Last Updated on November 27, 2025 by Bilal Hasdemir
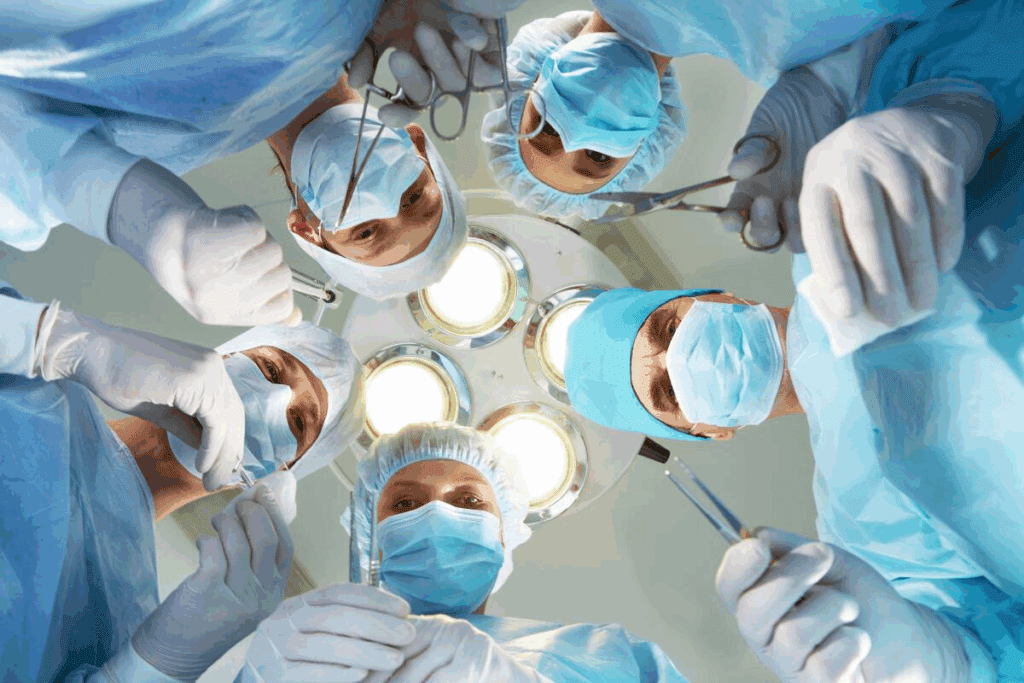
Understanding L4-L5 Spinal Surgery Risks is crucial. Learn how serious the operation is and the precautions taken for a positive outcome.
Degenerative disc disease affects millions of people worldwide, causing significant discomfort and disability. One common treatment for this condition is L4-L5 spinal fusion. This procedure involves removing the damaged disc and fusing the surrounding vertebrae.
This complex surgery is often considered when other treatments have failed to alleviate symptoms. The seriousness of L4-L5 surgery can be understood by examining its risks, complications, and recovery process.
Key Takeaways
- Degenerative disc disease is a common condition that can be treated with L4-L5 spinal fusion.
- L4-L5 spinal fusion involves removing the damaged disc and fusing the surrounding vertebrae.
- The surgery is considered when other treatments have failed to alleviate symptoms.
- Understanding the risks and complications is key for patients considering this surgery.
- The recovery process is vital for the surgery’s overall outcome.
Understanding the L4-L5 Spinal Segment
The L4-L5 spinal segment is key in the lower back. It supports our body’s weight and helps us move.
Anatomy of the L4-L5 Region
The L4-L5 area has a special structure. It includes the intervertebral disc, facet joints, and muscles. The intervertebral disc helps absorb shock, making movement smooth.
The facet joints add support and let us bend and twist. Knowing the L4-L5 anatomy helps doctors diagnose problems.
Function and Importance in Spinal Mechanics
The L4-L5 segment is vital for the spine’s stability and movement. It carries a lot of our body’s weight and helps us move.
Keeping the L4-L5 healthy is important for the spine’s function. Problems like herniated discs or spinal stenosis can cause a lot of pain and trouble.
Common Stress Factors on This Segment
The L4-L5 segment faces many stressors, like mechanical stress and degenerative changes. Degenerative disc disease and spondylolisthesis are common issues. They might need spinal fusion surgery.
| Condition | Description | Potential Treatment |
| Herniated Disc | A condition where the intervertebral disc bulges or ruptures, potentially compressing nerves. | Microdiscectomy, Spinal Fusion |
| Spinal Stenosis | Narrowing of the spinal canal, which can compress nerves and cause pain. | Laminectomy, Spinal Fusion |
| Spondylolisthesis | A condition where one vertebra slips over another, potentially causing nerve compression. | Spinal Fusion, Decompression Surgery |
Common Conditions Requiring L4-L5 Surgery
The L4-L5 spinal segment is often affected by several conditions that might need surgery. This area is key in supporting the spine and allowing for movement. It’s more prone to problems because of this.
Herniated Disc Pathology
A herniated disc happens when the soft center of the disc leaks out. This can irritate nerves, causing pain, numbness, and weakness in the lower back and legs.
Spinal Stenosis at L4-L5
Spinal stenosis is when the spine’s spaces narrow, putting pressure on nerves. At L4-L5, this can cause a lot of discomfort and neurological symptoms.
Degenerative Disc Disease
Degenerative disc disease is when discs lose height and strength over time. This can lead to pain and stiffness in the lower back.
Spondylolisthesis Complications
Spondylolisthesis is when a vertebra slips forward over the one below it. This can cause nerve compression and instability, often needing surgery to fix.
| Condition | Symptoms | Treatment Considerations |
| Herniated Disc | Pain, numbness, weakness in lower back and legs | Microdiscectomy, conservative management |
| Spinal Stenosis | Numbness, weakness, pain in legs, neurogenic claudication | Laminectomy, spinal fusion |
| Degenerative Disc Disease | Pain, stiffness in lower back | Spinal fusion, artificial disc replacement |
| Spondylolisthesis | Nerve compression symptoms, instability | Spinal fusion, decompression |
Understanding these common conditions and their treatments helps patients make informed decisions about L4-L5 surgery.
When Surgery Becomes Necessary
When other treatments don’t work, surgery is often needed for L4-L5 spinal problems. This choice is made after trying everything else. It’s a big decision.
Failed Conservative Treatment Approaches
First, doctors try physical therapy, medicine, and lifestyle changes. But if these don’t help, surgery might be next. Failed back surgery syndrome shows how important it is to think carefully about surgery.
Progressive Neurological Deficits
When symptoms get worse, like more numbness or weakness, surgery might be needed. Nerve damage can happen, but surgery can also help. It can stop further damage.
Cauda Equina Syndrome
Cauda Equina Syndrome is very serious and needs quick help. It happens when nerves in the lower back get squished. This can cause pain, numbness, and permanent damage if not treated fast. Surgery is often needed to fix this.
Quality of Life Considerations
For many, the choice to have surgery is about their quality of life. Chronic pain and not being able to do everyday things can really hurt a person’s life. If these problems are bad and can’t be fixed with other treatments, surgery might be considered. But, the risks like infection and blood clots must be thought about too.
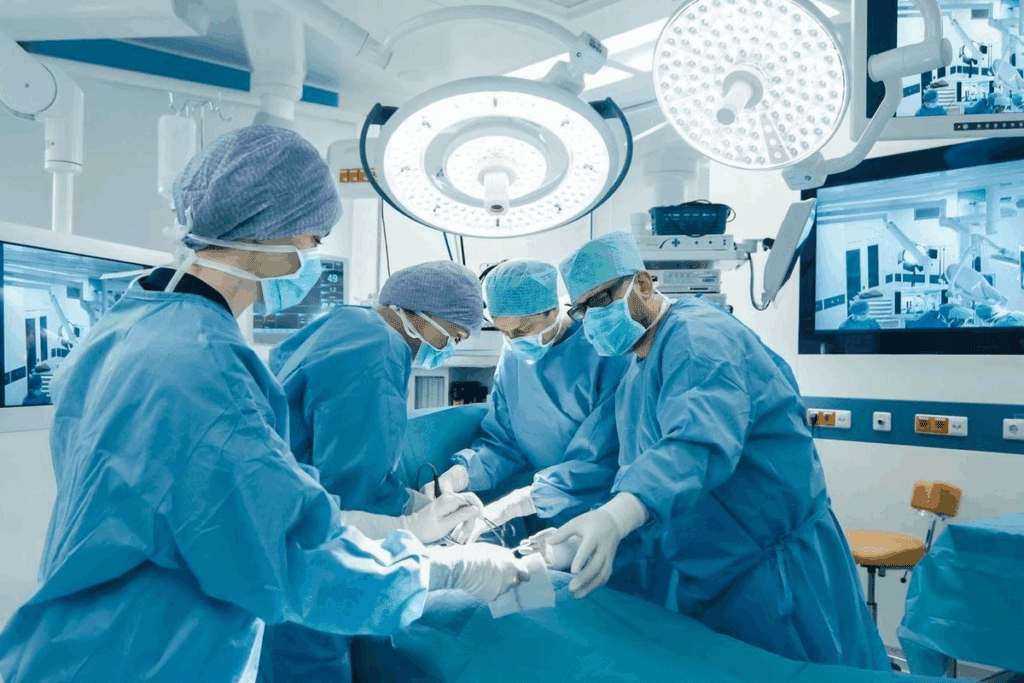
Types of L4-L5 Surgical Procedures

The choice of surgery for L4-L5 depends on the condition, patient’s health, and the surgeon’s skill. Different surgeries can be done on the L4-L5 segment. Each one is designed to fix specific spinal problems.
Microdiscectomy Techniques
Microdiscectomy is a small surgery for herniated discs. It removes the damaged disc that’s pressing on nerves. This method is chosen for its accuracy and quick recovery.
Laminectomy Procedures
A laminectomy removes part of the vertebrae to ease pressure on nerves. It’s often used for spinal stenosis.
Spinal Fusion Methods
Spinal fusion joins two or more vertebrae together. Bone grafts and sometimes hardware like screws are used. It treats conditions like degenerative disc disease and spondylolisthesis.
Artificial Disc Replacement Options
Artificial disc replacement replaces the damaged disc with an artificial one. It aims to keep the spine mobile and reduce pain.
Each surgery has its own use, benefits, and risks. The right surgery depends on a detailed look at the patient’s condition and health.
L4-L5 Spinal Surgery Risks
L4-L5 spinal surgery is a big step that comes with risks. These risks can happen right away or later on. It’s important for patients to know about these risks to make good choices about their treatment.
Immediate Postoperative Complications
Right after surgery, patients might face some problems. These can include:
- Anesthesia Risks: Problems with anesthesia, like breathing or heart issues, can happen.
- Postoperative Pain: It’s key to manage pain well, as bad pain can cause more problems.
- Infection: There’s always a chance of infection at the surgery site.
- Bleeding: Too much bleeding during or after surgery is a risk.
Long-Term Structural Complications
Long-term problems can also affect the success of L4-L5 spinal surgery. Some of these issues are:
- Hardware Complications: Problems with the surgical hardware, like it coming loose or breaking, can occur.
- Reoperation: Some patients might need more surgery because of problems or if the first surgery didn’t fully fix the issue.
- Adjacent Segment Disease: Disease in the spinal segments next to the surgery site can be a long-term problem.
To understand the risks and complications better, let’s look at the data in the table below:
| Complication Type | Description | Frequency |
| Anesthesia Risks | Respiratory or cardiac issues related to anesthesia | Low |
| Postoperative Pain | Pain following surgery | Common |
| Hardware Complications | Issues with surgical hardware, such as loosening or breakage | Moderate |
| Reoperation | Need for additional surgery due to complications | Variable |
Risk Factors That Increase Complication Rates
Some things can make complications more likely during or after L4-L5 spinal surgery. These include:
- Age: Older patients might face more risks.
- Pre-existing Conditions: Conditions like diabetes or heart disease can affect how well surgery goes.
- Smoking: Smoking can slow healing and increase risks.
- Obesity: Being overweight can put extra stress on the spine and affect recovery.
Knowing about these risk factors and complications is key for patients and doctors to make smart choices about L4-L5 spinal surgery.
Potential for Nerve Damage During Surgery
Nerve damage is a big worry in L4-L5 spinal surgery. It can happen for many reasons during the surgery. This can lead to serious problems.
Types of Nerve Injuries
There are different kinds of nerve injuries in L4-L5 surgery. These include:
- Neurapraxia: A temporary problem with nerve function.
- Axonotmesis: Damage to the nerve fibers, but the surrounding tissue is okay.
- Neurotmesis: A severe injury where the nerve is completely cut.
Symptoms of Nerve Damage
The symptoms of nerve damage can vary a lot. They depend on the type and how bad the injury is. Common signs include:
- Numbness or tingling in the legs.
- Muscle weakness.
- Pain.
- Loss of reflexes.
Treatment Options for Nerve Complications
Dealing with nerve damage from L4-L5 surgery aims to manage symptoms and help recovery. Treatment options include:
- Physical therapy to boost mobility and strength.
- Medications to control pain and other symptoms.
- In some cases, more surgery might be needed.
Long-Term Prognosis for Nerve Injuries
The outlook for nerve injuries from L4-L5 surgery can vary. Here’s a table showing possible outcomes:
| Type of Nerve Injury | Recovery Time | Potential for Full Recovery |
| Neurapraxia | Days to weeks | High |
| Axonotmesis | Months | Moderate |
| Neurotmesis | Variable, may be incomplete | Low |
It’s important for patients and doctors to know about the risks and possible outcomes of nerve damage in L4-L5 surgery.
Infection and Blood Clot Risks
Patients having L4-L5 surgery might face risks like infection and blood clots. It’s important for both patients and doctors to know about these risks. This helps in managing them well and avoiding complications.
Surgical Site Infection Rates
Surgical site infections (SSIs) are a big worry after L4-L5 surgery. The chance of getting an SSI can change based on many things. These include how the surgery is done, the patient’s health, and how they are cared for after surgery.
Studies show that SSIs in spinal surgery happen in 1% to 5% of cases. Good wound care and using antibiotics before surgery are key to lower SSI risks.
Deep Vein Thrombosis and Pulmonary Embolism
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are serious problems that can happen after L4-L5 surgery. DVT is when blood clots form in deep veins, usually in the legs. PE happens when these clots move to the lungs.
Moving early and using blood thinners are important ways to stop these issues.
Prevention Strategies
To stop infections and blood clots, we need to take many steps. This includes getting patients ready for surgery well, doing the surgery carefully, and taking good care of them after. Patients are told to drink lots of water, move around, and take their medicine to lower these risks.
Treatment Approaches
If infections or blood clots happen, we need to act fast. Infections might need antibiotics or surgery. DVT and PE often need blood thinners. In very bad cases, we might use stronger treatments like thrombolysis.
Hardware Complications in Fusion Procedures
Using hardware in spinal fusion surgery can lead to complications. These issues can affect the surgery’s success and the patient’s life quality.
Implant Failure Mechanisms
Implant failure is a big worry in spinal fusion surgeries. Implant failure mechanisms include material fatigue, wrong sizing, or bad placement. Knowing these can help lower the risk of problems.
Screw Loosening or Breakage
Screw loosening or breakage is common in spinal fusion. It can happen due to stress on the hardware, bad bone quality, or poor screw fixation. Symptoms might include pain, instability, or nerve problems.
Adjacent Segment Disease Development
Adjacent segment disease (ASD) is when the spinal segments next to the fusion site wear out. ASD can cause new pain and nerve issues, needing more surgery.
Revision Surgery Considerations
Revision surgery is needed for hardware issues or ASD. Revision surgery considerations include the surgery’s complexity, the patient’s health, and risks and benefits. Good planning and choosing the right patient are key for success.
In summary, hardware problems in spinal fusion surgeries are a big concern. Understanding these issues and their effects is vital for better patient results.
Patient Selection and Surgical Preparation
Choosing the right patients and preparing them well is key for L4-L5 surgery success. It’s important to evaluate and prepare patients carefully. This helps reduce risks and improve patient outcomes.
Optimal Candidate Criteria
Finding the best candidate for L4-L5 surgery involves a detailed check-up. We look at the patient’s medical history, current health, and how severe their spinal issue is. We consider age, overall health, and any other health problems.
- Age and overall health status
- Severity of spinal condition
- Presence of comorbidities
Preoperative Testing Requirements
Pre-surgery tests are vital. They include blood tests, imaging like MRI and CT scans, and other tests. These help us understand the patient’s health and spot any risks.
| Test Type | Purpose |
| Blood Work | Check overall health and find any issues |
| Imaging Studies | Look at the spinal condition and plan the surgery |
Medication Management Before Surgery
Medication management is very important before surgery. Some medicines might need to be changed or stopped to avoid problems like bleeding or bad reactions with anesthesia.
It’s important for patients to tell their doctor about all medicines they take. This includes supplements and over-the-counter drugs. This helps us make the right choices about medication management before surgery.
Mental Preparation for Major Surgery
Mental readiness is as important as physical readiness. Surgery can be stressful, and a positive attitude can help. Patients should talk about their worries and fears with their doctor.
By making sure patients are both physically and mentally ready, we can improve the chances of a successful surgery and a smooth recovery.
Recovery Timeline and Mobility Limitations
The journey to recovery after L4-L5 surgery is slow and requires patience. It’s important to know the different stages of recovery and how they affect your mobility.
Hospital Stay Expectations
After L4-L5 surgery, you might stay in the hospital for a few days to a week. This depends on the surgery’s complexity and your health. During your stay, doctors will watch over you, manage your pain, and start your rehabilitation.
Early Mobility Restrictions
Right after surgery, you’ll need to move less to heal properly. You should avoid heavy lifting, bending, or twisting. Following these rules is key to avoid problems and recover well.
Gradual Activity Progression
As you get better, you’ll start doing more things with the help of a physical therapist. Your progress will depend on how fast you heal and your overall health.
Return to Work and Daily Activities
When you can go back to work and daily activities varies. It depends on your job and the surgery details. Usually, you can start with light tasks in 6-12 weeks. But, it might take months to fully recover.
| Activity | Expected Timeline | Notes |
| Light Walking | 1-2 weeks | Gradually increase distance and pace |
| Driving | 2-4 weeks | Avoid heavy traffic and long distances initially |
| Returning to Work | 6-12 weeks | Depends on job requirements and physical demands |
Knowing the recovery timeline and following mobility advice are important for a good outcome after L4-L5 surgery. By listening to your healthcare team and being patient, you can have a full and healthy recovery.
Physical Therapy and Rehabilitation Process
Physical therapy is key after L4-L5 surgery. It helps patients get stronger and move better. A good physical therapy plan is vital for recovery, pain control, and better function.
Early Phase Rehabilitation Goals
The first part of rehab aims to lessen pain and swelling. It also works on improving movement and daily skills. Patients start with easy exercises and then do harder ones with a physical therapist’s help.
Progressive Strengthening Protocols
As recovery goes on, the focus shifts to making muscles around the spine stronger. Physical therapists create special exercises for each person. These exercises aim to boost spinal stability and overall health.
Pain Management During Rehabilitation
Managing pain well is very important during rehab. Physical therapists use many methods, like manual therapy and exercises, to control pain. This helps patients recover faster.
Long-Term Maintenance Exercises
Patients are often told to keep up with exercises at home after rehab. These exercises help keep the spine healthy and prevent future problems.
Failed Back Surgery Syndrome
Some patients keep feeling pain even after surgery. This is called failed back surgery syndrome. It’s a big problem in spinal surgery, affecting many patients.
Definition and Prevalence Rates
Failed back surgery syndrome (FBSS) means pain that doesn’t go away after spinal surgery. It happens to a lot of people after they’ve had surgery.
It’s hard to know exactly how many people get FBSS. But it’s clear that it’s a common problem after spinal surgery.
Common Causes of Surgical Failure
Several things can lead to FBSS. These include:
- Choosing the wrong patient for surgery
- Doing the surgery wrong or not fully
- Complications after surgery
- New disc problems or scar tissue
Knowing what causes FBSS helps us find ways to prevent it.
Diagnostic Approaches
To diagnose FBSS, doctors use:
- Looking at the patient’s medical history
- Doing a physical exam to check for pain and nerve issues
- Using MRI or CT scans to see the spine
These steps help find out why the pain is happening and how to treat it.
Management Options After Failed Surgery
Managing FBSS involves:
- Trying pain medicines and physical therapy first
- Using procedures like nerve blocks or spinal cord stimulation
- Considering surgery again if there’s a clear reason
It often takes a team of doctors to help patients with FBSS.
Choosing the Right Surgeon and Getting Second Opinions
Finding the right surgeon for L4-L5 surgery is key. It affects the surgery’s success. You should research well and think about important factors.
Surgeon Qualifications to Consider
There are several things to look at when checking a surgeon’s qualifications. These include:
- Board Certification: Make sure the surgeon is certified by a well-known board, like the American Board of Orthopaedic Surgery or the American Board of Neurological Surgery.
- Experience: Choose surgeons with lots of experience in L4-L5 surgeries.
- Specialization: It’s good to pick surgeons who focus on spinal surgery.
Hospital Quality Metrics
The hospital’s quality is also very important. Look at these metrics:
- Infection Control: Pick hospitals with low infection rates.
- Patient Satisfaction: High patient satisfaction scores mean good care.
- Accreditation: Make sure the hospital is accredited by a trusted organization.
Value of Multiple Surgical Consultations
Getting second opinions from different surgeons is helpful. It gives you a better understanding of the surgery needed and helps you make a good choice.
- Different Perspectives: You’ll get different views on your condition and treatment options.
- Comparing Recommendations: You can compare what each surgeon suggests and pick what’s best for you.
Questions to Ask Before Committing to Surgery
Before deciding on surgery, ask important questions:
- Surgical Experience: How many L4-L5 surgeries has the surgeon done?
- Success Rates: What are the surgeon’s success rates with this surgery?
- Potential Risks: What risks and complications could happen with the surgery?
By thinking about these points and getting opinions from several surgeons, you can make a smart choice for your L4-L5 surgery.
Conclusion
L4-L5 surgery is a complex procedure with various risks and complications. These risks can affect patient outcomes. It’s important to understand these risks when considering spinal fusion or other surgeries.
Patients thinking about L4-L5 surgery need to weigh the benefits against the risks. This helps them make informed decisions about their care. Spinal fusion, a common part of L4-L5 surgery, also needs careful thought about its risks and benefits.
A well-informed patient can better handle the complexities of L4-L5 spinal surgery. By knowing the details of the procedure, individuals can make choices that fit their needs. This can improve their chances of a successful outcome.
FAQ
What is L4-L5 surgery, and what conditions does it treat?
L4-L5 surgery is a procedure on the lower back, focusing on the L4-L5 segment. It treats issues like herniated discs, spinal stenosis, and degenerative disc disease.
What are the risks associated with L4-L5 surgery?
Risks include nerve damage, infection, and blood clots. Other complications are hardware issues and failed back surgery syndrome.
What is the recovery process like after L4-L5 surgery?
Recovery starts with a hospital stay. Then, you’ll have to limit your movement. Gradually, you’ll get back to normal, with physical therapy helping a lot.
How long does it take to recover from L4-L5 surgery?
Recovery time varies. Most people can get back to daily life in weeks to months. Full recovery might take several months.
What is failed back surgery syndrome, and how is it managed?
Failed back surgery syndrome is when you have pain or symptoms after surgery. Management can include more surgery, pain management, or other treatments.
How can I minimize the risk of complications during L4-L5 surgery?
To reduce risks, choose a qualified surgeon and follow instructions. Stick to postoperative care and report any concerns quickly.
What are the benefits of physical therapy after L4-L5 surgery?
Physical therapy helps with recovery, pain management, and improving function. It guides you through a rehabilitation program tailored to your needs.
Can L4-L5 surgery be performed using minimally invasive techniques?
Yes, some procedures, like microdiscectomy, use minimally invasive techniques. This can lead to less recovery time and less tissue damage.
How do I choose the right surgeon for my L4-L5 surgery?
Look for a surgeon with the right qualifications and experience. Consider their success rates and get second opinions. Also, check the hospital’s quality metrics.
What are the signs of potentially complications after L4-L5 surgery?
Watch for severe pain, numbness, weakness, infection signs, or trouble with bowel or bladder control. Seek immediate medical help if you notice these symptoms.
Reference:
This article defines double voiding and its benefits in reducing urinary frequency, including step-by-step instructions and variations. Additional techniques like bladder percussion, running water, and vibration therapy are also reviewed. It stresses medical consultation before trying these techniques.





