Last Updated on November 27, 2025 by Bilal Hasdemir

How much Pain after thoracic surgery should you expect? We address the negative discomfort and detail the crucial management options available.
Thoracic surgery is a complex procedure that can greatly affect a patient’s life. Understanding the pain from these surgeries is key for a good recovery. Patients often worry about the pain they might face.
Good post-surgical pain management makes patients more comfortable. It also lowers the chance of complications, leading to better results in thoracic surgery recovery.
Key Takeaways
- Thoracic surgery can significantly impact a patient’s quality of life.
- Understanding pain management is critical for recovery.
- Effective pain management improves patient comfort and reduces complications.
- Post-surgical pain management is a key part of the recovery process.
- Proper care can lead to better outcomes in thoracic surgery recovery.
Understanding Thoracic Surgery

To understand the pain from thoracic surgery, we need to look at the different surgeries involved. Thoracic surgery is complex, focusing on the chest area. Each surgery has its own pain risks.
Common Types of Thoracic Surgical Procedures
There are many thoracic surgeries, like thoracotomy, VATS (Video-Assisted Thoracic Surgery), and robotic-assisted surgery. Each affects pain differently after surgery.
- Thoracotomy makes a big cut in the chest to reach inside. This can cause a lot of pain because of the large cut and possible nerve damage.
- VATS uses small cuts and a camera for surgery. It’s less painful than thoracotomy but can cause some discomfort at the cut sites.
- Robotic-assisted surgery uses a robotic system for precise surgery with small cuts. This might lead to less pain after surgery.
Anatomical Considerations of the Chest Cavity
The chest cavity is complex, housing important organs like the heart and lungs. Knowing its anatomy helps us understand post-surgery pain.
The rib cage protects these organs but makes surgery tricky. Cutting through muscles and bones can cause pain after surgery.
Nerves in the chest and organs can also be affected by surgery. This adds to the pain patients feel.
The Nature of Pain After Thoracic Surgery

Pain after thoracic surgery is complex and varies from person to person. It’s important to understand this to manage pain effectively. The pain’s severity and type depend on the surgery, the patient’s pain tolerance, and their health.
Acute vs. Chronic Post-Thoracic Surgery Pain
Pain after thoracic surgery falls into two categories: acute and chronic. Acute pain is immediate and usually goes away as the body heals. Chronic pain lasts longer, sometimes for years.
Knowing the difference between these types of pain is key. Acute pain is normal after surgery. But chronic pain can greatly affect a person’s life, needing a more detailed plan for management.
Factors That Influence Pain Severity
Many things can affect how much pain someone feels after thoracic surgery. These include:
- The type and extent of the surgical procedure
- Individual patient factors such as age, overall health, and pain tolerance
- The presence of pre-existing pain conditions
- The surgical approach, including whether the surgery was open or minimally invasive
| Factor | Influence on Pain Severity |
| Surgical Procedure Type | Major surgeries like thoracotomies tend to result in higher pain levels compared to minimally invasive procedures like VATS. |
| Patient Age and Health | Older patients or those with comorbidities may experience different pain levels and require adjusted pain management strategies. |
| Pre-existing Pain Conditions | Patients with chronic pain conditions may have a different pain threshold and require more complex pain management. |
Understanding these factors helps healthcare providers create better pain management plans. This improves patient outcomes and satisfaction.
Pain Intensity Scale for Thoracic Procedures
Pain after thoracic surgery is a big worry for patients. The pain intensity scale helps us understand what to expect. It’s key for both patients and doctors to manage pain well.
Thoracic surgeries vary in how complex and invasive they are. This affects the pain after surgery. The pain intensity scale is a way to measure the pain patients feel after thoracic surgery.
Thoracotomy Pain Levels
Thoracotomy, an open-chest surgery, causes a lot of pain after. This is because of the big cut and the need to spread the ribs. Patients usually say their pain is between 6 and 8, on a scale of 0 to 10.
Effective pain management strategies are key for those having thoracotomy. They help reduce pain and aid in recovery.
VATS Procedure Pain Comparison
VATS, or Video-Assisted Thoracic Surgery, is less invasive than thoracotomy. It uses smaller cuts and causes less damage. So, patients feel less pain after VATS, usually scoring between 3 to 5 on the pain scale.
VATS leads to faster recovery times and shorter hospital stays. This makes it a good choice for many.
Robotic-Assisted Surgery Pain Expectations
Robotic-assisted thoracic surgery is the newest, most precise way to do surgery. It uses even smaller cuts than VATS. Patients feel the least pain after this surgery, often scoring below 3 on the pain scale.
This low pain is because of the surgery’s minimally invasive nature. The robotic system also offers better vision and control.
Immediate Post-Operative Pain Experience
Managing pain well right after thoracic surgery is key. In the first 24-48 hours, patients are watched closely in the hospital. They get care to handle their pain well.
First 24-48 Hours After Surgery
The first 24-48 hours after thoracic surgery are tough. Patients feel a lot of pain from the surgery. Managing pain well is important for a smooth recovery. It helps them breathe, cough, and move around sooner, lowering the chance of problems.
- Patients are watched for pain levels and get medicine as needed.
- Pain relief plans are made just for them, based on their health history.
Hospital Pain Management Protocols
Hospitals have set pain management plans to help patients. These plans mix medicine and other ways to help.
- Medicine like opioids and non-opioid pain relievers are used.
- Other methods include how patients are positioned, breathing exercises, and relaxation techniques.
By mixing these methods, doctors can create pain management plans that fit each patient. This makes patients more comfortable and helps them recover better.
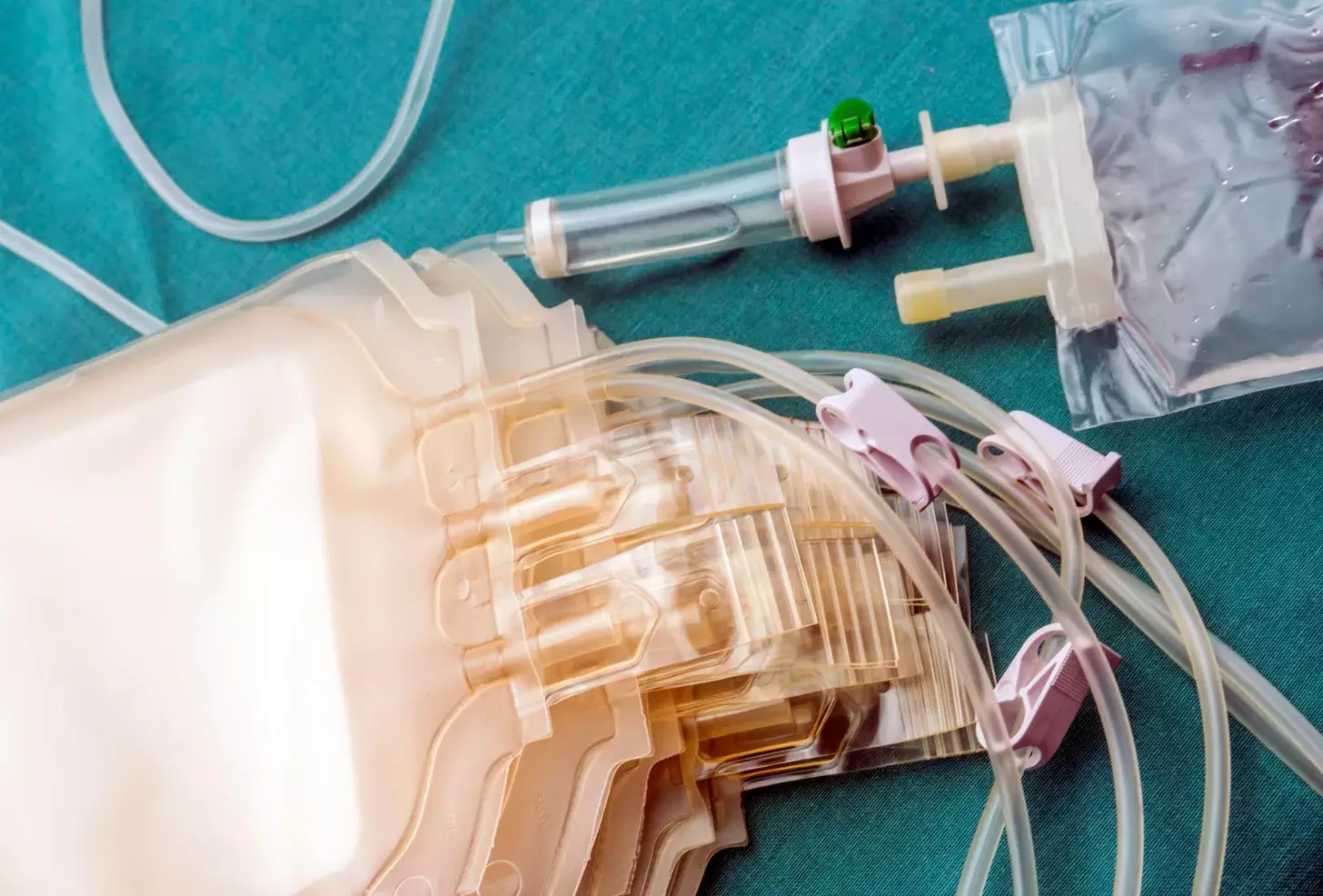
Pain from Chest Tubes and Drainage Devices
Chest tubes are a common part of thoracic surgery. Knowing how they affect pain is key to managing it well. These tubes can cause discomfort and pain, which can slow down recovery.
Discomfort During Placement
Putting in chest tubes can hurt because of the way tissues are moved and the foreign objects in the chest. Doctors use local anesthesia and pain meds to help with this.
Ongoing Pain With Tubes in Place
Patients often feel pain and discomfort with chest tubes in. This can be because of the tube itself, the stitches holding it in place, or the reason for needing the tube. It’s important to have good pain management to lessen this discomfort.
Pain During Chest Tube Removal
Removing chest tubes can also hurt, but it’s usually just for a short time. The pain is sharp but doesn’t last long. It’s important to manage pain well during this time to make patients more comfortable.
| Pain Management Strategy | Description | Effectiveness |
| Medication | Use of pain relief medication to manage pain | High |
| Breathing Exercises | Deep breathing exercises to minimize discomfort and improve lung function | Moderate |
| Positioning | Adjusting patient position to reduce strain on the chest and tube site | Moderate |
Understanding the pain from chest tubes and using good pain management can really help patients feel better after thoracic surgery.
Breathing Pain After Thoracic Surgery
Patients often face breathing pain after thoracic surgery. Breathing can become uncomfortable after such surgeries. We’re here to explain why and how to reduce this pain.
Why Deep Breathing Hurts
Deep breathing hurts after thoracic surgery because the chest area is involved. This includes the lungs, rib cage, and muscles. During surgery, these areas are touched, causing pain after.
Deep breathing exercises, though important for recovery, can make the pain worse. This is because they put extra pressure on the surgical site and tissues. Chest tubes and the healing incision also add to the discomfort when breathing deeply.
Techniques to Minimize Breathing Discomfort
To ease breathing pain after thoracic surgery, several methods can help. Proper pain management is key, as it makes deep breathing exercises easier. It’s important to work with your healthcare team to adjust your pain plan as needed.
- Practice deep breathing exercises regularly to help improve lung expansion and reduce the risk of complications like pneumonia.
- Use pillow support or splinting to reduce pain during coughing and deep breathing by holding a pillow firmly against your chest.
- Engage in physical therapy to improve your overall recovery and learn exercises tailored to your condition.
By using these techniques and talking openly with your healthcare providers, you can lessen breathing discomfort. This helps make your recovery smoother.
Incision and Nerve Pain Following Surgery
Surgical incisions and nerve damage are big causes of pain after thoracic surgery. It’s key to know what makes pain after surgery.
Intercostal Nerve Damage
Intercostal nerve damage is a common issue after thoracic surgery, causing ongoing pain. Intercostal nerves are between the ribs and can get hurt during surgery. This leads to nerve pain.
- Pain characteristics: sharp, stabbing, or burning sensations
- Factors influencing nerve damage: surgical technique, rib spreading, and individual anatomical variations
Surgical Wound Healing Discomfort
The healing of surgical wounds can also cause pain. Patients might feel anything from mild discomfort to severe pain as they heal.
The healing process includes inflammation, tissue repair, and nerve regeneration. These steps can make patients feel pain.
It’s very important to manage pain well during this time. This helps patients feel better and recover faster.
Long-Term Nerve Pain Considerations
Some people may have nerve pain for a long time after thoracic surgery. This can happen for many reasons, like how much nerve damage there was and how much pain a person can handle.
It’s important to understand the chance of long-term nerve pain. We work with patients to keep an eye on their pain and change treatment plans if needed.
Managing long-term nerve pain involves:
- Regular check-ups to watch pain levels
- Changing medication plans as needed
- Trying other pain management methods, like physical therapy or nerve blocks
Pain After Thoracic Surgery: Timeline and Duration
After thoracic surgery, patients often wonder about the recovery timeline and pain duration. Knowing the pain timeline is key for managing expectations and planning the recovery.
First Week Post-Surgery
The first week after thoracic surgery is usually the most painful. Patients feel a lot of discomfort due to the surgical incision and chest tubes. It’s important to manage pain well during this time, often with opioid medications.
In the initial days, patients are closely watched in the hospital for pain, breathing issues, and other complications. The pain is usually at its worst in the first 48-72 hours. It starts to get better as the patient recovers.
Weeks 2-4 Recovery Period
As patients move into weeks 2-4, the pain starts to lessen. But some discomfort may stay, mainly with deep breathing, coughing, or movement. Patients are advised to keep using pain management strategies, possibly switching to non-opioid options.
During this time, patients are encouraged to slowly increase their physical activity. This can help reduce pain and improve recovery. If ongoing pain is a problem, it’s important to talk to the healthcare provider to adjust the pain management plan.
Long-Term Pain Resolution
For most, significant pain reduction happens within the first month after surgery. But some may have lingering pain that can last months. The time it takes for pain to fully resolve varies, depending on the surgery type, overall health, and any complications.
Long-term pain is often managed with a mix of medication, physical therapy, and other non-medication strategies. It’s vital for patients to work closely with their healthcare team to manage any ongoing pain issues.
| Recovery Stage | Typical Pain Level | Recommended Pain Management |
| First Week | Severe | Opioid medications, rest |
| Weeks 2-4 | Moderate | Transition to non-opioid alternatives, gradual increase in physical activity |
| Long-Term | Mild to None | Non-pharmacological strategies, physical therapy, medication as needed |
Understanding the pain timeline after thoracic surgery helps patients prepare for their recovery. Knowing what to expect allows patients to better manage their pain and work with their healthcare providers for a smoother recovery.
Medication Options for Pain Control
Managing pain after thoracic surgery is key. It helps patients feel better, recover faster, and avoid complications.
Opioid Pain Medications
Opioids are used for severe pain after surgery. They work by binding to receptors in the brain and spinal cord. This reduces pain perception.
Common Opioid Medications:
- Morphine
- Fentanyl
- Oxycodone
- Hydrocodone
While effective, opioids can cause serious side effects. These include breathing problems, constipation, and addiction risk.
Non-Opioid Alternatives
To avoid opioid risks, non-opioid options are used more. These include:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) like ibuprofen and naproxen
- Acetaminophen
- Gabapentinoids for neuropathic pain
These medications can be used alone or with opioids. They help manage pain and reduce opioid doses.
Balancing Pain Relief and Side Effects
Finding the right balance between pain relief and medication side effects is important. Healthcare providers and patients work together to find this balance.
| Medication Type | Examples | Benefits | Side Effects |
| Opioids | Morphine, Fentanyl | Effective for moderate to severe pain | Respiratory depression, constipation, dependency |
| NSAIDs | Ibuprofen, Naproxen | Reduces inflammation, pain relief | Gastrointestinal issues, kidney strain |
| Acetaminophen | Tylenol | Pain relief, fever reduction | Liver damage (with overdose) |
Knowing about different medications helps patients manage their pain better. This leads to a more comfortable recovery.
Regional Anesthesia Techniques for Thoracic Pain
Managing pain after thoracic surgery is key. Regional anesthesia is a promising method. It numbs a specific area to block pain signals, avoiding the side effects of other pain meds.
Epidural Analgesia Benefits
Epidural analgesia is a common method for managing thoracic surgery pain. It involves injecting medication into the space around the spinal cord. This blocks pain signals from the chest area.
The benefits include:
- Effective pain relief for both rest and movement
- Reduced need for systemic opioids, minimizing side effects
- Improved respiratory function due to better pain control
Nerve Blocks for Targeted Relief
Nerve blocks are another technique for targeted pain relief. They involve injecting local anesthetic around specific nerves. This blocks pain signals from the surgical site.
This method is great for procedures with well-defined nerve distributions.
Duration and Effectiveness of Regional Techniques
The effectiveness of regional anesthesia varies. It depends on the surgery type, technique, and patient factors. Epidural analgesia can last several days, while nerve blocks may last shorter.
Healthcare providers closely monitor these techniques. They ensure patients get the best pain management.
Using epidural analgesia and nerve blocks helps patients with thoracic surgery. These methods offer effective pain relief with fewer side effects. They are part of a tailored pain management plan for each patient.
Non-Pharmacological Pain Management Strategies
Non-pharmacological strategies are key in managing pain after thoracic surgery. They work alongside medication to help patients recover better.
Physical Therapy Approaches
Physical therapy is vital in pain management. It includes gentle exercises and stretches to boost mobility and cut down pain. Physical therapists create personalized plans for safe and effective recovery.
Some common physical therapy methods are:
- Breathing exercises to better lung function
- Gentle stretching to increase flexibility
- Strengthening exercises to support chest and back muscles
Positioning and Movement Techniques
Right positioning and movement greatly affect pain levels after thoracic surgery. Frequent position changes and gentle mobilization can lessen pain and prevent issues like deep vein thrombosis.
Patients should:
- Change positions often, even in bed
- Use pillows or cushions for support and comfort
- Slowly increase mobility as advised by healthcare providers
Cold/Heat Therapy Applications
Cold and heat therapy are simple yet effective for pain management. Cold therapy reduces inflammation and numbs pain. Heat therapy relaxes muscles and boosts blood flow.
When using cold or heat therapy, remember to:
- Follow the recommended duration and frequency
- Use a barrier between the skin and the cold/heat source to avoid tissue damage
- Monitor skin response and adjust therapy as needed
By using these non-pharmacological pain management strategies, patients can lessen their need for pain medication. This can improve their overall recovery experience.
Psychological Aspects of Managing Thoracic Surgery Pain
Understanding the psychological side of pain management is key for thoracic surgery patients. Pain is not just physical but also influenced by our minds.
Anxiety and Pain Perception
Anxiety greatly affects how we feel pain after thoracic surgery. High anxiety can make pain worse, creating a tough cycle to break. Effective anxiety management is vital for pain control.
Using cognitive-behavioral therapy (CBT) and relaxation can lower anxiety. This can also reduce pain levels for patients.
Mindfulness and Relaxation Techniques
Mindfulness and relaxation are powerful tools for pain management. Mindfulness meditation and deep breathing exercises help reduce stress and promote relaxation. This aids in pain control.
- Mindfulness meditation helps patients stay in the present, reducing pain worries.
- Deep breathing exercises relax the body and lower pain perception.
- Progressive muscle relaxation releases tension, helping with pain relief.
Setting Realistic Pain Expectations
It’s important to set realistic pain expectations after thoracic surgery. Patients should know some pain is normal and how to manage it.
Understanding that pain is part of recovery but manageable helps patients cope better. Clear communication between healthcare providers and patients is essential for setting these expectations.
In conclusion, managing thoracic surgery pain’s psychological side is as critical as the physical. Addressing anxiety, using mindfulness and relaxation, and setting realistic pain expectations help patients through their recovery.
When Pain Becomes Chronic After Thoracic Surgery
For some, thoracic surgery can cause chronic pain that lasts long after recovery. This pain can really affect a person’s life, making it key to know why it happens and how to handle it.
Post-Thoracotomy Pain Syndrome
Post-thoracotomy pain syndrome (PTPS) is chronic pain after thoracic surgery. It happens when the chest wall is cut, like in a thoracotomy. This pain lasts more than two months.
The exact reason for PTPS is not known, but nerve damage during surgery is thought to play a part. Things that might lead to PTPS include:
- Nerve injury during surgery
- Intercostal nerve damage from the incision or rib spreading
- Formation of neuromas at nerve injury sites
Treatment Options for Persistent Pain
Dealing with chronic pain after thoracic surgery needs a variety of approaches. Treatment might include:
- Medications: Anticonvulsants, antidepressants, and opioids can help manage pain. But, opioids are used carefully because of dependency risks.
- Nerve Blocks: Injecting local anesthetics or steroids around nerves can help.
- Physical Therapy: Gentle exercises and therapy can improve mobility and lessen pain.
- Alternative Therapies: Acupuncture, massage, and cognitive-behavioral therapy can also be helpful.
It’s vital for those with chronic pain after thoracic surgery to team up with their healthcare team. Together, they can create a pain management plan that works for the patient.
Special Considerations for Different Thoracic Procedures
Different thoracic surgeries face unique pain management challenges. The surgery type, approach, and patient condition are key factors. They help decide the best pain management plan.
Lung Resection Pain Management
Lung resection surgery involves removing part of the lung. It requires careful pain management due to possible significant pain after surgery. Effective pain control is vital for deep breathing and coughing. These actions help prevent complications like pneumonia.
- Multimodal analgesia, combining different pain relief medications, is often used.
- Regional anesthesia techniques, such as epidural analgesia, can provide significant pain relief.
Cardiac Surgery Pain Differences
Cardiac surgery, like coronary artery bypass grafting (CABG), has its own pain management needs. The surgery’s approach can impact pain levels.
Pain after cardiac surgery can vary based on the incision site and cardiopulmonary bypass use. Effective pain management is key to reduce stress and aid recovery.
- Pain management strategies may include opioid and non-opioid medications.
- Some patients may benefit from regional anesthesia techniques.
Esophageal Surgery Pain Challenges
Esophageal surgery, like that for esophageal cancer, has unique pain management challenges. The esophagus’s delicate nature requires precise surgery.
Post-operative pain can be high due to the surgery’s location and extent. Pain management plans are customized for each patient, often combining medication and other therapies.
- Adequate pain control is essential for ensuring proper nutrition and hydration.
- Regional anesthesia and other advanced pain management techniques may be employed.
Communicating About Pain With Your Healthcare Team
Talking openly with your healthcare providers is key to managing pain after thoracic surgery. It’s a team effort to manage your pain well.
To get the best care, you must tell your healthcare team about your pain. Use pain scales and report any pain symptoms that worry you.
Using Pain Scales Effectively
Pain scales help measure your pain. They let your healthcare team know how bad your pain is. Then, they can change your treatment plan.
- Rate your pain from 0 to 10, with 0 being no pain and 10 being the worst.
- Keep your pain rating the same to track changes.
- Think about how pain affects your daily life when rating it.
Accurate pain assessment is key to a good pain management plan. Patients should tell their pain levels clearly.
When to Report Concerning Pain Symptoms
It’s important to know when to tell your healthcare team about pain symptoms. Look out for:
- Pain that gets worse or doesn’t go away with medicine.
- Pain that makes it hard to breathe deeply or cough.
- New or strange pain feelings.
Telling your healthcare team about these symptoms quickly helps them adjust your pain plan. Working together, you can control your pain better and recover faster.
Talking about pain is more than just reporting it. It’s about working with your healthcare team to find the best pain management strategies. By using pain scales and reporting symptoms, you help your recovery.
Conclusion
Managing pain well is key to a smooth recovery after thoracic surgery. We’ve looked at the different types of surgeries, the pain they cause, and how to handle it. This includes understanding the pain scale and knowing what affects pain levels.
Using a mix of medicines, local anesthesia, and other methods is important. It helps reduce pain and aids in healing. This approach is vital for a good recovery.
For the best recovery, it’s important to tackle pain from all angles. Talk openly with your healthcare team about your pain. Use pain scales and report any unusual symptoms. This way, you can get the best care possible.
FAQ
What is the typical pain level after thoracic surgery?
Pain levels after thoracic surgery vary. Patients use a mix of medicines and other methods to manage it. Knowing the pain scale used helps patients understand what to expect.
How long does pain last after thoracic surgery?
Pain after thoracic surgery can last different lengths of time. Most see big improvements in the first few weeks. But, some might face long-term pain, needing ongoing care.
What are the most effective pain management strategies after thoracic surgery?
Good pain management includes using both opioid and non-opioid drugs. Also, regional anesthesia and non-medical methods like physical therapy help. These strategies work together to control pain.
How can I manage pain from chest tubes and drainage devices?
To manage pain from chest tubes, use pain meds and find comfortable positions. Relaxation techniques also help. Always talk to your healthcare team about your pain.
Why does deep breathing hurt after thoracic surgery?
Deep breathing can hurt because of the surgery cut and nerve irritation. Using diaphragmatic breathing and incentive spirometry can ease this pain.
What are the risks of nerve damage during thoracic surgery?
Nerve damage, like to the intercostal nerves, is a risk. It can cause long-term pain, numbness, or tingling. It’s important to talk about these risks with your surgeon.
Can I use non-opioid alternatives for pain management after thoracic surgery?
Yes, you can use non-opioid options like NSAIDs, acetaminophen, and gabapentin. They can help reduce opioid use and side effects.
How do regional anesthesia techniques work for thoracic pain?
Techniques like epidural analgesia and nerve blocks block pain signals. They provide targeted relief, making them effective for thoracic surgery pain.
What is post-thoracotomy pain syndrome, and how is it treated?
Post-thoracotomy pain syndrome is chronic pain after thoracic surgery. Treatment includes medicines, nerve blocks, and other methods to manage pain.
How can I effectively communicate my pain to my healthcare team?
Use pain scales, keep a pain diary, and report any symptoms to your team. This helps them tailor pain management to your needs.
Are there any special considerations for pain management after different types of thoracic surgery?
Yes, each type of thoracic surgery has its own pain management needs. Knowing these differences is key to effective pain control.
What role does psychological support play in managing pain after thoracic surgery?
Psychological support, like mindfulness and relaxation, is vital. It helps reduce anxiety and improves pain tolerance after thoracic surgery.
References
- Yoon, S. H., et al. (2023). Correlation between pain intensity and quality of recovery after video-assisted thoracoscopic surgery for lung cancer resection. Journal of Pain Research, 16, 2985-2995. https://pubmed.ncbi.nlm.nih.gov/37808464/