Last Updated on November 27, 2025 by Bilal Hasdemir

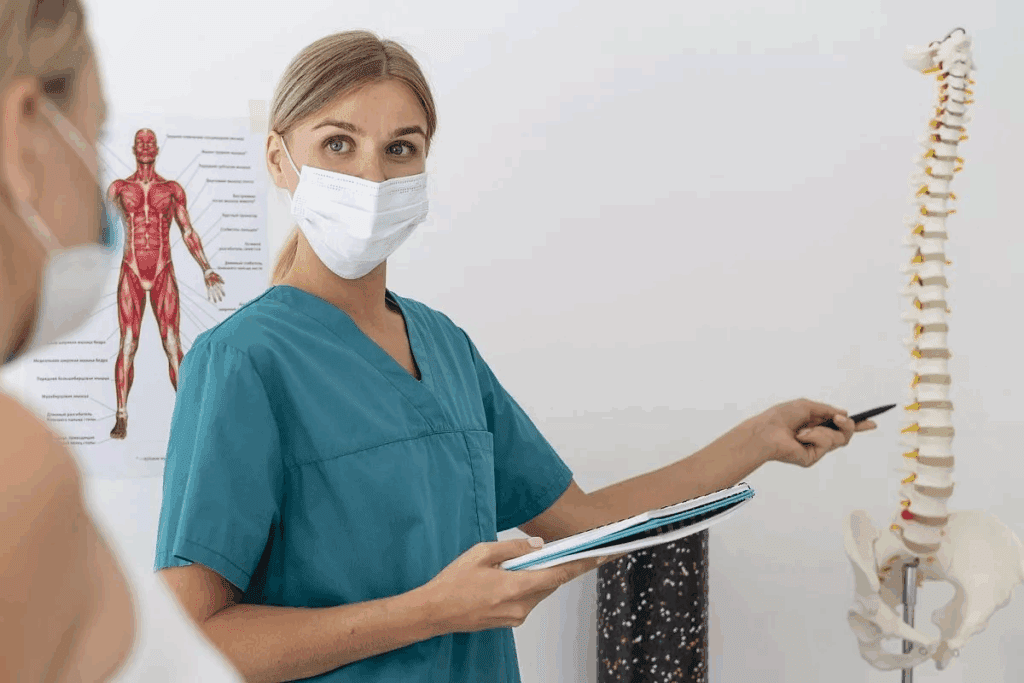
Did you know traditional spine surgery can cause a lot of tissue damage? This leads to long recovery times and more chances of complications. Minimally Invasive Spine Surgery is changing the game with less pain and quicker recovery. The Minimally Invasive Spine Surgery approach is often the easiest and best option. Learn about these amazing procedures for a positive outcome.
We’re seeing a big move towards minimally invasive surgery. This method causes less harm to the surrounding tissues. It means less chance of problems and a quicker get-back-to-normal time. So, more people are feeling okay about trying spine surgery.
Key Takeaways
- Minimally invasive techniques reduce tissue damage and promote faster healing.
- Less pain and quicker recovery times improve patient outcomes.
- Reduced risk of complications makes spine surgery a more viable option.
- Modern spine surgery techniques are designed to minimize recovery time.
- Patients can return to normal activities sooner with minimally invasive surgery.
Understanding Spine Surgery Complexity
Spine surgery complexity comes from many factors. These include the condition being treated and the patient’s body. Spine surgery covers a wide range of procedures. These range from simple to very complex.
Factors That Determine Surgical Difficulty
Several key factors affect the complexity of spine surgery. These include:
- Patient’s Overall Health: Pre-existing medical conditions can greatly impact the surgery’s complexity and the patient’s outcome.
- Nature of the Spinal Condition: The type and severity of the spinal condition being treated are key in determining the surgery’s difficulty.
- Surgeon’s Expertise: The surgeon’s experience and skill are vital for the success and complexity of spine surgery.
- Anatomical Considerations: Each patient’s anatomy can affect the surgery’s complexity.
The Spectrum of Spinal Procedures
Spinal procedures vary in complexity. They range from minimally invasive surgeries to more complex open surgeries. Some common procedures include:
- Minimally Invasive Discectomy: A procedure used to treat herniated discs with minimal tissue damage.
- Spinal Fusion: A surgery that involves fusing two or more vertebrae together to stabilize the spine.
- Laminectomy: A procedure that involves removing part or all of a vertebra to relieve pressure on the spinal cord.
Understanding these factors and the range of spinal procedures is key. It’s important for both medical professionals and patients. Recognizing the complexities of spine surgery helps us appreciate the skill and care needed for successful outcomes.
The Evolution of Minimally Invasive Spine Surgery
Medical technology has led to the creation of minimally invasive spine surgery. This change has made spine surgery less invasive. It offers patients quicker recovery times and fewer complications.
Historical Development
Minimally invasive spine surgery has been around for decades. Early attempts were limited by old technology. But, as imaging and tools got better, so did the surgery options.
“The 1980s saw the start of endoscopic techniques in spine surgery,” says a top expert. This was a big step towards less invasive surgeries. It aimed to cut down recovery times and tissue damage.
Technological Advancements
Technology has been key in making spine surgery less invasive. Better imaging and tools have made these surgeries more precise. Special instruments and retractors let surgeons work through small cuts.
- High-resolution imaging technologies
- Specialized surgical instruments
- Advanced navigation systems
These tech improvements have made spine surgery safer and more effective. They’ve also made it possible to treat more spinal issues.
Current State of Practice
Today, minimally invasive spine surgery is a standard part of orthopedic and neurological surgery. Procedures like endoscopic discectomy and kyphoplasty are common. They offer many treatment options for spinal problems.
The current state of practice is characterized by:
- Increased use of outpatient procedures
- Continued innovation in surgical techniques and technology
- Growing evidence supporting the efficacy of minimally invasive approaches
As technology keeps improving, we’ll see more advancements in spine surgery. This could lead to even better results for patients.
What Makes a Spine Surgery “Easy”?
Understanding what makes a spine surgery “easy” involves looking at both the surgical technique and the patient’s overall health. We consider a spine surgery “easy” when it involves minimally invasive techniques, fewer complications, and a quicker recovery time.
Surgical Criteria for Simplicity
Several factors contribute to the simplicity of a spine surgery. These include:
- Minimally invasive techniques that reduce tissue damage
- Shorter operation times
- Less blood loss during surgery
- Fewer complications
| Surgical Technique | Operation Time | Blood Loss | Complication Rate |
| Minimally Invasive Discectomy | 30-60 minutes | Minimal | Low |
| Endoscopic Discectomy | 45-90 minutes | Minimal | Low |
| Microdiscectomy | 60-120 minutes | Moderate | Moderate |
Patient Factors
Patient factors play a significant role in determining the ease of spine surgery. These include the patient’s overall health, age, and the specific condition being treated. Patients with fewer health issues and less complex spinal conditions tend to have simpler surgeries.
Recovery Considerations
Recovery considerations are also key in evaluating the ease of spine surgery. Surgeries with shorter recovery times and fewer post-operative complications are considered “easier.” Factors influencing recovery include the type of surgery, the patient’s health, and post-operative care.
By considering these factors, we can better understand what makes a spine surgery “easy” and make informed decisions about the best course of treatment.
Endoscopic Discectomy: The Least Invasive Option
Endoscopic discectomy is a big step forward in treating herniated discs. It’s a less invasive way than old-school surgeries. This method uses a small endoscope to see the disc and the area around it. It lets doctors remove the herniated part carefully.
Procedure Overview
The procedure starts with a small cut. Then, an endoscope and tools are put in. The endoscope shows the herniated disc clearly. This lets the surgeon take out the bad disc part without hurting the other tissues too much.
TESSYS Method and Variations
The TESSYS (Transforaminal Endoscopic Spine Surgery) method is a special way to do endoscopic discectomy. It goes through the spine’s foramen. Different angles and tools are used to fit each patient’s needs.
TESSYS has many benefits:
- It’s very minimally invasive, causing less damage
- It has fewer risks than open surgery
- Patients recover faster
- They feel less pain after surgery
Ideal Candidates
People with certain symptoms are best for endoscopic discectomy. They should have:
- Herniated discs that don’t get better with other treatments
- Discs that haven’t burst out
- Some types of spinal stenosis
Seeing a spine specialist is key to know if this treatment is right.
Recovery Timeline
Recovery from endoscopic discectomy is quicker than old surgeries. Most people can:
| Timeframe | Expected Recovery |
| Immediate Post-Surgery | Little pain, can start with light activities |
| 1-2 Weeks | Can do more, might go back to work |
| 4-6 Weeks | Full recovery, can do normal things again |
Everyone recovers differently. It depends on health, how big the surgery was, and following doctor’s orders.
“Endoscopic discectomy has changed how we treat herniated discs. It gives patients a quick, less invasive fix.” – Spine Surgery Expert
Microdiscectomy: Gold Standard for Herniated Discs
Microdiscectomy is seen as the top choice for treating herniated discs. It has high success rates and is less invasive. We’ll dive into the details of this procedure, including its method, success rates, and recovery.
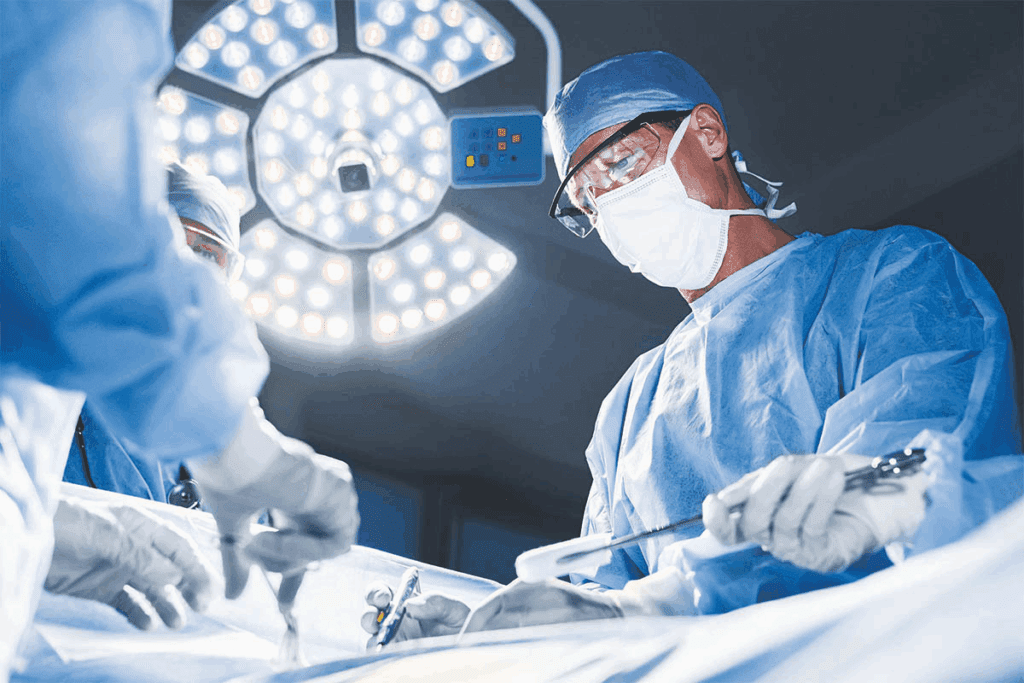
Surgical Technique
The surgery uses a small cut and an operating microscope to see the disc herniation. This minimally invasive method lets doctors remove the herniated disc material. This relieves pressure on the nerve.
Success Rates
Research shows microdiscectomy works well for herniated discs. Many patients feel better after the surgery. The procedure’s precision and direct aim at the herniated disc make it effective.
Typical Recovery Experience
Recovery from microdiscectomy is usually faster than traditional discectomy. Most people can get back to their usual activities in a few weeks. They benefit from less tissue damage and less pain after surgery.
Advantages Over Traditional Discectomy
Microdiscectomy has several benefits over traditional discectomy. It has smaller cuts, less muscle damage, and fewer complications. These advantages lead to better results for patients.
Minimally Invasive Treatments for Lumbar Spinal Stenosis
Minimally invasive treatments have changed how we treat lumbar spinal stenosis. This condition narrows the spinal canal, causing pain and discomfort. We’ll look at these treatments, like decompression and interspinous spacers, and how well they work.
Decompression Techniques
Decompression techniques are key in treating lumbar spinal stenosis. They aim to ease pressure on the spinal cord and nerves. Endoscopic decompression uses a small endoscope to see and remove the pressure-causing tissue.
Microdecompression involves a small incision and a microscope to find and remove the tissue. These methods have shown good results in easing symptoms and improving life quality.
Interspinous Spacers
Interspinous spacers are devices placed between the spinous processes to keep space and reduce nerve pressure. X-STOP is one such device used to treat lumbar spinal stenosis. It’s great for patients with neurogenic claudication.
Putting in interspinous spacers is a simple procedure that can be done under local anesthesia. This makes it a good choice for those who can’t handle more invasive surgeries.
Outcomes and Efficacy
Research shows that decompression techniques and interspinous spacers can effectively manage lumbar spinal stenosis. The right treatment depends on the condition’s severity and the patient’s health.
| Treatment | Success Rate | Recovery Time |
| Endoscopic Decompression | 80-90% | 2-4 weeks |
| Microdecompression | 85-95% | 4-6 weeks |
| Interspinous Spacers | 70-80% | 1-3 weeks |
It’s important for patients to talk to their healthcare provider to find the best treatment. Knowing the options and their outcomes helps patients make informed decisions about their care.
Kyphoplasty and Vertebroplasty for Compression Fractures
Kyphoplasty and vertebroplasty are two minimally invasive treatments for compression fractures. They help stabilize the fracture and reduce pain. These methods are popular because they improve a patient’s quality of life.
Procedure Comparison
Both kyphoplasty and vertebroplasty involve injecting bone cement into a fractured vertebra. But, they differ in their approach. Vertebroplasty is a simple cement injection. Kyphoplasty uses a balloon to create space before adding cement.
Key differences:
- Kyphoplasty can restore some lost height in the vertebra, unlike vertebroplasty.
- The balloon in kyphoplasty can reduce the fracture and improve spinal alignment.
- Kyphoplasty might offer better pain relief by stabilizing the fracture.
| Procedure | Description | Benefits |
| Vertebroplasty | Injection of bone cement into the fractured vertebra | Rapid pain relief, minimally invasive |
| Kyphoplasty | Inflation of a balloon within the vertebra followed by cement injection | Potential restoration of vertebral height, improved spinal alignment |
Patient Selection
Choosing the right procedure involves looking at several factors. These include the fracture’s severity, the patient’s health, and past treatments. The best candidates have painful fractures that haven’t improved with other treatments.
The choice between kyphoplasty and vertebroplasty depends on the specific characteristics of the fracture and the patient’s condition.
Recovery Expectations
Recovery from both procedures is usually quick. Most patients see pain relief within days. It’s important to follow post-procedure instructions to heal properly and avoid complications.
We recommend that patients:
- Avoid heavy lifting and bending.
- Do gentle exercises as advised by their healthcare provider.
- Follow a proper pain management regimen.
Understanding the differences between kyphoplasty and vertebroplasty helps patients make informed choices for treating compression fractures.
Minimally Invasive Spine Surgery Techniques and Approaches
Minimally invasive spine surgery has changed how we treat spinal problems. It uses methods that cause less damage and help patients heal faster. We choose the best treatment for each patient’s needs.
Tubular Retractor Systems
Tubular retractor systems are key in minimally invasive spine surgery. They let surgeons work through small cuts. These systems use dilators to slowly open the area, protecting muscles.
With tubular retractors, surgeons can see the area clearly. This makes it easier to do surgeries like discectomies and decompressions.
Endoscopic Approaches
Endoscopic spine surgery uses a thin, flexible tube with a camera and light. It lets doctors see the spine without big cuts. This way, patients heal faster and with less damage.
- Endoscopic discectomy for herniated discs
- Endoscopic decompression for spinal stenosis
Laser and Radiofrequency Procedures
Laser and radiofrequency methods are used in spine surgery. They help remove damaged tissue or stop pain. These methods are less invasive and may have fewer side effects.
Small Incision Benefits
Small cuts in spine surgery mean less damage and less pain after. Patients also heal faster. These benefits lead to better results and happier patients.
Outpatient Spine Procedures: Same-Day Surgery Options
Medical technology has improved a lot. Now, patients can go home the same day after spine surgery. This change is thanks to new, less invasive methods. These methods cause less damage and help patients heal faster.
Qualifying Procedures
Not every spine surgery can be done on an outpatient basis. But, many common problems can be treated this way. These include:
- Herniated discs treated with microdiscectomy or endoscopic discectomy
- Lumbar spinal stenosis addressed through minimally invasive decompression
- Certain compression fractures managed with kyphoplasty or vertebroplasty
These surgeries are simpler and have quicker recovery times. That’s why they’re great for outpatient care.
Patient Selection Criteria
Choosing the right patients is key for outpatient spine surgery success. The best candidates are those who:
- Have a stable medical condition
- Are in overall good health
- Have a supportive home environment for post-operative care
- Are able to follow post-operative instructions
We look at each patient’s health, age, and any other health issues. This helps us decide if they’re right for outpatient surgery.
Home Recovery Support
Having the right support at home is vital for patients after outpatient spine surgery. This means:
- Having a responsible adult to accompany the patient home and stay with them for at least the first 24 hours
- Ensuring the home is safe and free from tripping hazards
- Having necessary medications and supplies readily available
- Following a structured post-operative care plan
We give detailed advice on recovering at home. This helps avoid problems and makes the transition back home smoother.
Alternatives to Spinal Fusion
New advancements in spinal surgery offer several options instead of traditional spinal fusion. Thanks to medical technology, patients can now choose from various treatments. This means they don’t have to go through the more invasive spinal fusion procedure.
Motion Preservation Techniques
Motion preservation techniques help keep the spine moving naturally. This is different from spinal fusion, which stops the spine from moving. These methods are great for people with problems in the spinal discs or facet joints.
Benefits of Motion Preservation include less stress on other parts of the spine and faster recovery. But, these options might not work for everyone. Their long-term effects are also being studied.
Artificial Disc Replacement
Artificial disc replacement is a surgery that replaces a bad or damaged disc with an artificial one. It’s mainly used for degenerative disc disease.
The advantages of artificial disc replacement include keeping the spine mobile and possibly reducing pain. It’s important for patients to talk to their doctors about the risks and benefits. This helps decide if it’s the right choice for them.
Posterior Dynamic Stabilization
Posterior dynamic stabilization uses flexible implants to support the spine while keeping some natural movement. It’s good for patients with spinal instability or degenerative conditions.
The aim of posterior dynamic stabilization is to support the spine without the stiffness of fusion. This could lead to better results for some patients in the long run.
Exploring these alternatives to spinal fusion helps patients and doctors find the best treatment. It’s all about finding what works best for each person’s needs and condition.
Advanced Technologies in Minimally Invasive Spine Surgery
The field of minimally invasive spine surgery is changing fast. New technologies are making these surgeries more precise, safe, and effective.
Robotic-Assisted Surgery
Robotic-assisted spine surgery is a big step up in surgery tech. It lets surgeons work with more accuracy and control. Robotic-assisted surgery also offers real-time images and feedback, helping surgeons make better decisions.
The benefits of robotic-assisted spine surgery include:
- Enhanced precision and accuracy
- Reduced risk of complications
- Smaller incisions, leading to less tissue damage and scarring
- Faster recovery times for patients
Navigation Systems
Navigation systems are key in today’s spine surgery. They guide surgeons in real-time, using advanced imaging to track instruments. This helps surgeons navigate the complex spinal anatomy better.
The key advantages of navigation systems include:
- Improved accuracy in implant placement
- Reduced radiation exposure for both patients and surgical staff
- Enhanced visualization of spinal structures
Augmented Reality Applications
Augmented reality (AR) is starting to impact spine surgery. AR overlays digital info on the real world, giving surgeons vital data during surgery. This tech could make spine surgery even more precise and safe.
Some of the benefits of AR in spine surgery include:
- Real-time feedback on anatomical structures
- Enhanced visualization of complex spinal anatomy
- Improved accuracy in surgical instrument placement
Future Innovations
As tech keeps advancing, we’ll see even more new things in spine surgery. Future advancements might include more artificial intelligence, better robotic systems, and more AR and virtual reality use.
These new technologies promise to improve patient care and offer more treatment options for spinal issues.
Choosing the Right Surgeon and Facility
Choosing the right surgeon and facility is key to a successful spine surgery. It’s important to consider several factors to get the best care. This ensures a good outcome for your surgery.
Surgeon Experience and Specialization
Your surgeon’s experience and specialization matter a lot. A skilled surgeon in minimally invasive spine surgery can handle complex cases well. They can also help you recover faster. Look for a surgeon who is board-certified and has a good track record in your needed procedure.
Check the surgeon’s credentials, like their education and certifications. Also, read patient testimonials to learn about their expertise and care.
Hospital vs. Ambulatory Surgery Center
Deciding between a hospital or an ambulatory surgery center (ASC) is important. Hospitals can handle complex cases and have more resources. But, ASCs offer a more personal experience, might be cheaper, and have lower infection risks.
| Criteria | Hospital | Ambulatory Surgery Center |
| Complexity of Cases | Can handle complex and emergency cases | Generally handles less complex, elective procedures |
| Cost | Typically more expensive | Often less expensive |
| Personalization | May have less personalized care due to higher volume | Offers more personalized care |
| Infection Risk | Higher risk of hospital-acquired infections | Lower risk of infections |
Questions to Ask Before Surgery
Before spine surgery, ask your surgeon and facility staff important questions. This helps you make an informed choice. Key questions include:
- What experience do you have with this specific procedure?
- What are the possible risks and complications, and how are they managed?
- What is the recovery process like, and what support will I get?
- Are there other treatments or procedures I should consider?
By asking the right questions, you can choose wisely. This ensures the best outcome for your spine surgery.
Post-Operative Care and Rehabilitation
Good post-operative care and rehabilitation are key for a full recovery after spine surgery. They help patients get back to their normal lives quickly. Spine surgery has changed a lot, and so has how we care for patients after surgery.
Immediate Recovery Period
The first few days after surgery are very important. Patients usually stay in the hospital to be closely watched. Medical staff manage pain and look for any problems.
Key aspects of immediate recovery include:
- Pain management through medication
- Monitoring for signs of infection or other complications
- Gradual mobilization to prevent blood clots and stiffness
Physical Therapy Protocols
Physical therapy is a big part of getting better. It helps patients get stronger and move better. The therapy plan depends on the surgery type.
A typical physical therapy regimen may include:
- Gentle exercises to improve flexibility and strength
- Posture correction and body mechanics training
- Progressive resistance exercises to enhance muscle strength
Rehabilitation after spine surgery is not just about recovering from the operation; it’s about returning to a fully functional life.
Long-Term Maintenance
Keeping the spine healthy long-term is important. This means making lifestyle changes, exercising regularly, and seeing doctors for check-ups.
Long-term maintenance strategies include:
- Regular exercise routines to maintain flexibility and strength
- Maintaining a healthy weight to reduce spinal stress
- Ergonomic adjustments at work and home
Return to Work and Activities
When to go back to work or normal activities varies. It depends on the surgery, the patient’s health, and their job. Patients should avoid heavy lifting and bending for a few weeks.
Factors influencing return to work include:
| Factor | Description | Impact on Recovery |
| Type of Surgery | Minimally invasive vs. traditional open surgery | Minimally invasive typically allows for quicker return to work |
| Job Requirements | Desk job vs. manual labor | Desk jobs usually allow for earlier return compared to physically demanding jobs |
| Patient’s Health | Overall physical condition and presence of comorbidities | Better overall health generally correlates with faster recovery |
Following a detailed care and rehabilitation plan helps patients get the best results after spine surgery. It’s a team effort between the patient, doctors, and sometimes physical therapists. This ensures a smooth and effective recovery.
Conclusion: The Future of Spine Surgery
The field of spine surgery is changing fast, thanks to new minimally invasive techniques. These advancements are making treatments better and less invasive for patients.
Looking ahead, spine surgery will keep getting better. New technologies like robotic surgery and endoscopic methods are on the horizon. They promise to make treatments more effective and reduce recovery times.
As more people seek minimally invasive spine surgery, we’ll see even more breakthroughs. These will help meet the complex needs of patients with spinal issues. They will offer safer and more effective treatments.
In the end, the goal of spine surgery’s future is to improve patient care. By embracing these new advancements, we’re set for a brighter future for those undergoing spine surgery.
FAQ
What is minimally invasive spine surgery?
Minimally invasive spine surgery is a new way to treat spinal problems. It uses small cuts to fix issues, causing less pain and quicker healing. This method also lowers the chance of serious side effects.
What are the benefits of endoscopic discectomy?
Endoscopic discectomy is a less invasive surgery. It causes less damage to tissues, less pain after surgery, and faster recovery. This is compared to older surgery methods.
What is the TESSYS method in endoscopic discectomy?
The TESSYS method is a special way to do endoscopic discectomy. It uses a unique system to remove disc material. This method has a high success rate and few complications.
What is microdiscectomy, and how does it compare to traditional discectomy?
Microdiscectomy is a new, small surgery for herniated discs. It has smaller cuts, less damage, and quicker healing than traditional discectomy.
What are the treatment options for lumbar spinal stenosis?
For lumbar spinal stenosis, treatments include small surgeries and special devices. These aim to ease nerve pressure and improve symptoms.
What is the difference between kyphoplasty and vertebroplasty?
Kyphoplasty and vertebroplasty are both for compression fractures. Kyphoplasty uses a balloon to lift the vertebra. Vertebroplasty injects bone cement into the vertebra.
What are the benefits of outpatient spine procedures?
Outpatient spine surgeries have many benefits. They include shorter hospital stays, less risk of infections, and faster recovery. They are good for patients who qualify.
What are the alternatives to spinal fusion?
Instead of spinal fusion, there are other options. These include keeping the spine moving with special devices. They aim to avoid future problems.
How do advanced technologies improve minimally invasive spine surgery?
New technologies like robots and navigation systems make spine surgery better. They improve accuracy, safety, and results. This leads to better care for patients.
What factors should I consider when choosing a surgeon and facility for spine surgery?
When picking a surgeon and place for spine surgery, think about a few things. Look at the surgeon’s experience and the facility’s reputation. Also, check if they have the latest technology and good care after surgery.
What is the importance of post-operative care and rehabilitation after spine surgery?
Care and rehab after spine surgery are very important. They help ensure a smooth recovery and avoid problems. They also help improve long-term results.
What is the recovery timeline for endoscopic discectomy?
Recovery from endoscopic discectomy is usually short. It includes a brief hospital stay and then rest and rehab. Most people can get back to normal in a few weeks.
What are the advantages of robotic-assisted spine surgery?
Robotic-assisted spine surgery has many benefits. It offers better accuracy, less radiation, and better results. It’s a valuable tool for treating many spinal issues.
Can I undergo spine surgery as an outpatient procedure?
Yes, some spine surgeries can be done without staying in the hospital. It depends on the surgery type, patient health, and support at home.
References
- Wang, T. Y., et al. (2024). Advances and challenges in minimally invasive spine surgery. Journal of Spine Surgery, 10(2), 105-117. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11173127/