Knowing about a thrombus is key for stopping and treating serious health problems. At LivHospital, we use top medical skills and fair rules to give the best care. Learn the thrombus definition in medical terms and understand how blood clots form inside vessels.
A thrombus is a blood clot in a blood vessel or heart. It blocks blood flow. This can cause big health problems if not fixed right away.
We make sure to give clear info to people looking for health care worldwide. Our goal is to offer top-notch care with full support and advice.
Key Takeaways
- Understanding the medical definition of a thrombus is vital for health prevention.
- A thrombus is a blood clot that forms within a blood vessel or heart chamber.
- Thrombosis can lead to serious health issues if not properly treated.
- LivHospital delivers superior healthcare outcomes through advanced expertise and ethical protocols.
- Clear and accessible information is key for international healthcare seekers.
The Medical Definition of Thrombus
The term “thrombus” refers to a blood clot inside a blood vessel. This is a serious issue because it can cause strokes and heart attacks. Knowing about thrombus and how it forms is key for doctors and patients.
Clinical Terminology Explained
A thrombus is made up of fibrin, platelets, white blood cells, and some red blood cells. It forms when the body’s clotting gets out of balance. This can be due to injury, abnormal blood flow, or a tendency for blood to clot too much.
Thrombosis is the process of forming a thrombus. It involves many steps and factors. The main parts of thrombosis are:
- Platelets: These small cells clump together to form a clot.
- Fibrin: A protein that traps blood cells and platelets, making the clot stable.
- White blood cells: These cells are part of the immune response and can be in the thrombus.
- Red blood cells: Some red blood cells can also be trapped in the clot.
Difference Between Thrombus and Other Blood Conditions
It’s important to know the difference between a thrombus and other blood conditions. For example, an embolus is a clot that breaks loose and travels through the blood. Unlike a thrombus, which stays in one place, an embolus can move and cause blockages in other parts of the body, leading to serious problems like pulmonary embolism or stroke.
Here are some main differences between a thrombus and other blood conditions:
- Location: A thrombus stays in the vessel where it formed, while an embolus moves.
- Composition: Both are clots, but their composition and context (stationary vs. traveling) are different.
- Clinical Implications: A thrombus can cause local effects like vessel occlusion, while an embolus can damage distant organs.
Knowing these differences is critical for accurate diagnosis and treatment. By understanding the characteristics of a thrombus and how it differs from other conditions, doctors can provide the right care for patients.
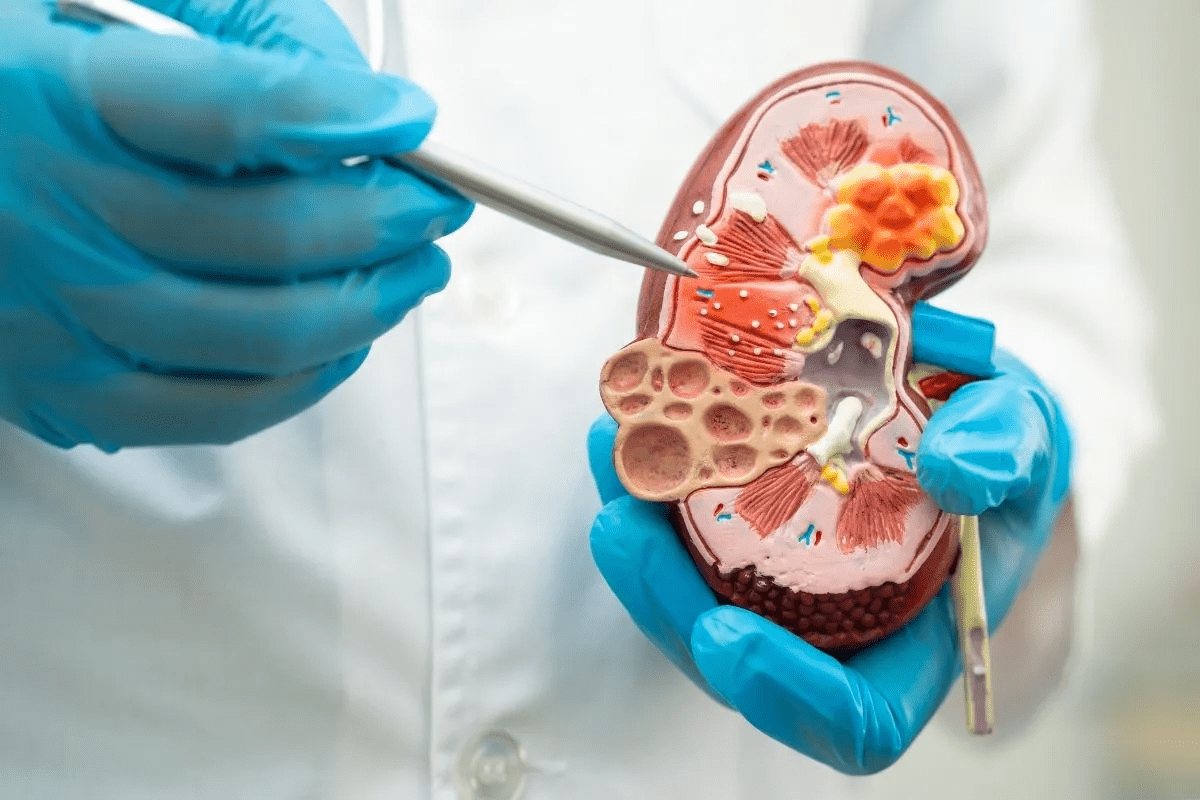
The Composition and Structure of a Thrombus
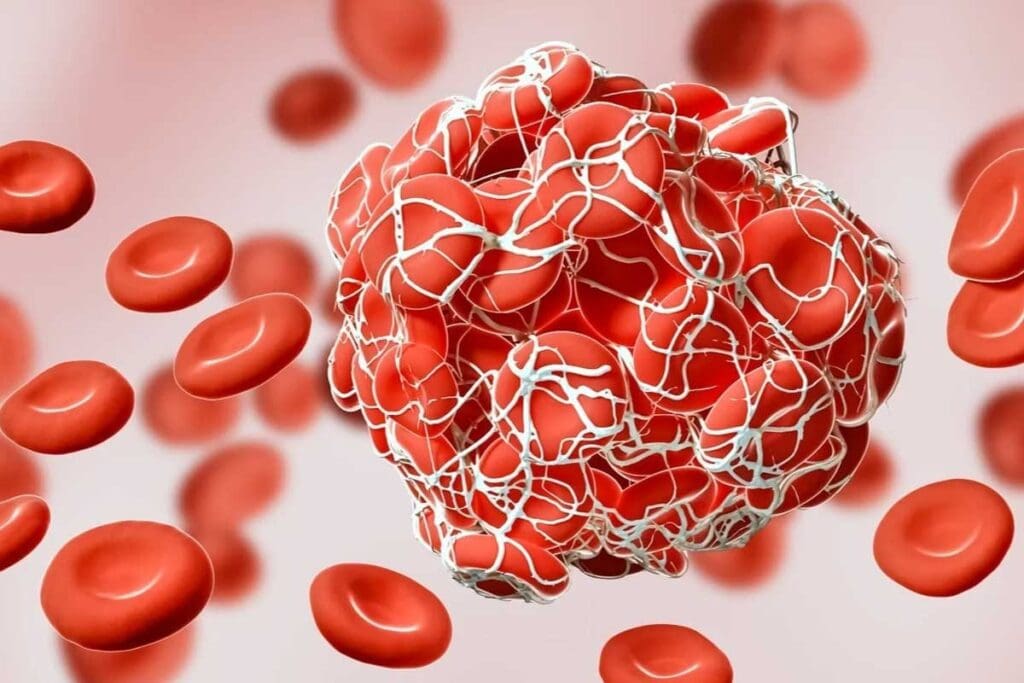
A thrombus is made up of platelets, fibrin, and blood cells. These elements are key to its structure and function. Knowing about them helps us understand how thrombi form and their impact on the body.
Key Components: Platelets, Fibrin, and Blood Cells
The main parts of a thrombus are:
- Platelets: These small blood cells start the formation of a thrombus. They gather at injuries, forming a platelet plug.
- Fibrin: Fibrin is a protein made during clotting. It creates a mesh that holds the platelet plug together, making the thrombus solid.
- Blood Cells: Red and white blood cells get trapped in the fibrin mesh. They add to the thrombus’s makeup.
How Thrombi Vary in Different Blood Vessels
The structure and makeup of a thrombus change based on where it forms in the blood vessels. For example:
- Arterial Thrombi: These are rich in platelets because of the high flow in arteries. They are often linked to sudden heart problems.
- Venous Thrombi: In veins, where blood flows slower, thrombi are more likely to have red blood cells and fibrin.
It’s important to understand these differences for better treatments of thrombus-related issues.
Thrombus Formation: The Process of Thrombosis
Thrombus formation is a complex process. It involves the coagulation cascade, a series of events that lead to thrombosis. Knowing this process is key to understanding many cardiovascular conditions.
The Coagulation Cascade Explained
The coagulation cascade is a series of biochemical reactions. These reactions result in the formation of a blood clot. It involves multiple clotting factors, which are proteins found in blood plasma.
We can break down the coagulation cascade into three main pathways. These are the intrinsic pathway, the extrinsic pathway, and the common pathway. These pathways come together to form a fibrin clot, which is the main component of a thrombus.
Thromboz: Understanding the Turkish Medical Term
In Turkish medical terminology, “thromboz” refers to thrombosis, the process of thrombus formation. Knowing this term is essential for international healthcare communication.
The term “thromboz” is used in various medical contexts in Turkey and other Turkish-speaking regions. It’s important for healthcare providers to know this terminology. This ensures accurate diagnoses and treatments.
| Term | Definition | Clinical Significance |
| Thrombosis | Formation of a blood clot within a blood vessel | Causes vascular obstruction, leading to ischemia or infarction |
| Thromboz | Turkish term for thrombosis | Essential for international medical communication |
| Coagulation Cascade | Series of biochemical reactions leading to clot formation | Critical for understanding thrombus formation |
Thrombus formation is a complex process that involves the coagulation cascade. Understanding this process and the terminology used in different medical contexts is vital. It’s key for effective healthcare delivery.
Types of Thrombi and Their Characteristics
It’s important to know about the different types of thrombi to treat them well. Thrombi can form in arteries, veins, and the heart. Each type has its own traits and effects on health.
Arterial Thrombi: Causes and Features
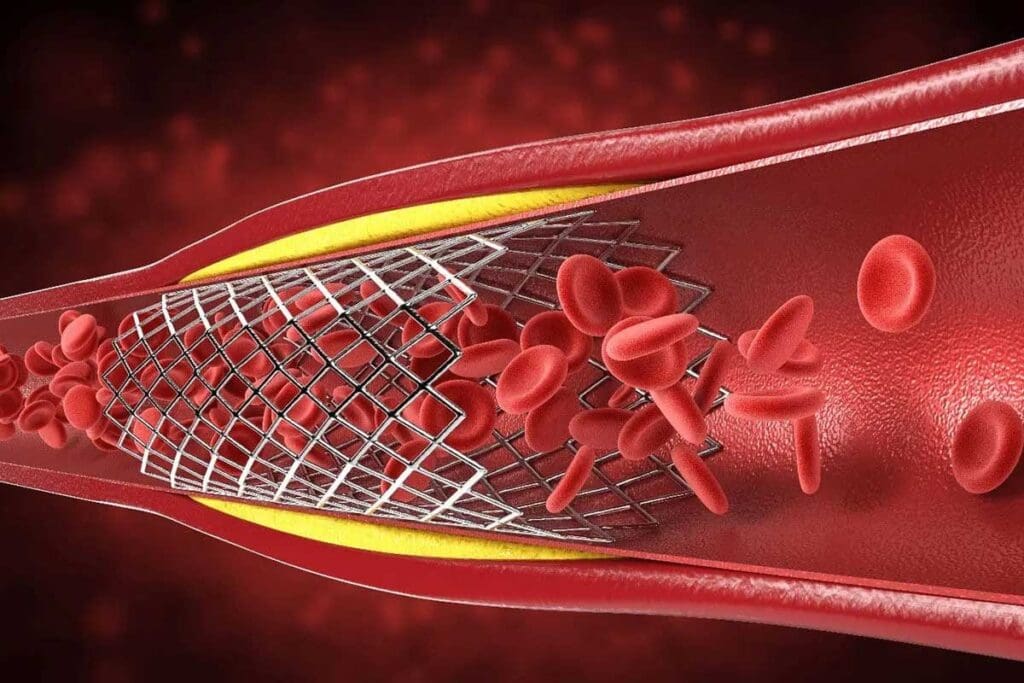
Arterial thrombi happen in arteries, which carry blood away from the heart. They often come from atherosclerosis, where plaque builds up. This can cause clots and lead to heart attacks and strokes.
“The formation of arterial thrombi is a complex process involving platelet activation, adhesion, and aggregation,” explains a leading cardiologist. “Understanding these mechanisms is key for prevention and treatment.”
Venous Thrombi: Deep Vein Thrombosis
Venous thrombi usually form in the deep veins of the legs, known as deep vein thrombosis (DVT). They can happen when blood doesn’t move well or when the coagulation system is off balance. While they might not cause as much immediate harm as arterial thrombi, they can be deadly if they break loose and go to the lungs.
- Risk factors for DVT include prolonged immobilization, surgery, cancer, and genetic predispositions to clotting.
- Symptoms may include swelling, pain, and redness in the affected limb.
- Early diagnosis and treatment are critical to prevent complications.
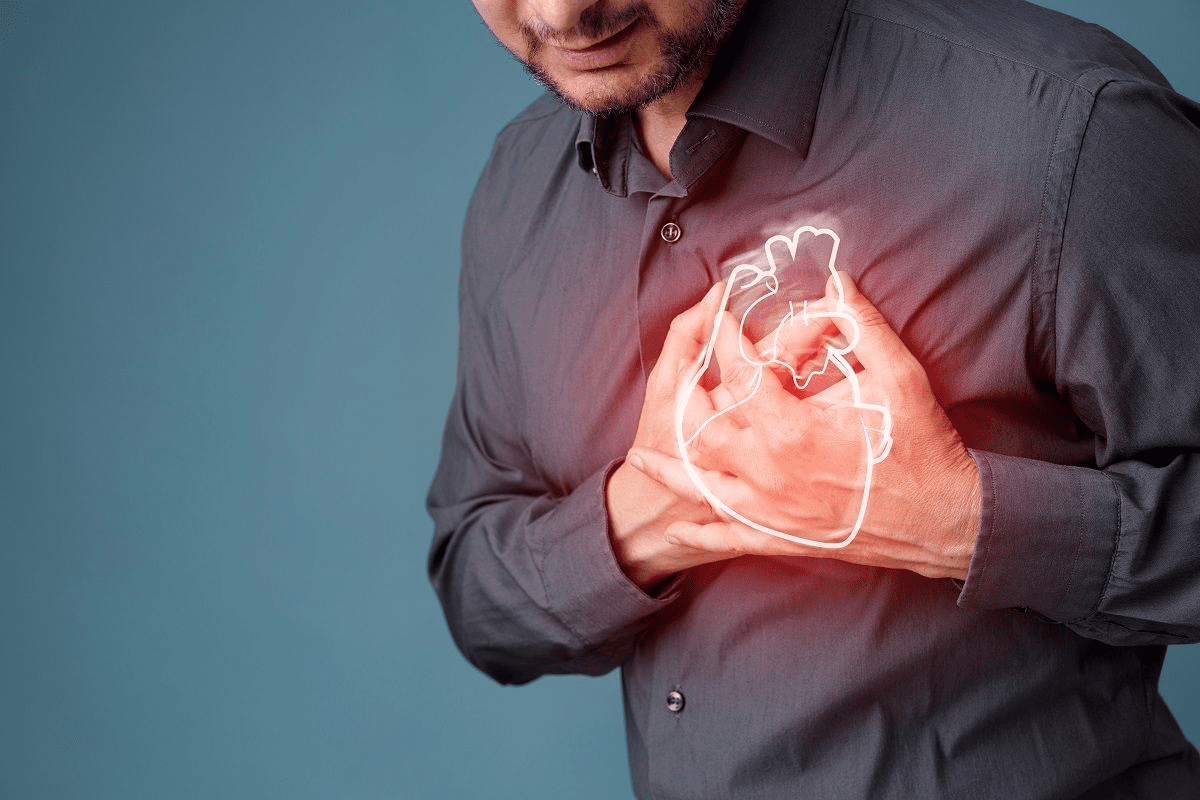
Cardiac Thrombi: Formation in Heart Chambers
Cardiac thrombi form in the heart chambers, often due to abnormal blood flow or after a heart attack. They can be very dangerous because they can travel to the brain or other organs. The left atrium is a common place for these to form, mainly in people with atrial fibrillation.
Key factors contributing to cardiac thrombi include:
- Atrial fibrillation, which leads to blood stasis in the left atrium.
- Recent myocardial infarction, which can damage the endocardium and lead to clot formation.
- Cardiac chamber dysfunction, reducing the heart’s ability to efficiently pump blood.
In conclusion, knowing about the different types of thrombi and their characteristics is vital for managing and treating them. By understanding the unique causes and features of arterial, venous, and cardiac thrombi, healthcare providers can improve patient care.
Common Locations for Thrombus Development
Thrombi can form in many parts of the body. Each location has its own risks and complications. It’s important to know where they usually appear.
Cerebral Thrombi and Stroke Risk
Cerebral thrombi happen in the brain’s blood vessels. They are a big reason for ischemic strokes. If a thrombus blocks a brain vessel, it can damage brain tissue.
This damage is because of a lack of oxygen and nutrients. It can lead to serious brain problems.
Things like high blood pressure, diabetes, and atherosclerosis increase the risk of cerebral thrombi. It’s key to manage these risks to prevent strokes.
Coronary Thrombi and Heart Attacks
Coronary thrombi form in the heart’s blood supply arteries. If a coronary thrombus blocks blood flow, it can cause a heart attack.
Coronary thrombi often start with atherosclerotic plaque rupture. This starts the blood clotting process. Finding and treating coronary thrombi quickly is critical.
Peripheral Thrombi in Limbs
Peripheral thrombi can happen in the arteries or veins of the limbs. Arterial thrombi can cause sudden limb ischemia. This is marked by pain, pale skin, no pulse, coldness, numbness, and weakness.
Venous thrombi, by contrast, can lead to deep vein thrombosis (DVT). DVT causes swelling, pain, and warmth in the affected limb. If a venous thrombus breaks loose, it can travel to the lungs, causing a pulmonary embolism.
| Location | Associated Risk | Common Causes |
| Cerebral | Ischemic Stroke | Hypertension, Diabetes, Atherosclerosis |
| Coronary | Myocardial Infarction | Atherosclerotic Plaque Rupture |
| Peripheral | Acute Limb Ischemia or DVT | Atherosclerosis, Immobility, Trauma |
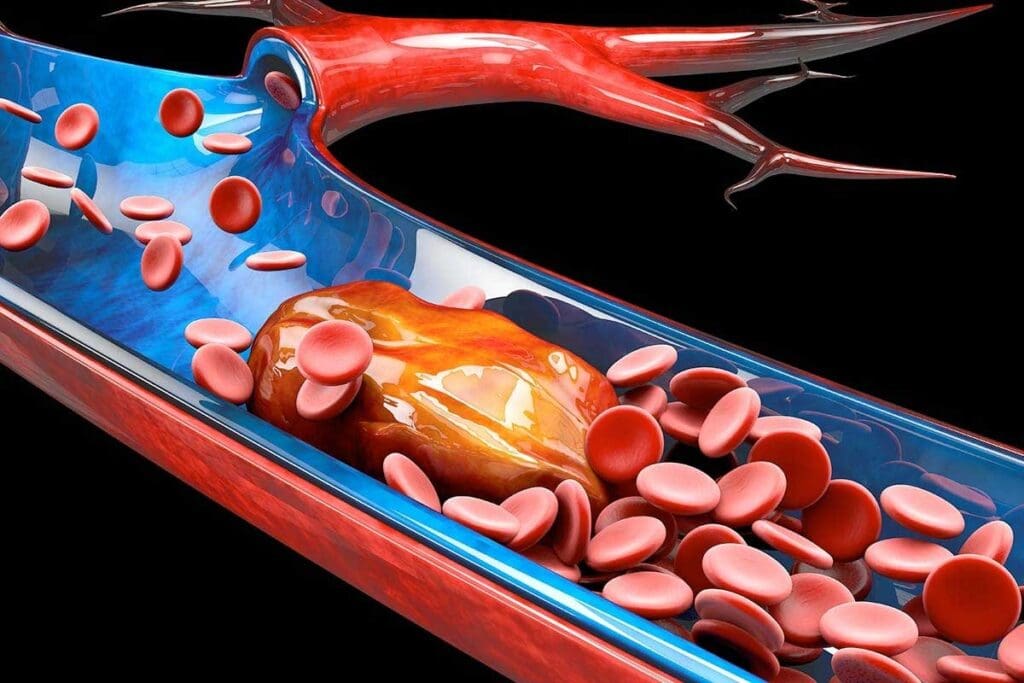
From Thrombus to Embolus: A Dangerous Transition
A thrombus turning into an embolus is a serious event. It can lead to severe health issues. When a thrombus breaks free, it can block vital organs or limbs.
How Thrombi Break Free and Become Emboli
Thrombi can break free due to changes in blood flow or pressure. The body’s fibrinolytic activity also plays a role. Once free, the thrombus becomes an embolus and travels through the blood.
The risk of a thrombus breaking free depends on its composition, size, and location. For example, a thrombus with a lot of fibrin is more likely to break loose.
| Factors Influencing Thrombus Dislodgement | Description |
| Composition | Thrombi with high fibrin content are more prone to embolization. |
| Size | Larger thrombi are more likely to cause significant embolic events. |
| Location | Thrombi in areas of high blood flow or turbulence are more likely to dislodge. |
The Path of an Embolus Through the Circulatory System
An embolus travels through the blood until it gets stuck in a small vessel. This can cause tissue damage and serious health issues.
An embolus from the heart can cause a stroke. One going to the lungs can lead to a pulmonary embolism. The symptoms depend on where the embolus ends up.
“The clinical implications of an embolus are vast and can range from mild symptoms to life-threatening conditions, stressing the need for quick medical action.”
Cardiologist
It’s key for healthcare providers to understand how a thrombus turns into an embolus. This knowledge helps them manage and prevent these dangerous events.
Risk Factors for Thrombus Development
It’s important to know what can lead to thrombus formation. We’ll look at genetic factors, lifestyle choices, and medical conditions that increase the risk.
Genetic Predispositions to Thrombosis
Genetics can greatly affect your risk of getting a thrombus. Some genetic conditions make blood clotting more likely. For example, Factor V Leiden is a mutation that raises clotting risk. Knowing these genetic risks helps us tailor care plans.
- Inherited thrombophilias
- Family history of thrombotic events
- Genetic mutations affecting clotting factors
Lifestyle Factors That Increase Risk
Our lifestyle choices can also raise the risk of thrombus. For instance, smoking and obesity are known risks. We recommend a healthy lifestyle to lower these risks.
- Prolonged immobility
- Smoking and tobacco use
- Obesity and lack of physical activity
Medical Conditions Associated with Thrombus Formation
Some medical conditions also increase thrombus risk. Atrial fibrillation, deep vein thrombosis, and cancer are examples. Managing these conditions is key to preventing thrombosis.
| Medical Condition | Risk Factor for Thrombus |
| Atrial Fibrillation | Increased risk of stroke due to clot formation |
| Cancer | Hypercoagulability associated with malignancy |
| Deep Vein Thrombosis | Direct formation of thrombi in deep veins |
Understanding these risk factors helps us prevent and manage thrombosis. This improves patient outcomes.
Thrombus Definition in Clinical Practice
Diagnosing a thrombus in clinical practice uses imaging and lab tests. These methods help us detect and understand its effects. They guide our treatment choices and aim to improve patient care.
Identifying thrombus formation is key in treating heart diseases and strokes. It lets doctors start the right treatments quickly.
Diagnostic Techniques for Detecting Thrombi
Many methods help find thrombi, each with its own strengths and uses. Here are some:
- Ultrasound: A non-invasive tool great for finding thrombi in veins and arteries.
- Computed Tomography (CT) scans: Gives detailed images to spot thrombi in places like the lungs and abdomen.
- Magnetic Resonance Imaging (MRI): Offers clear images for diagnosing thrombi in hard-to-reach areas.
- Angiography: An invasive method that uses contrast to see thrombi in blood vessels.
These imaging methods are often backed up by clinical checks and lab tests to confirm a thrombus.
Biomarkers and Laboratory Tests
Besides imaging, biomarkers and lab tests are vital for diagnosing thrombi. Important biomarkers include:
| Biomarker | Clinical Significance |
| D-dimer | High levels suggest fibrin breakdown, often linked to thrombi. |
| Troponin | High troponin levels can mean heart damage, possibly from coronary thrombi. |
Lab tests like complete blood counts and coagulation profiles offer more clues for diagnosing thrombi.
“Using biomarkers and imaging together makes diagnosing thrombi more accurate. This helps us target treatments better.”
— Cardiologist
By combining these diagnostic methods, we can better detect and manage thrombi. This improves patient care overall.
Treatment Approaches for Thrombus
Treating thrombus requires a mix of medical therapies and interventions. The right treatment depends on the thrombus’s type, location, and severity. It also depends on the patient’s health.
Anticoagulant Therapies
Anticoagulant therapies are key in managing thrombus. These drugs stop new thrombi from forming and prevent existing ones from growing. Heparin and warfarin are common anticoagulants used. Newer drugs like dabigatran, rivaroxaban, and apixaban offer different benefits and fewer side effects.
Anticoagulant therapies help prevent thrombus growth and embolism. But, they must be monitored closely to avoid bleeding risks.
Thrombolytic Medications
Thrombolytic medications dissolve formed thrombi. Drugs like alteplase and reteplase activate the body’s clot-dissolving system. They are vital in treating acute ischemic stroke and myocardial infarction.
These medications are given intravenously or directly to the thrombus via catheter. The choice depends on the situation and the thrombus’s location.
Surgical Interventions for Thrombus Removal
Surgical removal may be needed for some thrombi. This involves removing the thrombus through surgery or minimally invasive methods.
Catheter-directed thrombectomy is a less invasive option. It uses a catheter to deliver drugs or mechanically remove the thrombus. Surgery is usually for when other treatments fail or are not possible.
In conclusion, treating thrombus is highly personalized. It requires a detailed look at the patient and the thrombus. By knowing the different treatments, like anticoagulants, thrombolytics, and surgery, we can tailor care for each patient.
Prevention Strategies for Thrombosis
To prevent thrombosis, we need to make lifestyle changes and use medical treatments. Knowing and using these strategies can lower the risk of thrombosis. This can also prevent serious complications.
Lifestyle Modifications to Reduce Risk
Making lifestyle changes is key to preventing thrombosis. Regular physical activity is important. It improves blood flow and lowers clot risk. We suggest doing at least 30 minutes of moderate exercise daily.
- Keep a healthy weight to ease vein pressure.
- Avoid sitting for long periods, like on long trips.
- Drink lots of water to stay hydrated.
- Don’t smoke, as it harms blood vessels and increases clot risk.
Eating a balanced diet is also important. Foods rich in fruits, vegetables, and whole grains help manage cholesterol and blood pressure. This reduces thrombosis risk.
Prophylactic Medications and Their Use
Sometimes, just changing your lifestyle isn’t enough. Prophylactic medications like anticoagulants might be needed for high-risk individuals. These drugs stop blood clots from forming.
Here are some common medications:
- Warfarin: An oral anticoagulant that needs regular blood checks.
- Direct Oral Anticoagulants (DOACs): Newer drugs with easier dosing and no need for blood tests.
- Aspirin: Helps prevent arterial clots.
It’s important to take your medicine as directed. Also, keep up with doctor visits to adjust treatment if needed.
Teaching patients about thrombosis prevention is vital. By understanding the risks and taking action, people can lower their chance of getting thrombosis.
COVID-19 and Thrombus: Emerging Research
Research on COVID-19 is growing, showing a link between the virus and thrombi. The pandemic has made it clear how important it is to understand this connection. This is true, mainly in severe cases.
Microclots in COVID-19 Patients
Studies have found microclots in COVID-19 patients. These small clots can block tiny blood vessels, causing organ problems. Even after treatment, these microclots can stay, leading to concerns about better treatments.
Microclots in COVID-19 patients might be linked to persistent symptoms and long-term issues. This changes how we treat patients after they’ve had COVID-19.
Long-Term Implications for Post-COVID Care
Thrombus formation in COVID-19 patients is a long-term worry. As we deal with the pandemic, post-COVID care must focus on preventing blood clots. This might mean longer use of blood thinners, changes in lifestyle, and watching for clot signs.
There’s also a risk of long-term heart problems in those who had blood clots from COVID-19. This shows we need a full plan for post-COVID care that meets these patients’ complex needs.
Conclusion: Understanding the Significance of Thrombus in Modern Medicine
Knowing what thrombus means is key in today’s medicine. It’s vital for diagnosing, treating, and preventing blood clots. We’ve looked into what thrombus is, its makeup, and how it forms. We’ve also talked about the risks and signs of blood clots.
Thrombus is very important in today’s medicine. It’s a big cause of heart attacks and strokes. At LivHospital, we focus on caring for patients with blood clot issues. We use the newest ways to diagnose and treat, like medicines and surgery.
More research and learning are needed to help patients more. By understanding thrombus, we can find better ways to stop and treat blood clots. This will help improve lives for people all over the world.
FAQ
What is a thrombus in medical terms?
A thrombus is a blood clot that forms inside a blood vessel or heart chamber. It can cause serious health problems.
What is the difference between a thrombus and an embolus?
A thrombus is a blood clot in a blood vessel. An embolus is a clot that breaks free and travels, causing blockages elsewhere.
What are the components of a thrombus?
A thrombus is made of platelets, fibrin, and blood cells. The structure can change based on where it forms in the blood vessels.
What is thrombosis, and how does it relate to thrombus formation?
Thrombosis is the process of forming a thrombus. It involves the coagulation cascade. In Turkish, it’s called “thromboz”.
What are the different types of thrombi, and how do they differ?
There are arterial, venous, and cardiac thrombi. Each has its own causes, features, and risks, depending on where they form in the body.
Where are thrombi most likely to develop, and what are the associated risks?
Thrombi can form in the brain, heart, or limbs. Each location has its own risks, like stroke, heart attack, or limb problems.
What are the risk factors that contribute to thrombus development?
Risk factors include genetics, lifestyle, and certain health conditions. These can increase the chance of thrombosis.
How are thrombi diagnosed in clinical practice?
Diagnosis uses imaging and lab tests, like biomarkers. These help find and understand thrombi.
What are the treatment options for thrombi, and how are they chosen?
Treatment includes anticoagulants, thrombolytics, and surgery. The choice depends on the thrombus’s type, location, and impact.
How can the risk of thrombosis be reduced, and what role does patient education play?
Prevention involves lifestyle changes and medications. Patient education is key in managing thrombosis risk.
Is there a link between COVID-19 and thrombus formation?
Research shows COVID-19 may increase thrombus risk, including microclots. This could affect long-term care after COVID.
What is the significance of understanding thrombus in modern medicine?
Understanding thrombus is vital for treating patients with thrombotic disorders. It highlights the need for ongoing research and education.
References
- National Heart, Lung, and Blood Institute. (2022). Thrombosis. U.S. Department of Health and Human Services.https://www.nhlbi.nih.gov/health/thrombosis