Pelvic organ prolapse affects millions of women worldwide. Prolapse surgery is a common treatment. It’s important to understand the recovery process and necessary precautions for a smooth recovery. Long-term restrictions after prolapse surgery including lifting limits. Essential tips for preventing recurrence and healing.
After prolapse repair, patients often wonder about long-term restrictions. These restrictions help ensure the surgery’s success and prevent complications. We’ll guide you through what to expect during your recovery and the precautions you need to take.
Key Takeaways
- Understanding the recovery process is key for a smooth and effective recovery.
- Certain activities may be restricted after prolapse surgery.
- Following the recommended long term restrictions can prevent complications.
- A successful prolapse repair requires patience and following post-operative instructions.
- Our goal is to provide a detailed guide to support your recovery journey.
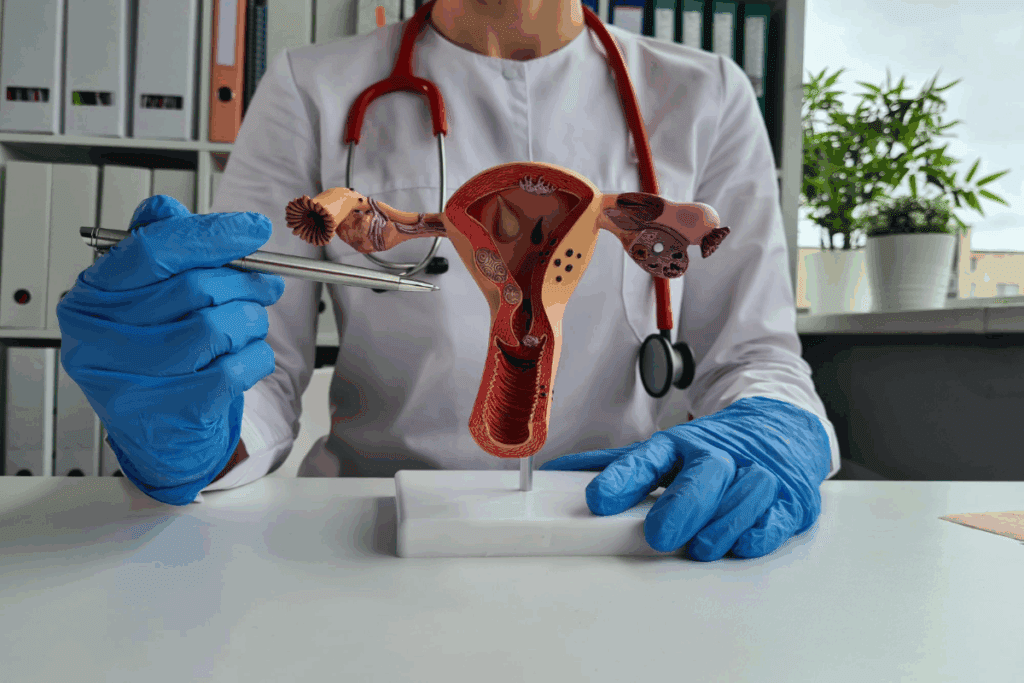
Understanding Pelvic Organ Prolapse and Surgical Interventions

Pelvic organ prolapse happens when muscles in the pelvis get weak. This makes the organs drop into the vagina. It can really affect a woman’s life, so surgery is often needed to fix it.
Common Types of Pelvic Organ Prolapse
There are a few main types of pelvic organ prolapse. Each one is named after the organ affected. The most common ones are:
- Cystocele: When the bladder bulges into the vagina.
- Rectocele: When the rectum bulges into the vagina.
- Uterine prolapse: When the uterus slips out of its normal position.
These problems usually come from weak pelvic muscles and tissue. This can happen because of childbirth, aging, or other reasons.
When Surgery Becomes Necessary
Surgery is an option when prolapse really affects daily life and other treatments don’t help. The choice to have surgery depends on how bad the symptoms are and the patient’s health.
Different Surgical Approaches for Prolapse Repair
There are different ways to fix prolapse through surgery. These include:
- Native Tissue Repair: This method uses the patient’s own tissue to fix the prolapse.
- Mesh Repair: This uses a synthetic mesh to support the prolapsed organ.
- Sacrocolpopexy: A procedure that attaches the prolapsed organ to a stable part inside the pelvis.
Each method has its own good points and things to think about. The right choice depends on the case and what the patient wants.
“The choice of surgical technique depends on the type and severity of the prolapse, as well as the patient’s health status and preferences.”
Immediate Post-Operative Recovery Period
Prolapse surgery starts a critical recovery time. It’s important to manage it well. The days and weeks after surgery are key for healing and avoiding problems.
Hospital Stay and Early Recovery
The hospital stay after surgery is usually short. It can last from a few hours to a couple of days. This depends on the surgery’s complexity and the patient’s health.
While in the hospital, doctors watch over the patient closely. They manage pain and look for any signs of trouble.
When you go home, rest, drink plenty of water, and follow your doctor’s instructions carefully.
Managing Pain and Discomfort
Managing pain well is important after surgery. Stick to the pain plan your doctor gives you. This might include medicine, ice packs, or relaxation techniques.
If your pain gets worse or is very bad, tell your doctor right away. This could mean there’s a problem.
Initial Movement Restrictions
Right after surgery, you’ll need to avoid certain movements. This includes heavy lifting, bending, and hard activities.
Following these rules helps prevent problems and makes sure the surgery works.
| Activity | Immediate Post-Op Recommendation |
| Heavy Lifting | Avoid for at least 4-6 weeks |
| Bending or Straining | Minimize for 2-3 weeks |
| Strenuous Exercise | Avoid for 6-8 weeks |
By managing the early recovery well, patients can have a better outcome. They can also get back to normal activities smoothly.
The First Six Weeks: Critical Recovery Phase
After prolapse surgery, patients face a critical recovery phase lasting about six weeks. It’s vital to follow specific guidelines to ensure proper healing and avoid complications.
Essential Movement Limitations
In the first six weeks, it’s key to avoid heavy lifting, bending, and strenuous activities. Limiting movement helps prevent strain on the surgical site, promoting effective recovery.
- Avoid heavy lifting over 10-15 pounds
- Minimize bending or straining
- Refrain from strenuous exercise or activities
Lifting Restrictions (Weight Limits)
Lifting heavy objects can stress the pelvic floor, potentially causing complications. We advise against lifting anything heavier than 10-15 pounds during the initial six-week recovery period.
- Use assistance when lifting or moving heavy objects
- Keep frequently used items at waist level to avoid bending
- Consider using tools or devices that can help with lifting
Sitting and Sleeping Positions
Proper sitting and sleeping positions are key to recovery. We recommend maintaining a comfortable and supportive posture to reduce strain on the pelvic area.
- Use a supportive chair with proper lumbar support when sitting
- Avoid crossing legs or ankles, which can restrict blood flow
- Consider using a wedge pillow to support your back while sleeping
By following these guidelines, patients can improve their recovery outcomes. It’s also important to follow your healthcare provider’s specific instructions. They may have additional recommendations based on your individual needs.
Long Term Restrictions After Prolapse Surgery
After prolapse surgery, knowing the long-term rules is key for a good recovery. These rules help the healing and keep the surgery’s results lasting.
Physical Activity Limitations Beyond Six Weeks
The first six weeks after surgery are very important. But, some activity limits might last longer. Avoid high-impact activities like running or jumping.
Start with low-impact activities like walking or swimming. But, always listen to your body. It’s important to stay active but not too much.
Permanent Lifting Constraints
One important guideline is to avoid lifting objects heavier than 25 pounds to protect the pelvic floor.We tell patients to never lift more than 25 pounds. This rule helps keep the pelvic floor safe and supports the surgery’s success.
| Lifting Guidelines | Weight Limit | Recommended Frequency |
| Light Lifting | Less than 10 pounds | Occasional |
| Moderate Lifting | 10-25 pounds | Rare |
| Heavy Lifting | More than 25 pounds | Avoid |
Impact on Daily Living
The rules after surgery can change daily life. Simple tasks like grocery shopping or laundry might need to be done differently. Look into ergonomic tools and methods to make daily tasks easier.
By following these rules, patients can have a successful recovery and a better life after surgery.
Returning to Exercise: Safe Approaches
After prolapse surgery, it’s important to start exercising carefully. Physical activity helps regain strength and health. But, it’s key to be cautious.
When looking at safe exercises, we must know which ones are good and which to avoid. A good exercise plan can prevent future prolapse problems and boost your health.
Walking and Low-Impact Activities
Walking is a great low-impact activity to start soon after surgery. Begin with short walks and slowly increase the distance and time. Swimming or cycling are also good when your doctor says it’s okay.
- Start with short walks (5-10 minutes) and gradually increase the duration.
- Avoid high-impact activities, such as running or jumping, for several weeks.
- Consider incorporating gentle stretching exercises to improve flexibility.
Pelvic Floor-Safe Exercises
Pelvic floor exercises, or Kegels, are key for strengthening pelvic muscles. To do Kegels right:
- Identify the correct muscles by stopping the flow of urine mid-stream.
- Contract these muscles for 5-10 seconds, then release.
- Repeat the exercise 10-15 times, three times a day.
Other safe exercises include:
- Gentle core strengthening exercises, such as planks or bridges.
- Low-impact aerobics, like dancing or tai chi.
- Yoga or Pilates exercises that focus on controlled movements and breathing.
Exercises to Avoid Permanently
Some exercises can harm the pelvic floor and should be avoided. These include:
- High-impact activities, such as heavy lifting or bending.
- Exercises that involve straining or bearing down, like heavy weightlifting.
- Activities that cause significant pressure on the pelvic floor, such as trampolining or horseback riding.
Knowing which exercises to avoid and doing safe, low-impact activities helps in a healthy recovery. It also lowers the chance of future prolapse problems.
Sexual Activity Following Prolapse Surgery
Many women wonder when it’s safe to start sex again after prolapse surgery. The recovery time is key, and sex is important in many relationships. Knowing when to start sex again can help make recovery better and more enjoyable.
When It’s Safe to Resume Intimacy
Doctors usually say wait 6 to 8 weeks before starting sex again. This lets the tissues heal and lowers the chance of problems. But, how long you wait can depend on your surgery and how you heal.
It’s very important to listen to your surgeon about when to start sex again. They will check how you’re doing and give advice just for you. It’s important to listen to your body and not rush.
Potential Changes and Adjustments
Some women might notice changes in sex after surgery. These can be vaginal dryness, less feeling, or pain during sex. These changes are often short-term but can last for some.
To help with these issues, try different lubricants for dryness. Talk to your doctor about any pain or discomfort. They can help find ways to make sex better for you.
Addressing Discomfort and Concerns
If you feel pain or discomfort during sex, it’s important to talk about it. Open up with your partner about how you feel. This helps both of you understand each other better.
Talking to your doctor can also help figure out if the pain is from the surgery or something else. They can suggest treatments to help you enjoy sex again.
Starting sex again after surgery needs patience, understanding, and talking with your doctor and partner. By knowing what changes might happen and taking steps to fix them, you can have a good recovery.
Household Activities and Daily Living Adjustments
Recovering from prolapse surgery means making smart changes to your daily life. We’ll show you how to adjust your routine for safety and comfort. This will help you recover smoothly.
Housework Modifications
After surgery, it’s key to do lighter housework to protect your pelvic floor. Light tasks like dusting or folding laundry are okay. But, avoid heavy lifting, bending, or hard work.
Break big tasks into smaller ones. Take breaks often to rest. This helps your body heal.
For cleaning or cooking, use ergonomic tools to ease the strain. A mop with a long handle or a stool for standing can help a lot.
Ergonomic Considerations
Making your home ergonomic is important for recovery. Arrange your space to avoid straining your body. This means no heavy lifting, bending, or reaching.
Keep often-used items at waist level to avoid bending. Use a supportive chair for tasks to keep good posture and avoid pain.
Tools and Techniques for Safer Movement
Using safe movement techniques is key to avoid injury. Learn to lift right, bending at the knees, not the waist. Also, avoid twisting.
Tools like grabber reachers make picking up things easier. Adaptive equipment can also help with daily tasks without strain.
By making these changes and listening to your body, you can get through recovery more comfortably.
Returning to Work and Travel Considerations
Prolapse surgery starts a healing journey. It includes getting back to work and daily activities. The recovery time varies based on surgery type and health.
Timeline for Different Occupations
The time to return to work depends on the job. Desk jobs might allow return in 4 to 6 weeks. Jobs needing heavy lifting or bending may take 8 to 12 weeks or more.
It’s wise to talk to a healthcare provider. They can help figure out the best time to go back to work based on your job and healing.
Workplace Accommodations
When returning to work, some might need to adjust their workspace. This could mean ergonomic changes to ease pelvic area strain. Discussing these needs with your employer and healthcare provider is a good idea.
Small changes, like taking breaks and avoiding heavy lifting, can help a lot. They can keep you comfortable and prevent problems.
Driving and Long-Distance Travel
Driving after surgery should wait until you’re off narcotic pain meds. You should be able to stop quickly without pain. This usually takes 2 to 4 weeks, but it can vary.
For long trips, wait until you’re fully healed, usually 6 to 8 weeks after surgery. Always take breaks to stretch and move. This helps avoid blood clots and discomfort.
Understanding your recovery and planning ahead helps you safely return to work and travel. This way, you can enjoy the benefits of your surgery for a long time.
Swimming and Water-Based Activities After Surgery
For those recovering from prolapse surgery, knowing when to start swimming again is key. Swimming is a low-impact activity that can help during recovery. But, it’s important to follow guidelines for a safe return to water activities.
Timeline for Returning to Swimming
The time to start swimming again varies based on recovery and surgery type. Generally, patients should wait 6 to 8 weeks before swimming or doing water activities. This time allows the area to heal and lowers the risk of infection.
Always listen to your healthcare provider’s advice. They can give you personalized guidance based on your situation.
Benefits of Water Therapy
Water therapy, like swimming, has many benefits during recovery. Water’s buoyancy eases the body’s stress, allowing for gentle exercise. It can also reduce pain and swelling, helping you recover faster.
- Improves circulation
- Enhances muscle relaxation
- Supports joint mobility
Precautions for Water Activities
When you start swimming or water activities again, take precautions. Make sure the water is clean to avoid infections. Also, avoid diving or jumping, as they can stress the pelvic area.
Begin with gentle movements and slowly increase the intensity as you get stronger.
Managing Bowel and Bladder Function Long-Term
Prolapse surgery patients need to focus on managing their bowel and bladder for the best long-term results. Keeping these functions in check is key to avoiding problems and making recovery smoother.
Preventing Constipation
Constipation is a common problem after prolapse surgery. Eating a diet full of fiber, like fruits, veggies, and whole grains, helps. Drinking enough water is also important, as it makes stool softer and helps with regular bowel movements. Try to drink at least eight glasses of water a day.
In some cases, a doctor might suggest a stool softener or fiber supplement to fight constipation. Creating a regular bowel routine, like trying to go at the same time each day, is also helpful.
Bladder Management Strategies
Managing the bladder is very important after prolapse surgery, as some might face urinary incontinence or trouble emptying the bladder. Doing pelvic floor exercises, like Kegels, can help strengthen the muscles that control the bladder.
- Find the right muscles by stopping urine flow mid-stream.
- Do Kegel exercises by tightening these muscles, holding for five seconds, then releasing.
- Do this 10-15 times, three times a day.
When to Consult Your Doctor
Knowing when to see a doctor for bowel or bladder issues is key. If you have persistent constipation, urinary retention, or painful urination, talk to your doctor. Also, seek help right away if you have signs of infection, like fever or bad-smelling discharge.
By following these tips and staying in touch with your healthcare team, you can manage your bowel and bladder long-term. This will improve your life after prolapse surgery.
Recommended Exercises for Prolapse Prevention
Exercises are key in recovering from prolapse surgery. They help strengthen the pelvic floor and prevent it from happening again. A good exercise plan can greatly improve pelvic health and lower the chance of future problems.
Pelvic Floor Strengthening Techniques
Strengthening the pelvic floor is vital after prolapse surgery. Kegel exercises are a top choice for this. To do Kegels, squeeze your pelvic muscles like you’re stopping urine flow, hold for a few seconds, and then release. Do this 10-15 times, three times a day.
The bridge pose is also great. It strengthens the pelvic floor and works the core. Lie on your back, knees bent, feet flat, lift your hips up, and squeeze your pelvic muscles as you lift.
Core Stability Exercises
Core stability exercises are important for the pelvic floor and overall core strength. The plank exercise is a good way to work your core. Start in a push-up position, engage your core, and hold for 30-60 seconds.
Pelvic tilts are also helpful. Lie on your back, knees bent, feet flat, tilt your pelvis up, and then back down again. Repeat this 10-15 times.
Breathing Techniques for Support
Breathing techniques can also support the pelvic floor. Diaphragmatic breathing involves deep breathing into your diaphragm. Lie on your back, breathe in deeply through your nose, letting your abdomen rise while your chest stays steady.
| Exercise | Description | Repetitions |
| Kegel Exercises | Contract and release pelvic muscles | 10-15, 3 times a day |
| Bridge Pose | Lift hips towards the ceiling | 10-15 |
| Plank Exercise | Hold a push-up position | 30-60 seconds |
| Pelvic Tilts | Tilt pelvis upwards and back down | 10-15 |
| Diaphragmatic Breathing | Breathe deeply into the diaphragm | 5-10 minutes |
Emotional and Psychological Aspects of Recovery
Healing after prolapse surgery is not just about the body. It’s also about the mind and emotions. Adjusting to the changes takes time and effort.
Managing Expectations and Patience
Managing your expectations and being patient are big challenges. Your daily life might change a lot, which can be tough. Remember, recovery is a slow process.
- Set realistic goals for recovery
- Understand that setbacks are a normal part of the healing process
- Practice patience and self-compassion
Setting goals you can reach and being kind to yourself helps a lot. It makes the recovery journey easier.
Body Image and Self-Perception
Prolapse surgery can change how you see your body. These changes might make you feel less confident or less about yourself.
Strategies for coping with these changes include:
- Focusing on the positive outcomes of the surgery
- Seeking support from loved ones or support groups
- Engaging in activities that promote self-care and well-being
By focusing on the good and getting support, you can start to feel better about yourself again.
Support Resources and Communities
Having the right support is key for your emotional and psychological recovery. This includes doctors, support groups, and online forums.
Some benefits of these resources include:
- Emotional support and understanding
- Practical advice and guidance
- A sense of community and connection
Using these resources can make you feel supported and strong during your recovery.
Long-Term Outcomes and Success Rates
The success of prolapse surgery depends on many factors. It’s important for patients to know what to expect. This helps them understand their recovery and how well the surgery will work.
Factors Affecting Surgical Success
Several things can affect how well prolapse surgery works. These include the type of surgical procedure and the severity of the prolapse. Your overall health and following post-operative instructions also matter.
The surgeon’s experience and the quality of care after surgery are key too. Every patient is different. So, it’s vital to talk to your doctor about how these factors might affect you.
Potential for Recurrence
One worry after surgery is that the problem might come back. The chance of this happening depends on the surgery type and your health. Regular check-ups are important to catch any signs of recurrence early.
To lower the chance of the problem coming back, making lifestyle changes helps. This includes staying at a healthy weight, not lifting heavy things, and doing pelvic floor exercises. These actions can help keep the surgery successful for a long time.
Maintaining Results Over Time
To keep the surgery’s results, you need to make lifestyle changes and sometimes see a pelvic floor therapist. Eating well and exercising regularly is good for your pelvic health.
Also, listen to your body and tell your doctor about any changes or worries. By doing this, you can get the most out of your surgery and improve your life quality.
Signs of Complications or Surgical Failure
It’s important for patients who have had prolapse surgery to know the signs of complications or failure. The surgery aims to fix the prolapse. Knowing about possible issues helps in getting medical help quickly.
Warning Symptoms to Monitor
After prolapse surgery, watch out for certain symptoms. These include persistent pain, severe vaginal bleeding, fever, or trouble urinating. It’s vital to watch these symptoms closely and talk to your healthcare provider if you notice them.
Also, if you have leg pain or swelling, it could mean a blood clot. Seeking medical help right away can stop serious problems.
When to Seek Immediate Medical Attention
If you have heavy vaginal bleeding that soaks more than one pad an hour, severe abdominal pain, or trouble controlling urination, get help fast. These could be signs of serious issues that need quick treatment.
- Severe vaginal bleeding
- Abdominal pain
- Difficulty urinating
- Fever above 100.4°F (38°C)
Addressing Recurrent Prolapse
In some cases, prolapse can come back after surgery. If you feel a heaviness in the pelvis, see vaginal bulging, or have trouble controlling your urine, see your doctor. Getting help early can manage recurrent prolapse well.
Knowing the signs of complications or surgical failure helps patients take charge of their recovery. By watching for warning symptoms and knowing when to get medical help, patients can reduce risks and get the best results from prolapse surgery.
Lifestyle Modifications for Long-Term Success
After prolapse surgery, making lifestyle changes can greatly help. These changes support the surgery’s success and improve overall health.
Weight Management Strategies
Keeping a healthy weight is key to reduce stress on pelvic muscles. A balanced diet and gentle exercise are recommended. Even a small weight loss can lower the risk of prolapse coming back.
It’s best to work with a healthcare provider or nutritionist for a weight plan. This plan should fit your health, mobility, and food likes.
Dietary Considerations for Tissue Health
Eating foods rich in nutrients helps heal tissues. More fiber from fruits, veggies, and grains helps avoid constipation after surgery. Drinking enough water keeps tissues elastic and the pelvic floor healthy.
Eating foods like berries and leafy greens boosts health. Foods with vitamin C and zinc help repair tissues.
Smoking Cessation and Other Factors
Stopping smoking is key for better health and fewer surgery complications. Smoking causes chronic coughing, straining pelvic muscles. We offer help to quit smoking.
Other lifestyle changes, like not lifting heavy or managing coughs, are also important. Be careful with your body position and avoid straining the pelvic floor. Regular check-ups with doctors help track progress and solve any issues.
By making these lifestyle changes, patients can greatly improve their long-term results after surgery. It’s about making lasting changes for better health and well-being.
Conclusion: Living Well After Prolapse Surgery
Recovering from prolapse surgery takes time, patience, and a long-term care plan. We’ve talked about the different stages of recovery, from right after surgery to making lifestyle changes. Each step is important for a full recovery.
Knowing the long-term restrictions after prolapse surgery is key. Following these rules helps avoid problems and boosts life quality. This means choosing the right exercises, handling daily tasks, and living a healthy lifestyle.
We urge patients to be active in their prolapse surgery recovery. Listen to your doctor and go to all follow-up visits. This helps the recovery go smoothly and effectively.
It’s possible to live well after prolapse surgery with the right attitude and support. By adjusting and being aware of long-term restrictions, people can see better health and happiness. We’re here to offer full care and advice, helping you get the best results.
FAQ
What are the long-term restrictions after prolapse surgery?
After surgery, you should avoid heavy lifting and bending for weeks to months. The exact time depends on the surgery type and your recovery.
How long does it take to recover from prolapse surgery?
Recovery time varies. Most people take several weeks to a few months to fully heal. Your age, health, and surgery complexity play a role.
Can I push a prolapsed bladder back into place?
You might be able to push a prolapsed bladder back, but it’s not a lasting fix. You need medical help to treat the root cause.
What is the best surgery for prolapsed bladder?
The best surgery depends on your prolapse severity, health, and other factors. Options include cystocele repair, vaginal mesh, and more.
How long does a cystocele repair last?
Repair longevity varies. It depends on the surgery method, your health, and post-op care. Generally, it offers long-term relief.
Can pelvic prolapse cause leg pain?
Yes, pelvic prolapse can cause leg pain. This happens due to pressure on nerves and tissues. Pain severity varies by person.
Is it normal to feel a bulge after prolapse surgery?
Feeling a bulge or pressure is common during healing. But, if it persists or is concerning, talk to your doctor.
How soon can prolapse surgery fail?
Failure timing varies a lot. It depends on surgery type, initial prolapse severity, and post-op care.
Can you have bladder prolapse twice?
Yes, bladder prolapse can recur. Risk depends on surgery type and post-op care.
What are the benefits of water therapy after prolapse surgery?
Water therapy, like swimming, is good for healing. It’s low-impact and strengthens pelvic muscles.
When can I swim after hysterectomy?
Swimming timing after hysterectomy varies. Wait several weeks, as advised by your surgeon.
How long after prolapse surgery can I have sex?
Wait 6 to 12 weeks before sex, as advised by your doctor. Follow their specific guidance.
Does prolapse surgery make you tighter?
Surgery aims to correct prolapse, not tighten vaginas. But, some procedures might improve tone. Effects vary by person.
What are the signs of complications or surgical failure after prolapse surgery?
Look out for persistent prolapse, pain, and urinary or bowel issues. Seek medical help for these symptoms.
How can I manage bowel and bladder function long-term after prolapse surgery?
Eat well, stay hydrated, and practice good bowel habits. Do pelvic floor exercises and follow your doctor’s advice.
Reference:
- MedicalNewsToday: Bladder Emptying and Post-Surgery Recovery ,https://www.medicalnewstoday.com/articles/316706























