or absorption. The main types are:
- Gastric Bypass Surgery: Makes a small stomach pouch and changes the intestine’s path.
- Sleeve Gastrectomy: Takes out a big part of the stomach, leaving a narrow sleeve.
- Adjustable Gastric Banding: A band is put around the stomach’s top to make a small pouch.
- Duodenal Switch: Removes a big part of the stomach and changes the intestines’ path.
Obesity-Related Health Conditions Addressed by Surgery
Bariatric surgery helps with many health problems caused by being overweight, such as:
- Type 2 Diabetes: Many see big improvements or even no diabetes anymore.
- Hypertension: Losing weight can lower blood pressure.
- Sleep Apnea: Weight loss can make sleep better.
- Joint Pain: Less weight means less pressure on joints.
General Benefits of Weight Loss Surgery
Bariatric surgery offers more than just weight loss, including:
- Improved Overall Health: Less obesity-related health issues.
- Enhanced Quality of Life: Better mobility and doing more activities.
- Long-Term Weight Management: Lasting weight loss with lifestyle changes.
Knowing about bariatric surgery’s purpose and benefits helps people choose the right treatment.
Overview of Risk Assessment in Bariatric Procedures
Bariatric surgery risk assessment looks at many things. It checks the patient’s health, how complex the surgery is, and possible problems. This detailed check is key to see if bariatric surgery is right for someone. It also helps lower the risks of the surgery.
How Surgical Risk is Measured
Measuring surgical risk in bariatric surgery involves different tools and criteria. It looks at the patient’s overall health, body mass index (BMI), any health problems they have, and past surgeries. The type of surgery also affects the risk.
Tools like scoring systems are used to rate the risk of problems. For example, the American Society of Anesthesiologists (ASA) Physical Status Classification System helps judge a patient’s health before surgery.
Short-Term vs. Long-Term Complications
Bariatric surgery has risks of both short-term and long-term problems. Short-term complications happen right after surgery. These can be bleeding, infection, or breathing or heart issues.
Long-term complications can show up months or years later. These might include nutritional problems, gastrointestinal complications, or issues with the surgery site like hernias.
The Role of Patient Selection in Risk Determination
Choosing the right patient is key in bariatric surgery risk. It’s important to check the patient’s health, mental readiness, and commitment to lifestyle changes after surgery. This helps find patients at higher risk and tailor the surgery to reduce risks.
A team of doctors, nutritionists, and psychologists work together. They decide if surgery is right for the patient. They also plan the care before and after surgery.
Gastric Bypass Surgery: Risk Profile
Gastric bypass surgery comes with many risks. These risks include short-term problems and long-term health issues. This surgery, also known as Roux-en-Y gastric bypass, makes a small stomach pouch and changes the small intestine’s path.
Procedure Overview and Mechanism
This surgery makes the stomach smaller and changes food’s path in the intestines. This can lead to a lot of weight loss. It involves making a small pouch at the stomach’s top and connecting it to the small intestine. This bypasses a big part of the stomach and upper intestine.
“Gastric bypass surgery is a highly effective weight loss solution, but it’s not without risks,” notes a leading bariatric surgeon. “Patients must be aware of the possible complications and long-term health effects.”
Common Complications and Their Frequency
Common problems include internal hernias, bowel obstruction, and vitamin deficiencies. Studies show that internal hernias happen in 2-4% of patients. Vitamin deficiencies affect up to 30% of patients because of poor absorption.
- Internal hernias: 2-4%
- Vitamin deficiencies: up to 30%
- Bowel obstruction: 1-2%
Mortality Rates and Severe Adverse Events
The death rate for this surgery is low, between 0.1% and 0.5%. But, serious problems can happen. These include pulmonary embolism, heart issues, and leaks at the surgery site.
Mortality Rate: 0.1% to 0.5%
Long-Term Nutritional Concerns
After surgery, long-term nutritional worries include vitamin and mineral deficiencies. These often include vitamin B12, iron, and calcium. Patients must follow a strict diet and take supplements to avoid these problems.
“Long-term follow-up is key to manage nutritional deficiencies and avoid complications,” says a nutritional expert in bariatric care.
Knowing the risks and taking steps to prevent them can help patients have a successful surgery.
Sleeve Gastrectomy: Possible Complications
Sleeve gastrectomy, like other bariatric surgeries, has risks to consider. This surgery removes a big part of the stomach, leaving a narrow “sleeve” or tube-like stomach.
How the Procedure Works
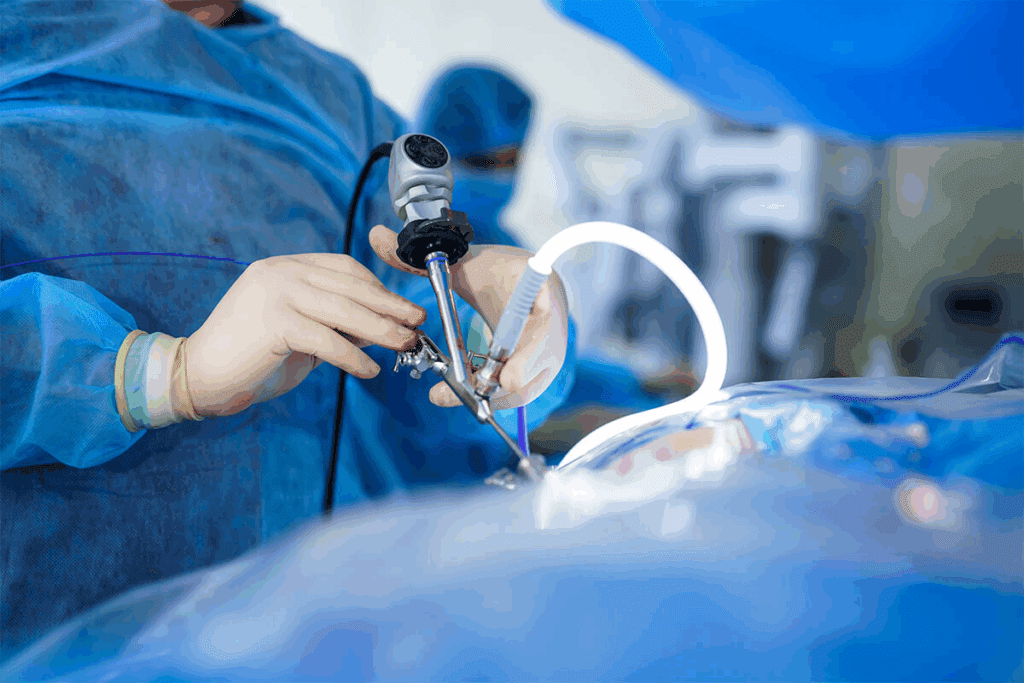
The surgery is done laparoscopically, with small incisions in the belly. The surgeon takes out about 80% of the stomach, making a banana-shaped gastric sleeve.
Short-Term Surgical Risks
Short-term risks of sleeve gastrectomy include:
- Leakage: A leak from the staple line is a serious complication.
- Bleeding: Hemorrhage can occur during or after surgery.
- Infection: As with any surgery, there is a risk of infection.
Long-Term Complications
Long-term complications may include:
- Nutritional deficiencies: Patients may experience deficiencies in vitamins and minerals.
- Gastroesophageal reflux disease (GERD): Some patients may develop or experience worsening of GERD symptoms.
- Weight regain: There is a possibility of weight regain if dietary habits are not maintained.
Comparative Safety Profile
Comparing sleeve gastrectomy to other bariatric procedures, it’s seen as safer than gastric bypass. But, the decision should be based on each patient’s needs.
Duodenal Switch: The Most Complex Bariatric Procedure
The duodenal switch is a complex bariatric surgery known for its significant weight loss benefits and risks.
Procedure Mechanics and Complexity
The duodenal switch combines two steps: a sleeve gastrectomy and an intestinal bypass. The sleeve gastrectomy makes the stomach smaller, limiting how much food you can eat. The intestinal bypass changes how food moves through your intestines, reducing calorie absorption.
This surgery’s complexity comes from its two-part approach. It limits food intake and changes how your body absorbs nutrients. This makes it effective but also increases the risk of complications.
Highest Risk Factors and Complications
The duodenal switch carries high risks, including nutritional deficiencies and malabsorption issues. Patients may face problems with vitamins and minerals, like vitamin B12, iron, and calcium.
| Complication | Frequency |
| Nutritional Deficiencies | High |
| Malabsorption Issues | High |
| Surgical Complications | Moderate |
Nutritional Deficiencies and Malabsorption Issues
Those who have the duodenal switch need to take supplements for life to avoid deficiencies. It’s important to keep an eye on their nutrition to avoid problems.
Without proper nutrition, patients can face serious health issues. These include anemia, osteoporosis, and neurological problems. Teaching patients about diet and supplements is key.
Patient Selection Criteria
Choosing the right patients for the duodenal switch is essential due to its complexity and risks. The best candidates have a high BMI and obesity-related health issues that haven’t been solved by other methods.
Choosing patients involves a detailed look at their medical history, mental readiness, and commitment to ongoing care. This ensures they understand and are ready for the challenges ahead.
Adjustable Gastric Banding: Risks and Complications
Adjustable gastric banding is a simple bariatric surgery but comes with risks. These include band slippage and erosion. The surgery creates a small pouch in the stomach by placing a band around it. This limits how much food you can eat.
Procedure Details and Device-Related Issues
The adjustable gastric banding procedure is reversible and adjustable. But, device-related issues are a big worry. These can be mechanical failures like band leakage or port malfunction. These problems might need more surgeries.
Band Slippage and Erosion Concerns
Band slippage and erosion are major complications. Band slippage happens when the band moves, causing blockages or reducing its effect. Erosion is when the band goes through the stomach wall, a serious issue that needs quick medical help.
| Complication | Description | Frequency |
| Band Slippage | Band moves from its original position | 5-10% |
| Erosion | Band wears through the stomach wall | 1-5% |
| Device-Related Issues | Mechanical failures, leakage, or port malfunction | 10-20% |
Reoperation Rates and Long-Term Outcomes
Because of these complications, reoperation rates are high. Many patients need more surgery to adjust or remove the band. The outcomes vary, with some losing weight long-term and others gaining it back or facing ongoing issues.
Choosing adjustable gastric banding needs careful thought and talking to a healthcare expert. Knowing the risks and long-term effects is key to making a good choice.
Gastric Balloon Procedures: Safety Considerations
Intragastric balloon placement is a non-surgical way to lose weight. It involves putting a balloon in the stomach to make it smaller. This helps you eat less and lose weight.
Intragastric Balloon Placement Process
The process of putting in a gastric balloon is simple. It’s done under sedation. The balloon goes in through the mouth with an endoscope and is filled with saline.
This whole thing takes less than an hour. Most people can go home the same day. The procedure’s simplicity makes it appealing for those looking for a less invasive way to lose weight.
Potential Complications and Side Effects
Even though it’s safe, gastric balloon procedures can have side effects. You might feel nausea, vomiting, and abdominal pain. Rare but serious problems like balloon deflation or migration can also happen.
Temporary Nature and Risk-Benefit Profile
The balloon is usually taken out after six months to a year. This can be good or bad. It’s a chance to try a big weight loss effort without a long-term commitment.
But, keeping the weight off after the balloon is gone can be hard. It requires big lifestyle changes. It’s important to weigh the risks and benefits before getting a gastric balloon.
Deciding to get a gastric balloon should be a thoughtful choice. You should talk to a healthcare professional first.
The Riskiest Bariatric Surgery: Comparative Analysis
It’s important to know the risks of different bariatric surgeries before making a choice. These surgeries help people lose weight and improve their health. But, each surgery has its own set of risks.
Mortality Rate Comparison Across Procedures
The risk of death is a key factor when looking at bariatric surgeries. Different surgeries have different death rates. For example, gastric bypass surgery has a death rate between 0.1% and 0.5%. On the other hand, sleeve gastrectomy and adjustable gastric banding have death rates below 0.1%.
- Gastric Bypass: 0.1% – 0.5% mortality rate
- Sleeve Gastrectomy: Less than 0.1% mortality rate
- Adjustable Gastric Banding: Less than 0.1% mortality rate
- Duodenal Switch: Higher mortality rate compared to other procedures
Complication Frequency and Severity
Complications can happen during or after surgery, and they vary by procedure. Gastric bypass and duodenal switch are more complex and have more complications than sleeve gastrectomy or adjustable gastric banding. Common problems include infections, bleeding, and nutritional issues.
| Procedure | Complication Rate | Common Complications |
| Gastric Bypass | Higher | Infection, bleeding, nutritional deficiencies |
| Sleeve Gastrectomy | Moderate | Leakage, bleeding |
| Adjustable Gastric Banding | Lower | Band slippage, erosion |
Reoperation Requirements
Reoperation rates differ among bariatric surgeries. Adjustable gastric banding often needs more surgeries because of problems like band slippage or erosion. In contrast, sleeve gastrectomy usually needs fewer surgeries.
Risk-Benefit Analysis by Procedure
Each bariatric surgery has its own risk and benefit. Gastric bypass can lead to significant weight loss and health improvements but comes with higher risks. Sleeve gastrectomy offers moderate weight loss with fewer complications.
Choosing a bariatric surgery should consider your health, weight loss goals, and the risks of each procedure.
Patient-Specific Risk Factors in Bariatric Surgery
The risk of bariatric surgery varies from person to person. Knowing these factors helps doctors decide if surgery is right for a patient. It also helps reduce risks.
Age and Its Impact on Surgical Risk
Age is a big factor in bariatric surgery risks. Older patients face more risks because their bodies are less strong. They also have more health problems.
Research shows that people over 60 are more likely to die or have serious problems after surgery. This is compared to younger patients.
BMI and Comorbidity Considerations
The patient’s BMI and health problems are key in deciding surgery risks. Those with a very high BMI face more risks. Health issues like diabetes and sleep apnea also add to the risk.
Previous Abdominal Surgeries
Having had surgery before can make bariatric surgery harder. It can cause adhesions and change the body’s shape. Doctors need to look at past surgeries carefully.
Psychological Factors Affecting Outcomes
Psychological health is important for bariatric surgery success. Mental health issues or wrong expectations can make it hard to lose weight and stay healthy. It’s important to check mental health before surgery.
| Risk Factor | Impact on Bariatric Surgery |
| Age | Increased risk of complications in older patients |
| BMI and Comorbidities | Higher BMI and presence of comorbidities increase risk |
| Previous Abdominal Surgeries | Potential for adhesions and surgical complications |
| Psychological Factors | Impact on weight loss success and long-term health benefits |
Surgeon Experience and Hospital Volume: Impact on Safety
Surgeon experience and hospital volume are key to safety in bariatric surgery. Bariatric surgery is complex, needing a skilled surgeon and a well-coordinated team.
The Learning Curve in Bariatric Surgery
Bariatric surgery, like other surgeries, has a learning curve for surgeons. Studies show that more experienced surgeons have better results. This is because they know the procedure well, have better skills, and choose the right patients.
At first, surgeons face a higher risk of complications. But, as they gain experience, they improve their techniques. This leads to fewer problems for patients. It’s important for patients to ask about their surgeon’s experience.
Center of Excellence Certification
Organizations like the American Society for Metabolic and Bariatric Surgery (ASMBS) give Center of Excellence certification. This is for hospitals that meet certain standards, like having experienced surgeons and a good care team. These centers have better patient outcomes than non-certified ones.
Being certified means the hospital follows strict standards. This includes having skilled surgeons and a team that provides good follow-up care. Patients at these centers often have fewer complications and better long-term results.
Correlation Between Volume and Outcomes
Many studies show that more bariatric surgeries at a hospital lead to better results. High-volume hospitals have fewer complications, readmissions, and deaths.
| Hospital Volume | Mortality Rate | Complication Rate |
| Low Volume | 0.5% | 10% |
| High Volume | 0.1% | 5% |
These numbers show that high-volume centers are safer. Choosing a hospital with a good track record in bariatric surgery is key.
Post-Surgical Care and Its Role in Risk Reduction
The time after bariatric surgery is very important. Good care can lower the chance of problems. It includes many key steps to help the surgery go well.
Early Complication Detection
Spotting problems early is a big part of care after surgery. Looking for signs of infection, bleeding, or other bad effects is key in the first few weeks. Patients should watch their health closely and tell their doctor about any odd symptoms right away.
Nutritional Monitoring and Supplementation
Watching what you eat is also very important. Bariatric surgery can cause nutrient shortages if not managed right. Seeing a nutritionist regularly helps catch these issues early. Sometimes, taking extra nutrients is needed to make sure you get everything you need.
| Nutritional Aspect | Pre-Surgery | Post-Surgery |
| Protein Intake | Normal dietary intake | Supplementation recommended |
| Vitamin B12 | Normal levels | Monitoring and supplementation |
| Iron | Normal levels | Monitoring and supplementation |
Follow-Up Schedule Importance
Having a good plan for follow-up visits is key for bariatric surgery success. Going to the doctor regularly lets them check on you and catch any problems early. Sticking to the follow-up plan is very important for the best results.
Lifestyle Modifications for Optimal Outcomes
Changing your lifestyle is also very important. Patients should eat healthy and exercise often. These habits help with weight loss and improve overall health.
In summary, post-surgical care includes many important steps. These are early problem detection, watching your diet, following up with your doctor, and making lifestyle changes. By focusing on these, patients can greatly reduce risks and have a good outcome from bariatric surgery.
Conclusion: Making an Informed Decision About Bariatric Surgery
It’s important for patients to know the risks and benefits of bariatric surgery. Different procedures have different risks. Knowing these helps with patient education.
Patients should think about their health, how severe their obesity is, and the chance for weight loss. This helps them decide if surgery is right for them.
Deciding on surgery means understanding the surgery and the lifestyle changes after it. With the right education, people can handle the process better and get good results.
Bariatric surgery can change lives for those with obesity. Knowing the risks and benefits is the first step to a healthier life.
FAQ
What are the most common risks associated with bariatric surgery?
Risks include bleeding, infection, and leaks. Also, bowel obstruction and nutritional deficiencies are common. Adjustable gastric banding can have device-related issues.
How do different bariatric procedures compare in terms of risk?
Gastric bypass and duodenal switch are more complex. They have higher risks than sleeve gastrectomy or adjustable gastric banding. Each patient’s risk depends on their health.
What is the mortality rate for bariatric surgery?
The death rate varies by procedure. It’s usually between 0.1% and 0.5%. Gastric bypass and duodenal switch have higher rates.
How does patient selection impact the risk of bariatric surgery?
Choosing the right patient is key. Age, BMI, and health conditions affect risk. A careful evaluation can lower risks.
What are the long-term nutritional concerns after bariatric surgery?
Long-term, patients might face vitamin and mineral deficiencies. These include vitamin B12, iron, and calcium. Lifelong supplements and monitoring are needed.
How does surgeon experience affect the outcome of bariatric surgery?
Surgeon experience matters a lot. More experienced surgeons have better results and fewer complications. They have honed their skills over time.
What is the role of post-surgical care in minimizing risks?
Post-surgical care is vital. It helps catch complications early and ensures proper nutrition. Lifestyle changes are also key for success.
Can previous abdominal surgeries increase the risk of bariatric surgery?
Yes, previous surgeries can make bariatric surgery riskier. Adhesions and altered anatomy are concerns. Surgeons must assess these factors carefully.
How do psychological factors affect bariatric surgery outcomes?
Mental health and lifestyle changes post-surgery are critical. They can greatly influence success and risk. A thorough pre-surgical evaluation is important.
What is the significance of Center of Excellence certification for bariatric surgery?
Certification shows a facility meets quality and safety standards. It’s linked to better outcomes and fewer complications.
Are there any non-surgical alternatives to bariatric surgery?
Yes, intragastric balloon placement is a less invasive option. It’s reversible. But, its effectiveness varies by individual.
How does the complexity of duodenal switch impact its risk profile?
Duodenal switch is complex, leading to higher risks. Nutritional deficiencies and malabsorption are common. Careful patient selection is necessary.
What are the risks associated with adjustable gastric banding?
Risks include device problems, band slippage, and erosion. Reoperation may be needed. Weight loss outcomes can vary.
How does BMI influence the risk of bariatric surgery?
Higher BMI increases surgical risk. It’s linked to mobility issues, comorbid conditions, and surgical challenges.
What lifestyle modifications are necessary after bariatric surgery?
Patients need to make big lifestyle changes. This includes diet, exercise, and supplements. These are essential for success.
References
- Chang, S. H., Stoll, C. R., Song, J., Varela, J. E., Eagon, C. J., & Colditz, G. A. (2014). The effectiveness and risks of bariatric surgery: An updated systematic review and meta-analysis, 2003–2012. JAMA Surgery, 149(3), 275–287. https://jamanetwork.com/journals/jamasurgery/fullarticle/1790378



































