Pregnancy changes a woman’s body a lot, making blood clotting risks higher. Medical data shows pregnant people are 5 times more likely to get a blood clot than non-pregnant ones.
Blood clotting disorders, like deep vein thrombosis and pulmonary embolism, are serious. They can harm both the mother and the baby. It’s important to know why they happen and how to manage them.
Key Takeaways
- Pregnancy increases the risk of blood clotting problems.
- Blood clotting disorders can endanger maternal and fetal health.
- Understanding the causes is key to managing these conditions.
- Proper management ensures the well-being of both mother and baby.
- Liv Hospital provides top-tier care for clotting disorders during pregnancy.
Understanding Blood Clotting During Pregnancy
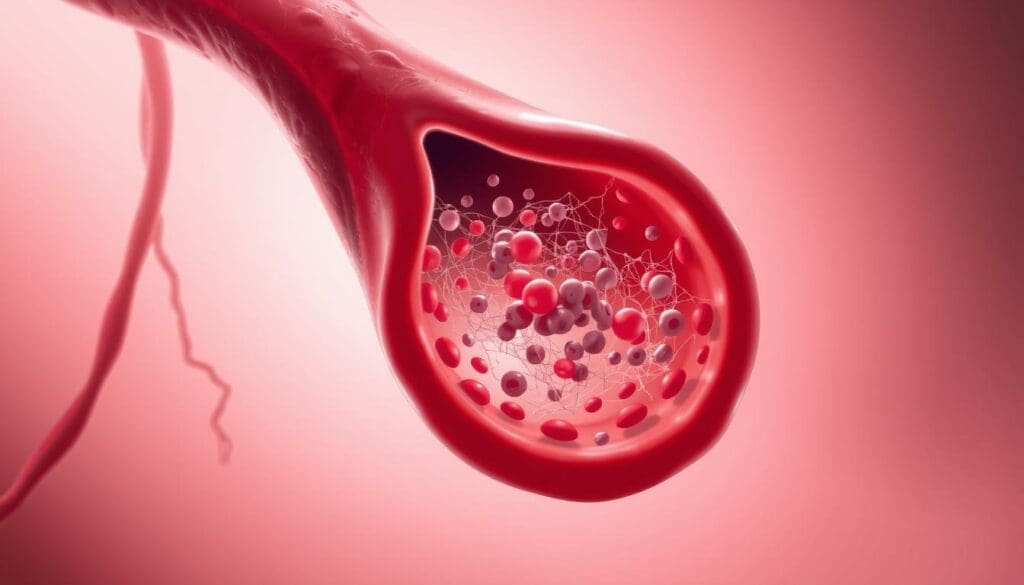
It’s important to know how blood clotting changes during pregnancy. This knowledge helps manage risks. Pregnancy brings big changes to how blood clots, affecting the risk of clots.
Normal Physiological Changes in Pregnancy
Pregnancy brings many changes to get ready for childbirth. One key change is the body’s tendency to clot blood more. This helps prevent too much blood loss during delivery.
Increased clotting factors are made during pregnancy. This makes blood more likely to clot. While it’s a normal change, it also raises the risk of unwanted clots.
Why Pregnancy Increases Clotting Risk Fivefold
Pregnancy makes clotting risk fivefold higher. This is due to several factors, like changes in blood and reduced leg blood flow. The growing uterus also puts pressure on blood vessels in the pelvis.
“The risk of venous thromboembolism is significantly increased during pregnancy and the postpartum period, making it a leading cause of maternal morbidity and mortality.”
Reduced Blood Flow in the Legs During Pregnancy
As the baby grows, it can press on blood vessels in the pelvis. This reduces blood flow to the legs. This can lead to a higher risk of clotting, mainly in the deep veins of the legs, known as Deep Vein Thrombosis (DVT).
| Physiological Change | Effect on Clotting Risk |
| Increased clotting factors | Increased risk of clot formation |
| Reduced blood flow in legs | Increased risk of DVT |
| Pressure on pelvic blood vessels | Reduced blood flow, increased clotting risk |
Knowing these changes is key to managing blood clotting risks in pregnancy. Healthcare providers can take steps to lower these risks by understanding these factors.
Clotting Disorder Pregnancy: Types and Manifestations

It’s important to know about clotting disorders in pregnancy. They can cause serious problems for both mom and baby. Knowing the types and how they show up is key to managing risks.
There are many clotting disorders that can happen during pregnancy. Each one has its own signs and risks. These include deep vein thrombosis (DVT), pulmonary embolism (PE), and inherited and acquired thrombophilias.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a blood clot in a vein deep in the body. It usually happens in the lower leg or thigh. Pregnancy makes it more likely because of changes in blood volume and vein pressure.
Symptoms of DVT may include:
- Swelling of the affected limb
- Pain or tenderness
- Warmth or redness of the skin
Pulmonary Embolism
Pulmonary embolism happens when a blood clot travels to the lungs. It’s a serious condition that needs quick medical help.
Common symptoms of pulmonary embolism include:
- Shortness of breath
- Chest pain that worsens with deep breathing
- Coughing up blood
Inherited and Acquired Thrombophilias
Thrombophilias are conditions that make blood clots more likely. They can be inherited or caused by other factors. Inherited ones include Factor V Leiden, while acquired ones might come from antiphospholipid syndrome.
| Type of Thrombophilia | Description | Risks During Pregnancy |
| Factor V Leiden | Inherited condition affecting blood clotting | Increased risk of DVT and PE |
| Antiphospholipid Syndrome | Acquired autoimmune disorder | Increased risk of clotting and pregnancy complications |
Knowing about clotting disorders and their signs is vital for pregnancy management. Early detection and treatment can greatly improve outcomes for both mom and baby.
Risk Factors for Developing Blood Clots While Pregnant
Blood clots during pregnancy can be caused by genetics, medical conditions, and lifestyle. Knowing these factors helps spot and manage blood clotting disorders early.
Genetic Predisposition and Family History
Women with a family history of clotting disorders face a higher risk of blood clots during pregnancy. Genetic thrombophilias, like Factor V Leiden, can greatly increase this risk. If you have a family history, talk to your healthcare provider about it.
“A family history of venous thromboembolism is a significant risk factor for pregnant women, and awareness of this history can guide preventive measures.”
Dr. Jane Smith, Obstetrician
Previous Blood Clot History
Having had blood clots before is a big risk factor. Women who’ve had DVT or pulmonary embolism are more likely to clot again during pregnancy. Previous clotting incidents suggest an underlying clotting disorder that pregnancy may worsen.
| Risk Factor | Description | Impact on Pregnancy |
| Genetic Predisposition | Inherited conditions like Factor V Leiden | Increased risk of blood clots |
| Previous Blood Clot | History of DVT or pulmonary embolism | Higher risk of recurrent clotting events |
| Lifestyle Factors | Obesity, smoking, and prolonged immobility | Contributes to increased clotting risk |
Lifestyle and Medical Factors
Lifestyle and medical factors also affect blood clot risk during pregnancy. Obesity, smoking, and prolonged immobility raise the risk. Certain medical conditions and some medications, like estrogen-containing contraceptives, also increase the risk.
Pregnant women should know about these risk factors and talk to their healthcare provider. Early action to manage these risks can lower the chance of blood clots and complications during pregnancy.
How Blood Clotting Disorders Affect Maternal Health
Blood clotting disorders in pregnancy can cause serious health issues for the mother. These include a higher risk of stroke and preeclampsia. It’s important for pregnant women to know about these risks and symptoms.
Immediate Health Risks
Blood clotting disorders can lead to serious health problems for pregnant women. These include blood clots in the deep veins (DVT) or lungs (PE). These conditions are dangerous and need quick medical help. Quick diagnosis and treatment are key to avoiding serious issues.
Risk of Stroke and Other Serious Complications
Women with blood clotting disorders face a higher risk of stroke during or after pregnancy. This risk is higher if they also have high blood pressure or preeclampsia. It’s important to monitor and manage these risks to keep the mother safe. For more info on managing blood clots during pregnancy, visit https://www.hematology.org/education/patients/blood-clots/pregnancy.
Preeclampsia and Its Relationship to Clotting Disorders
Preeclampsia is a pregnancy complication with high blood pressure and organ damage. Blood clotting disorders can raise the risk of preeclampsia. Knowing this is key for early detection and treatment in pregnant women with clotting disorders.
When to Seek Immediate Medical Attention
Pregnant women with blood clotting disorders should know when to get medical help fast. Symptoms like severe headache, vision changes, severe abdominal pain, or trouble breathing are urgent. Knowing these symptoms can save lives.
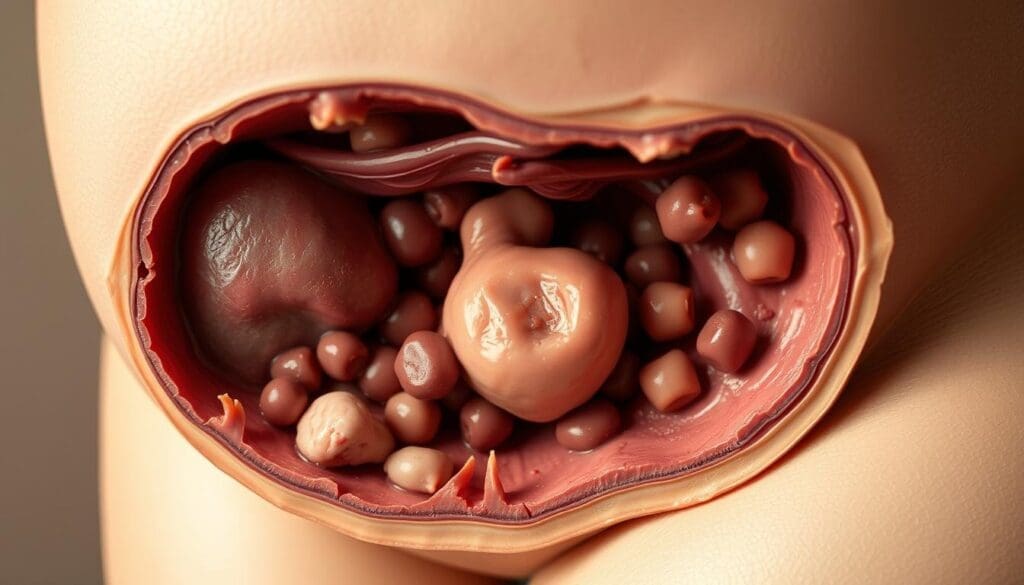
Impact of Clotting Disorders on Fetal Development
Clotting disorders during pregnancy can harm fetal development. They can lead to reduced blood flow to the placenta. This can harm the fetus.
Intrauterine Growth Restriction
Intrauterine growth restriction (IUGR) happens when a fetus doesn’t grow as it should. Clotting disorders can cause IUGR by reducing blood flow to the placenta. The placenta is key for the fetus’s growth and development.
Risk Factors for IUGR:
- Presence of clotting disorders
- History of previous IUGR pregnancies
- Placental insufficiency
Placental Insufficiency
Placental insufficiency is when the placenta can’t provide enough oxygen and nutrients to the fetus. Clotting disorders can cause blood clots in the placenta. This reduces its ability to function properly.
Miscarriage and Pregnancy Loss
Clotting disorders increase the risk of miscarriage and pregnancy loss. Blood clots can disrupt the fetus’s normal development. This can lead to pregnancy complications.
The risk factors for miscarriage due to clotting disorders include:
- Previous history of miscarriage
- Family history of clotting disorders
- Presence of antiphospholipid syndrome
Long-term Effects on Child Development
Children born to mothers with clotting disorders may face long-term developmental challenges. These can include cognitive, emotional, and physical delays.
| Potential Long-term Effects | Description |
| Cognitive Delays | Difficulties with learning and memory |
| Emotional Developmental Issues | Increased risk of emotional and behavioral problems |
| Physical Developmental Delays | Delays in physical growth and motor skills development |
Diagnosis and Detection of Blood Clotting Disorders
Early detection of blood clotting disorders is key for pregnant women. It allows for timely treatment and management. Diagnosing these conditions involves a combination of medical history, physical examination, and various diagnostic tests.
Screening Tests and When They’re Recommended
Screening tests for blood clotting disorders are not routine for all pregnant women. They are recommended for those with a personal or family history of blood clots or certain genetic predispositions. Common screening tests include:
- Complete Blood Count (CBC)
- Prothrombin Time (PT) and Partial Thromboplastin Time (PTT)
- Fibrinogen level tests
These tests help identify abnormalities in blood clotting. They can indicate the presence of a clotting disorder.
Genetic Testing for Inherited Thrombophilias
Genetic testing is available for inherited thrombophilias, such as Factor V Leiden and Prothrombin G20210A mutation. This testing is usually recommended for women with a family history of blood clots or recurrent miscarriages.
| Genetic Mutation | Risk Associated |
| Factor V Leiden | Increased risk of DVT and PE |
| Prothrombin G20210A | Higher risk of venous thromboembolism |
Diagnosing Autoimmune Conditions Like Antiphospholipid Syndrome
Antiphospholipid syndrome (APS) is an autoimmune disorder that can cause blood clots and pregnancy complications. Diagnosis involves detecting specific antibodies in the blood. It also requires clinical criteria such as a history of blood clots or pregnancy loss.
“The diagnosis of antiphospholipid syndrome requires a combination of clinical and laboratory criteria, highlighting the need for a thorough assessment.”
Early Detection Strategies for High-Risk Women
For women at high risk of blood clotting disorders, early detection strategies are important. This includes regular monitoring of clotting parameters and close surveillance for signs of thrombosis. Healthcare providers may also recommend prophylactic anticoagulation therapy in some cases.
Understanding diagnostic approaches and detection strategies helps healthcare providers manage blood clotting disorders in pregnancy. This improves outcomes for both mother and baby.
Treatment Approaches for Managing Clotting Disorders
Managing clotting disorders during pregnancy is key for the health of both mom and baby. Treatment often includes anticoagulant therapy and close monitoring. This helps lower the risk of problems.
Anticoagulant Therapy Options
Anticoagulant therapy is vital for managing clotting disorders in pregnancy. Low-molecular-weight heparin (LMWH) and unfractionated heparin (UFH) are safe choices. Studies show LMWH is safer with fewer side effects.
“Anticoagulant therapy during pregnancy greatly lowers the risk of blood clots,” notes a leading expert.
“Tailored anticoagulant therapy is key to achieving positive outcomes.”
Monitoring and Adjusting Treatment Throughout Pregnancy
Regular checks are key to fine-tuning treatment as pregnancy progresses. Blood tests help see if therapy is working and watch for side effects. Dosage or type of therapy might need to change for best results.
Recent Advances in Tailored Anticoagulant Therapy
New developments in anticoagulant therapy have led to more personalized care. Tailored anticoagulant therapy picks the best treatment based on each patient’s needs. This approach has shown to improve outcomes for pregnant women with clotting disorders.
In summary, managing clotting disorders in pregnancy needs a full treatment plan. This includes anticoagulant therapy, regular checks, and adjusting treatment as needed. A personalized approach to anticoagulant therapy helps reduce risks and ensures the best results for mom and baby.
Delivery and Postpartum Management for Women with Clotting Disorders
Women with clotting disorders need a special plan for delivery and after birth. They must be watched closely to avoid blood clots, which are a big risk during this time.
Planning for Safe Delivery
Safe delivery planning is key for women with clotting disorders. Doctors, hematologists, and other experts work together. They might adjust anticoagulant therapy before delivery to lower bleeding risks.
When to deliver is also important. Sometimes, induction of labor is suggested. This helps manage any problems right away.
Managing Anticoagulation During Labor and Delivery
Keeping anticoagulation in check during labor and delivery is tricky. It’s about stopping clots without causing too much bleeding. Low Molecular Weight Heparin (LMWH) is often stopped 24 hours before delivery.
| Anticoagulant | Management During Labor | Management Post-Delivery |
| LMWH | Discontinued 24 hours before delivery | Resumed 4-6 hours post-delivery |
| Unfractionated Heparin | Stopped during active labor | Resumed post-delivery as directed |
Postpartum Vigilance and Extended Treatment
After birth, women with clotting disorders need extra care. The risk of blood clots is higher after giving birth. Postpartum anticoagulation helps lower this risk.
How long to keep taking anticoagulants varies. It depends on the woman’s risk and other health issues. Usually, it’s for 6 weeks after birth.
Breastfeeding Considerations with Anticoagulant Therapy
Breastfeeding is usually safe for women on anticoagulant therapy. It’s important to pick an anticoagulant that’s okay for breastfeeding. Warfarin and LMWH are safe because they don’t get into breast milk much.
Women should talk to their doctor about their treatment and breastfeeding. It’s also good to watch for any bleeding in the baby.
Conclusion: Living Well with Clotting Disorders During Pregnancy
Women with clotting disorders can have a good pregnancy with the right care. Testing and treatment are key to keep both mom and baby safe.
Recent studies show early detection and regular checks are vital. Tailored anticoagulant therapy helps too. This way, women can lower risks and have a healthy pregnancy.
Managing clotting disorders in pregnancy needs careful planning. The right treatment can lower serious risks. This includes anticoagulant therapy, regular checks, and a planned delivery.
By being proactive, women with clotting disorders can have a positive pregnancy. This ensures the best health for both mom and baby.
FAQ
What are the risks associated with blood clotting disorders during pregnancy?
Blood clotting disorders during pregnancy can lead to serious issues. These include deep vein thrombosis and pulmonary embolism. Both can harm the mother and the baby.
Why does pregnancy increase the risk of blood clotting?
Pregnancy changes the body in ways that increase clotting risk. For example, blood volume goes up and blood flow in the legs goes down. This can make clotting five times more likely.
What are the different types of clotting disorders that can occur during pregnancy?
Pregnancy can cause several clotting disorders. These include deep vein thrombosis and pulmonary embolism. Inherited and acquired thrombophilias, like antiphospholipid syndrome, are also risks.
What are the risk factors for developing blood clots during pregnancy?
Several factors can increase the risk of blood clots during pregnancy. These include genetic predisposition and family history. Previous blood clot history and lifestyle factors, like obesity, also play a role.
How do blood clotting disorders affect maternal health?
Blood clotting disorders can pose immediate risks. These include deep vein thrombosis and pulmonary embolism. They can also lead to long-term health issues, such as stroke and heart disease.
Can blood clotting disorders affect fetal development?
Yes, they can. Blood clotting disorders can harm fetal development. They increase the risk of growth restriction and miscarriage. They can also affect a child’s long-term development.
How are blood clotting disorders diagnosed during pregnancy?
Diagnosing these disorders involves several steps. Screening tests and genetic testing are used. Autoimmune conditions, like antiphospholipid syndrome, are also diagnosed.
What are the treatment approaches for managing clotting disorders during pregnancy?
Managing these disorders includes anticoagulant therapy. Treatment is monitored and adjusted as needed. New approaches to tailored therapy are also being explored.
How are women with clotting disorders managed during delivery and postpartum?
Managing these disorders during delivery and postpartum is key. Safe delivery planning and anticoagulation management are important. Extended treatment and breastfeeding considerations are also vital.
Can women with clotting disorders breastfeed while on anticoagulant therapy?
Discussing breastfeeding with a healthcare provider is essential. Some anticoagulants are safe, while others may not be.
What is the importance of proper management and care for women with clotting disorders during pregnancy?
Proper management and care are critical. They help prevent complications and ensure the health of both mother and baby.





