Last Updated on November 27, 2025 by Bilal Hasdemir

Radiology billing in the US can be tricky, mainly when CT scans are done here but read elsewhere. This situation, often referred to as “ct scans only done but no reader in the US,” makes getting paid and following CMS guidelines harder.
Radiology billing is tough because of new codes, detailed paperwork, and strict rules. The 2025 CMS 2.83% cut in Medicare conversion factor will also affect radiology services.
It’s key to know the technical and professional sides of radiology billing. Also, understanding medical necessity and following CMS guidelines helps avoid expensive mistakes.
Key Takeaways
- Understand the technical and professional components of radiology billing.
- Ensure compliance with CMS guidelines to avoid billing errors.
- Stay updated on changes in radiology coding guidelines.
- Verify medical necessity for radiology services.
- Be aware of the impact of CMS updates on radiology billing.
The Current Landscape of Radiology Billing in the US

The state of radiology billing in the US is changing due to new trends and CMS updates. This field is complex and influenced by CMS rules. These rules guide how radiology billing works.
Recent Trends Affecting Radiology Practices
There’s a big push for medical billing compliance and using new tech to make billing easier. Billing is now more focused on the patient, making things clearer and happier for them.
New billing software and AI are being used more. They help cut down on mistakes and make billing faster. But these changes also mean more training and possibly higher costs for new tech.
Impact of the 2025 CMS 2.83% Reduction in Medicare Conversion Factor
The CMS’s 2.83% reduction in Medicare conversion factor for 2025 is a big deal. It lowers how much money radiology services get paid, affecting doctors’ and imaging centers’ income.
This change makes billing harder, like keeping up with reimbursement rates and staying financially stable. Radiology practices need to find ways to deal with this, like improving how they code and bill.
Key Challenges Facing Radiology Billing Professionals
Radiology billing pros face big hurdles, like following complex CMS rules and dealing with radiology billing challenges. One big issue is knowing how to bundle and unbundle procedures correctly, as CMS has strict rules.
Many radiology places lose money because of wrong billing, like unbundling when they should bundle. It’s key to keep up with CMS rules and have accurate records to beat these challenges.
Understanding Technical vs. Professional Components in Radiology Billing

Getting radiology billing right means knowing the difference between the technical and professional parts of radiology services. This is key to making sure both the place where the test is done and the doctor who reads it get paid right.
Defining Technical Component (TC) in Radiology Services
The Technical Component (TC) covers the technical side of radiology services. This includes the equipment, supplies, and the people needed to do the test. It’s usually billed by the place where the test is done.
In radiology billing, the TC is very important. It includes the costs of doing the test, like the scanner, the tech’s work, and the place’s overhead. For example, a CT scan’s TC covers the scanner, the tech, and the facility’s costs.
Explaining the Professional Component (PC) in Radiology Services
The Professional Component (PC) is about the doctor’s job of reading the images. It’s billed separately from the TC and is done by the doctor or their group.
The PC is key in radiology billing. It pays the doctor for reading the images and writing a report. This part needs a lot of skill and is a big part of the test’s value.
Proper Use of Modifiers ‘-TC’ and ‘-26’
Modifiers ‘-TC’ and ‘-26’ are important in radiology billing. The ‘-TC’ shows it’s for the technical part, and the ‘-26’ shows it’s for the professional part.
Using these modifiers correctly is very important. If a hospital bills for a CT scan with the ‘-TC’ modifier, it means it’s for the technical part. If a doctor bills for reading the CT scan with the ‘-26’ modifier, it means it’s for their professional work.
Not using these modifiers correctly can cause problems. It can lead to denied claims, delayed payments, and more work for everyone. So, it’s very important for radiology billing experts to use these modifiers correctly.
CT Scans Only Done, But No Reader in the US: Billing Implications
CT scans done in the US but read abroad can be tricky for billing. This method might save money, but it makes billing harder. It’s because the technical and professional parts are split.
Legal and Compliance Considerations for Offshore Interpretations
Using offshore readers for CT scans brings up legal and compliance issues. Healthcare providers must check if offshore teams follow US healthcare laws, including HIPAA. They need to make sure these teams keep patient info and data safe, like US teams do.
The Centers for Medicare and Medicaid Services (CMS) rules must be followed for billing. Payers won’t pay for scans unless they’re needed. It’s up to the coder to prove this need in the claim.
Billing Protocol for Domestically Performed but Internationally Interpreted Scans
When scans are done in the US but read abroad, the US place should only bill for the technical part. The reader should bill for the professional part. This split billing needs clear records to meet payer rules.
- The technical part includes the cost of the equipment, upkeep, and the tech team.
- The professional part is the radiologist’s job to read the scan.
Documentation Requirements for Split Technical and Professional Services
Good records are key for split billing. The technical part needs details on the scan, like the equipment and who did it. The radiologist must also write a detailed report of their scan findings.
Right coding and records are vital to avoid claim rejections and follow CMS rules. This means using the right codes (‘-TC’ for technical and ‘-26’ for professional) and having all the needed documents.
Essential CMS Radiology Billing Guidelines for 2025
The CMS has made important updates to radiology billing for 2025. These changes include updates to the Medicare Physician Fee Schedule and bundled payment policies. Radiology practices need to understand these updates to stay compliant and get the most from their billing.
Updated Medicare Physician Fee Schedule for Radiology
The Medicare Physician Fee Schedule has been updated for 2025. There’s a 2.83% reduction in the Medicare conversion factor. This change affects how radiology services are paid, so practices need to adjust their billing strategies.
Key aspects of the updated fee schedule include:
- Revised payment rates for radiology services
- Updates to relative value units (RVUs) for certain procedures
- Continued emphasis on value-based care initiatives
Changes to Bundled Payment Policies
Bundled payment policies are changing, affecting how radiology services are billed and reimbursed. The CMS has made these policies more refined to manage costs and improve care coordination.
Important changes include:
- Expanded bundled payment models for certain diagnostic imaging procedures
- Enhanced guidance on billing for bundled services
- Increased focus on cost containment and quality metrics
Compliance Requirements for Radiology Practices
Radiology practices must follow strict compliance rules to avoid penalties and ensure proper payment. Key areas include:
- Accurate coding and documentation practices
- Adherence to the National Correct Coding Initiative (NCCI) edits
- Compliance with CMS guidelines for radiology billing
To show why compliance is key, consider this example:
| Compliance Area | Potential Risk | Mitigation Strategy |
| Accurate Coding | Incorrect coding leading to claim denials | Regular staff training on coding updates |
| Documentation | Insufficient documentation supporting medical necessity | Implementation of robust documentation protocols |
By keeping up with these changes and adapting to the evolving radiology billing landscape, practices can stay compliant and improve their revenue cycle.
Navigating Radiopharmaceutical Billing Changes
The CMS has made a big change in radiopharmaceutical billing. Now, certain high-cost radiopharmaceuticals get separate reimbursement. This change shows how payment policies in radiology are always evolving. It’s key for radiology practices to understand these changes to stay compliant and get the most reimbursement.
New Separate Reimbursement Rules for Radiopharmaceuticals Over $630
The CMS now pays separately for radiopharmaceuticals costing over $630 per day. This change impacts how radiology practices bill for these expensive agents. To benefit from this rule, practices need to use the right coding and documentation for these radiopharmaceuticals.
Key aspects of the new reimbursement rule include:
- Separate reimbursement for radiopharmaceuticals costing over $630 per day
- Updated coding requirements for high-cost radiopharmaceuticals
- Potential impact on bundled payment arrangements
Documentation Requirements for Radiopharmaceutical Claims
Good documentation is key for radiopharmaceutical claims, now more than ever. Radiology practices must keep detailed records of radiopharmaceutical use. This includes the specific agent, dosage, and date of administration.
Best practices for documentation include:
- Maintaining detailed records of radiopharmaceutical administration
- Ensuring accurate coding and billing information
- Retaining documentation to support medical necessity
Common Billing Errors and How to Avoid Them
Radiology practices need to watch out for common billing errors with radiopharmaceuticals. These errors can lead to claim denials and compliance issues. The most common mistakes include wrong coding, not enough documentation, and not showing medical necessity.
Strategies to avoid these errors include:
- Implementing robust coding and billing protocols
- Conducting regular audits to ensure compliance
- Providing ongoing training for staff on radiopharmaceutical billing
By knowing the new reimbursement rules, keeping good documentation, and avoiding common errors, radiology practices can handle the changes in radiopharmaceutical billing well.
Establishing Medical Necessity for Radiology Procedures
Radiology practices must focus on showing medical necessity to follow CMS rules and get paid. It’s key for radiology billing to prove a procedure is needed. This affects whether it gets paid back.
CMS Requirements for Demonstrating Medical Necessity
The Centers for Medicare and Medicaid Services (CMS) says radiology procedures need a valid reason in the patient’s file. “The chosen diagnosis must logically support the reason for the imaging service,” CMS says. Good radiology coding links the procedure to the patient’s need.
To meet CMS rules, radiology practices need strong documentation. They should keep detailed patient records that show why the procedure was needed.
Proper Documentation Practices
Good documentation is key for showing medical necessity. Radiology practices should follow these steps:
- Keep detailed patient records that show why the procedure was needed.
- Make sure the doctor’s notes support the need for the procedure.
- Use the right ICD-10 codes that match the patient’s condition and the procedure.
By following these steps, radiology practices can make their claims stronger. This helps avoid denials because of medical necessity.
Handling Denied Claims Due to Medical Necessity Issues
Even with careful planning, claims might get denied for medical necessity. If this happens, radiology practices should have a plan. This includes:
- Looking at why the claim was denied and if it’s fair.
- Getting more information, if needed, to prove the procedure was necessary.
- Writing a detailed appeal that answers the denial and shows evidence.
As “The key to successful appeals lies in providing clear, concise, and compelling evidence that supports the medical necessity of the procedure.” Being proactive with denied claims can help radiology practices get more money. It also makes their work easier.
Critical CPT Codes for Radiology Billing Success
Knowing CPT codes well is key for radiology billing pros. It helps them deal with the complex world of medical billing. Getting CPT coding right is important for following rules and getting the most money for radiology services.
Understanding Q0092 and 99071 CPT Codes
The CPT codes Q0092 and 99071 are big in radiology billing. Q0092 is for setting up and moving a portable X-ray machine. 99071 is for educational stuff for patients. Knowing how to use these codes right is very important.
Q0092: Setup and Portability of Portable X-ray Equipment – This code is for when a portable X-ray machine is taken to a patient. It’s important to bill correctly to avoid mistakes.
99071: Educational Supplies – This code is for teaching materials given to patients. In radiology, this could be about procedures or how to care for yourself after a procedure.
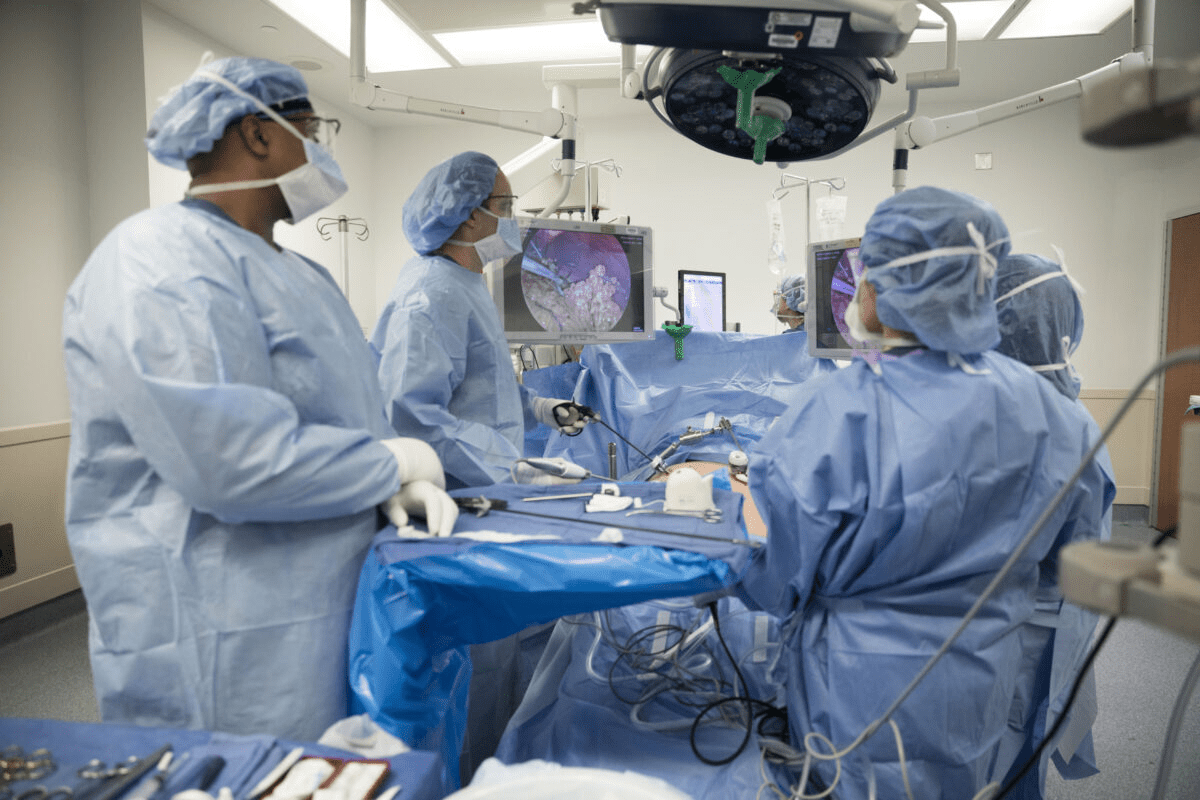
Interventional Radiology Coding Essentials
Interventional radiology needs precise coding because it’s about small, detailed procedures. The CPT codes used here are complex and varied.
| CPT Code | Description |
| 37241 | Vascular embolization or occlusion |
| 36245 | Selective catheter placement in the visceral artery |
| 77012 | Computed tomography guidance for needle placement |
It’s very important to know these codes and how to use them for accurate billing in interventional radiology.
When to Use 76499 (Unlisted Radiologic Procedure)
The CPT code 76499 is for procedures that don’t have a specific code. This code is used when a procedure doesn’t fit into any other category.
Documentation is key when using 76499. You need to keep detailed records of the procedure, like the method used and why it was needed, for successful billing.
Using the right CPT codes, including knowing when to use 76499, is very important for the financial health of radiology practices.
Diagnostic Imaging Center Billing Best Practices
Diagnostic imaging centers need to make their billing better to stay accurate and efficient. This is important in today’s complex healthcare world. Good billing helps keep finances stable and follows rules.
Optimizing Workflow Between Technical and Professional Services
It’s key for imaging centers to work well between technical and professional services. The technical part deals with the equipment and getting patients ready. The professional part is when radiologists read the images.
Key strategies for optimization include:
- Using integrated practice management systems (PMS) for both technical and professional billing.
- Having clear communication and data sharing between technical staff and radiologists.
- Using computer-assisted coding (CAC) systems to make coding better and faster.
Implementing Effective Charge Capture Systems
Good charge capture systems are vital for billing all services correctly. This means:
- Using electronic health records (EHRs) and practice management systems (PMS) with charge capture.
- Training staff on the need for accurate and quick charge capture.
- Checking charge capture often to find and fix mistakes.
Strategies for Reducing Claim Denials
Lowering claim denials is key for keeping cash flow and reducing work. Strategies include:
- Using claim scrubbers to find and fix errors before sending claims.
- Ensuring patient and insurance info is correct.
- Keeping up with CMS guidelines and other payer rules to avoid wrong claims.
By following these best practices, imaging centers can make billing better, cut down on denials, and follow rules.
Compliance Strategies for Radiology Practices Under CMS Chapter 13
Radiology practices face strict rules under CMS Chapter 13 to avoid audits and penalties. Following these rules is key to keeping finances stable and reputation high in healthcare.
Key Provisions Affecting Radiology
CMS Chapter 13 has several rules that affect radiology practices. Knowing these rules is vital for good compliance strategies. Important areas include:
- Coverage and Payment Rules: It’s important to know when Medicare covers radiology services. This helps in billing correctly.
- Documentation Requirements: Keeping detailed records is essential. Radiology practices must document all necessary information well.
- Compliance with Coding Guidelines: Correct coding is key for billing and following rules. Staying current with CPT and ICD codes is necessary.
Audit Preparation and Documentation Requirements
Getting ready for audits is important. Radiology practices need to keep accurate records and have strong documentation. Key steps include:
- Maintaining Detailed Patient Records: Patient records must be complete and show the services given accurately.
- Implementing a Compliance Audit Program: Regular audits help find and fix compliance issues early.
- Training Staff: All staff should know about compliance rules and their roles in following them.
Implementing a Robust Compliance Program
A strong compliance program is vital for radiology practices under CMS Chapter 13. Key parts of such a program are:
- Designating a Compliance Officer: Having a dedicated compliance officer is important. They oversee compliance and ensure the practice follows CMS rules.
- Regular Updates and Training: Keeping up with CMS Chapter 13 changes and training staff regularly is necessary.
- Continuous Monitoring and Improvement: It’s important to regularly check and improve compliance processes. This keeps them effective and in line with rules.
By understanding and using these compliance strategies, radiology practices can lower their risk of non-compliance. This helps them stay stable and respected in healthcare.
Conclusion: Future-Proofing Your Radiology Billing Practices
Radiology billing needs to keep up with new CMS rules and coding changes. To stay ahead, it’s important to be proactive in medical billing for radiology. This means making sure staff know how to handle complex coding rules.
Putting money into good billing practices and training staff pays off. It leads to better cash flow, fewer claim denials, and less risk of audits. Keeping current with radiology billing helps avoid financial losses and boosts earnings.
It’s key for radiology practices to have strong compliance strategies. This helps them deal with the constant changes in medical billing. By focusing on future-proofing and following rules, radiology practices can stay financially stable and thrive in the long run.
FAQ
What are the key challenges facing radiology billing professionals?
Radiology billing pros struggle with CMS rules, accurate coding, and following regulations. The 2025 CMS 2.83% Medicare cut is a big challenge.
How do technical and professional components impact radiology billing?
Technical and professional parts are key in radiology billing. The technical part is about the equipment used. The professional part is about the doctor’s work. Using modifiers ‘-TC’ and ‘-26’ correctly is important.
What are the billing implications of CT scans performed domestically but interpreted abroad?
CT scans done in the U.S. but read abroad need careful billing. Legal and compliance issues, billing rules, and documentation are important. Knowing the rules for offshore readings is key.
What are the essential CMS radiology billing guidelines for 2025?
For 2025, CMS has new rules for radiology billing. This includes the Medicare Fee Schedule update and new payment policies. Knowing these rules is essential for success.
How have radiopharmaceutical billing rules changed?
New rules for radiopharmaceuticals over $630 have come in. There are specific rules for billing. It’s important to know these changes to avoid mistakes.
What establishes medical necessity for radiology procedures?
Medical necessity for radiology is based on CMS rules and proper documentation. Understanding these rules helps handle denied claims.
What are the critical CPT codes for radiology billing success?
Important CPT codes for radiology billing are Q0092, 99071, and 76499. Knowing how to use these codes is vital for accurate billing.
What are the best practices for diagnostic imaging center billing?
Good billing practices include efficient workflow and effective charge capture. Reducing denials is also important.
How can radiology practices ensure compliance under CMS Chapter 13?
To comply with CMS Chapter 13, radiology practices need to understand the rules. They should prepare for audits and have a strong compliance program.
What is the significance of CPT code Q0092?
CPT code Q0092 is important in radiology billing. Knowing how to use it is key to accurate billing and following CMS rules.
How can radiology billing practices be future-proofed?
To stay ahead, radiology billing needs to follow CMS rules and invest in staff training. Proper billing practices are also essential for success.
Reference
Practice Expense and Its Impact on Radiology Reimbursement. (2025). Journal (ScienceDirect). https://www.sciencedirect.com/science/article/pii/S1546144025001528