At Liv Hospital, we know that blood clots can be both good and bad. They are called thrombi and form when blood turns gel-like. This usually happens to stop bleeding.
Blood clots are like jelly and can happen in arteries or veins. They can be in the heart, brain, lungs, or other places. While they help with injuries, they can be risky if they block blood flow or reach important organs.
It’s important to know about the different types of blood clots. We’ll look at the blood clot names and how they form. This will help us understand this complex health issue better.
Key Takeaways
- Blood clots can be lifesaving or life-threatening depending on their type and location.
- They form when blood changes from a liquid to a gel-like state, typically to prevent bleeding.
- Blood clots can occur in various parts of the body, including arteries and veins.
- Understanding the different types of blood clots is essential for effective care.
- Blood clots can become dangerous if they impede normal blood flow or travel to vital organs.
Understanding Blood Clots: The Basics
A blood clot, or thrombosis, is a solid mass formed from blood. It happens when blood turns from liquid to solid. This is important for stopping too much bleeding when we get hurt. But sometimes blood clots form without reason, which can be very dangerous.
What Are Blood Clots?
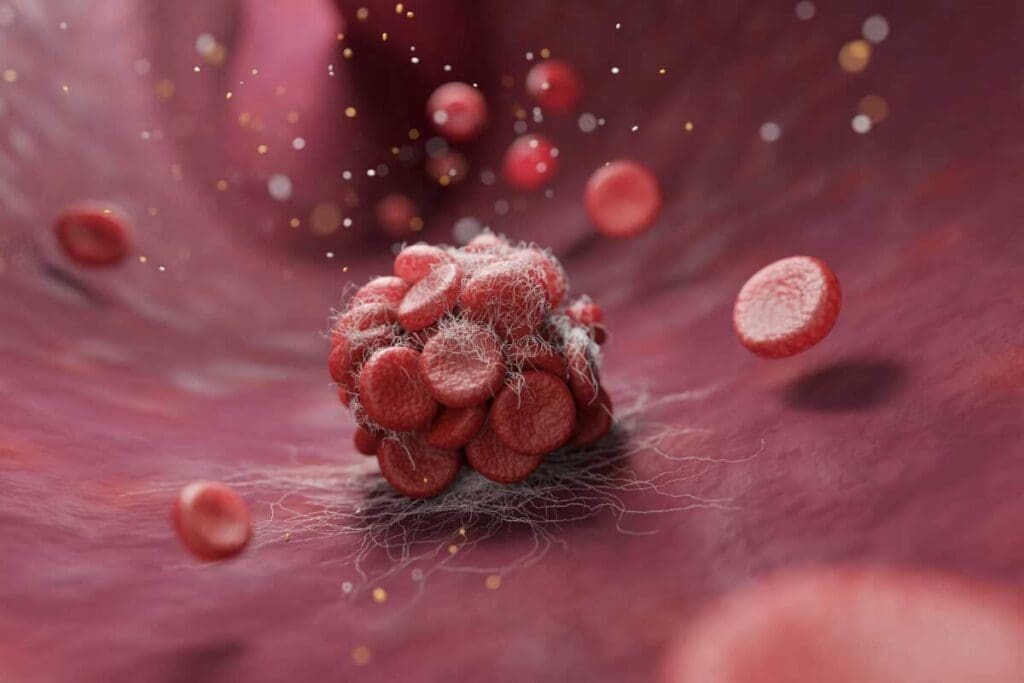
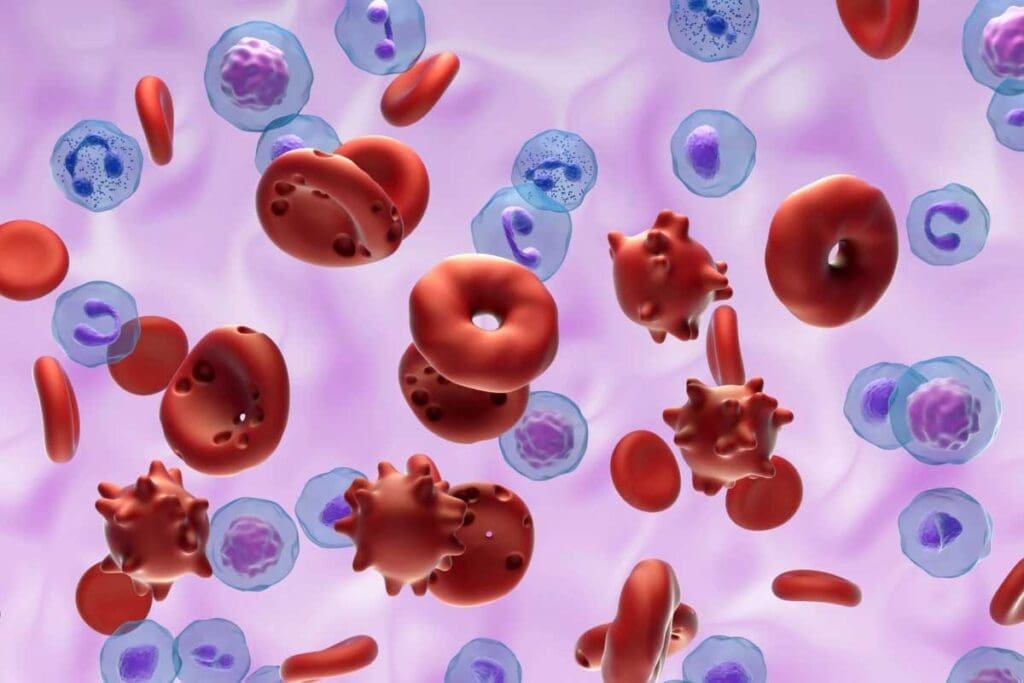
Blood clots are made of platelets, red blood cells, and fibrin, a protein that acts like glue. Understanding blood clots is key to knowing their role in health and disease.
The Blood Clotting Process
The clotting process, or coagulation, is a series of steps that form a fibrin clot. It starts with injury to a blood vessel. Here’s a quick look at how it works:
| Step | Description |
| 1. Injury | Blood vessel injury occurs, exposing the underlying tissue. |
| 2. Platelet Activation | Platelets adhere to the injury site and become activated. |
| 3. Clotting Factor Activation | Clotting factors are activated in a cascade, leading to fibrin formation. |
| 4. Fibrin Clot Formation | Fibrin strands form, trapping blood cells and platelets, creating a clot. |
There are different types of blood clots based on where they form and how they move. A stationary clot in a vein is called a thrombosis. An embolus is a clot that breaks loose and travels through the blood.
How Blood Clots Form in the Body
Blood clots form through a complex process. This process is called the coagulation cascade. It involves many clotting factors and cells.
The coagulation cascade is tightly controlled. It makes blood clots when needed but stops them from forming too much. It has two main paths: the intrinsic and extrinsic pathways.
The Coagulation Cascade
The cascade starts when a blood vessel is damaged. This damage exposes blood to tissue factor, starting the extrinsic pathway. The intrinsic pathway is triggered by blood touching negatively charged surfaces. Both paths meet to form a fibrin clot.
Many clotting factors are involved in this process. These factors, labeled with Roman numerals, are key to making a blood clot.
| Clotting Factor | Function |
| Factor I (Fibrinogen) | Converted to fibrin to form the clot |
| Factor II (Prothrombin) | Converted to thrombin, which converts fibrinogen to fibrin |
| Factor III (Tissue Factor) | Triggers the extrinsic pathway |
Factors That Trigger Clot Formation
Many things can start clot formation. These include injuries, inflammation, and certain health conditions. When a blood vessel is injured, the coagulation cascade starts to make a clot and stop bleeding.
“The coagulation pathway is a cascade of events that leads to hemostasis, allowing for rapid healing and prevention of spontaneous bleeding.”
At first, blood clots are soft and jelly-like. But they can harden over time. Knowing what triggers clot formation helps us understand the risks of different clots.
Understanding how blood clots form and what influences them is key. This knowledge helps us see why diagnosing and treating them is so important. The coagulation cascade is complex, and problems with it can cause serious health issues.
Physical Characteristics of Blood Clots
It’s important to know about blood clots’ physical traits for diagnosing and treating health issues. Blood clots can differ a lot in how they look and feel. This affects how we find and treat them.
Soft vs. Hard Blood Clots
Blood clots can be soft or hard, based on their makeup and age. At first, they might be soft and jelly-like. This makes them more likely to break apart.
As time goes on, these clots get harder and more solid. This happens through a process called fibrinization, which makes the clot stronger.
Soft clots are usually new and haven’t fully set yet. Hard clots are older and more solid. Knowing a clot’s texture can tell us a lot about its age and how stable it is.
Jelly-like Appearance and Texture
Some blood clots look and feel like jelly. This is because they have lots of red blood cells and fibrin strands. This jelly-like feel is common in newer clots.
The look and feel of blood clots can also change based on where they form in the body. Clots in veins might look different from those in arteries.
Changes in Clot Consistency Over Time
As blood clots get older, they change a lot. New clots are softer and more likely to break loose. Older clots get harder and more stable. Knowing these changes is key to managing and treating them.
| Clot Characteristic | Fresh Clot | Older Clot |
| Texture | Soft, jelly-like | Hard, organized |
| Composition | High in red blood cells, loose fibrin | More fibrin, contracted |
| Risk | Higher risk of embolization | Lower risk of embolization, more stable |
Healthcare experts can better diagnose and treat blood clots by knowing their physical traits. This knowledge is vital for creating effective treatments and improving patient care.
Different Types of Blood Clots: A Comprehensive Overview
Blood clots vary in how they form, what they’re made of, and where they occur. Knowing these differences is key for spotting and treating them.
Thrombus vs. Embolus: Understanding the Difference
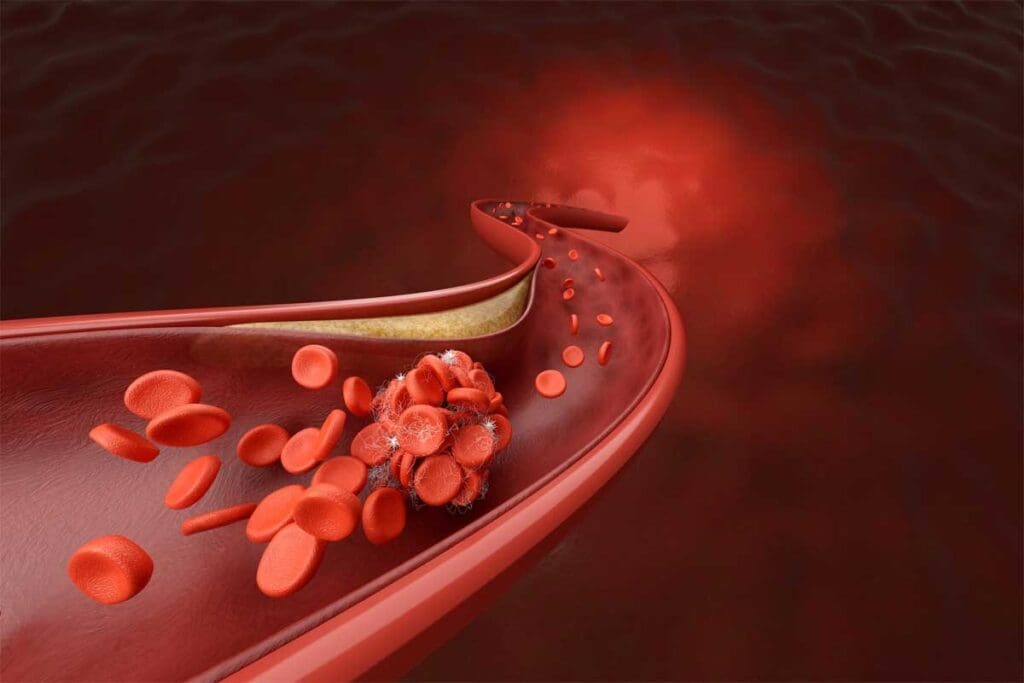
A thrombus is a blood clot that stays in one place in a blood vessel. An embolus, by contrast, breaks free and travels to block another area. This can cause severe issues like a pulmonary embolism or stroke.
Arterial vs. Venous Clots
Clots can also be divided by where they happen. Arterial clots block oxygen-rich blood flow, leading to heart attacks or strokes. Venous clots, found in veins, can cause deep vein thrombosis (DVT).
Classification Based on Location
Where a clot forms matters too. Clots can be in the legs (DVT), lungs (pulmonary embolism), brain (stroke), or heart (heart attack). Each spot has its own risks and treatment needs.
In summary, blood clots come in many types, each with its own set of challenges. By knowing the differences between thrombus and embolus, and where they occur, doctors can give better care.
Deep Vein Thrombosis (DVT): The Hidden Danger
It’s key to know about Deep Vein Thrombosis (DVT) risks for early treatment. DVT is when a blood clot forms in a deep vein, usually in the legs. This can be deadly if the clot moves to the lungs, causing a pulmonary embolism.
Common Locations for DVT
DVT often happens in the lower legs, like the calf, thigh, or pelvis. But it can also occur in other deep veins. These areas are more likely to clot because of the blood flow and pressure.
- Calf: Clots often form here due to prolonged immobility.
- Thigh: Clots in this area can be larger and more dangerous.
- Pelvis: Clots here can be risky because of their size and how hard they are to find.
Risk Factors and Symptoms
Many things can raise your risk of getting DVT, like prolonged immobility, surgery, cancer, and genetic predispositions. Knowing the symptoms is key to quick action. Common signs include:
- Swelling in the affected limb.
- Pain or tenderness, often described as a cramp or soreness.
- Warmth or redness of the skin over the affected area.
Statistics and Prevalence in the United States
DVT is a big problem in the United States. About 900,000 people get it every year, and up to 100,000 die from it. Knowing these numbers shows how important it is to be aware and take steps to prevent it.
Pulmonary Embolism (PE): When Clots Travel to the Lungs
A Pulmonary Embolism (PE) occurs when a clot moves from Deep Vein Thrombosis (DVT) to the lungs. This is a serious condition that can be deadly if not treated quickly.
Development of PE from DVT
PE usually starts when a blood clot breaks free from the deep veins in the legs. It then travels to the lungs. This can block a pulmonary artery, causing severe symptoms and serious health risks.
DVT is a major risk factor for PE. Research shows that without treatment, about 30% of patients with DVT in the legs may get PE. It’s important to understand this connection to catch and treat PE early.
Recognizing PE Symptoms
The symptoms of Pulmonary Embolism can vary. This makes it hard to diagnose. Common signs include:
- Shortness of breath
- Chest pain that gets worse with deep breathing
- Coughing up blood
- Rapid heart rate
- Lightheadedness or dizziness
It’s vital to notice these symptoms early and get medical help. Quick treatment can greatly improve the chances of recovery.
“Prompt recognition and treatment of Pulmonary Embolism can be lifesaving. Healthcare providers must be vigilant in identifying patients at risk and initiating appropriate diagnostic and therapeutic measures.”
Severity and Mortality Rates
The severity of Pulmonary Embolism can vary. The death rate for PE is high, making it a serious condition. The American Heart Association says PE is a top cause of death in pregnant women and can be fatal in other groups, like the elderly and those with health issues.
| Risk Factor | Mortality Rate |
| Untreated PE | Up to 30% |
| Promptly Treated PE | <5% |
| Pregnancy-related PE | Significantly higher than in non-pregnant women |
Knowing how serious PE is highlights the need for prevention, early detection, and effective treatment.
Arterial Thrombosis: Clots in the Arterial System
Arterial thrombosis happens when a clot blocks an artery. This stops blood from reaching vital organs. It can cause serious problems like heart attacks and strokes by cutting off oxygen and nutrients.
Causes and Risk Factors
Many things can lead to arterial thrombosis. Atherosclerosis, or plaque buildup, is a big cause. When this plaque bursts, it can start a blood clot. Other risks include high blood pressure, smoking, diabetes, and high cholesterol.
Lifestyle choices also play a part. Being inactive, overweight, or eating too much saturated fat can raise your risk. Knowing these risks helps prevent and treat the condition early.
Common Sites of Arterial Thrombosis
Arterial thrombosis can happen in different arteries. The coronary arteries, which feed the heart, and the carotid arteries, which supply the brain, are common spots. Clots here can cause heart attacks and strokes.
| Artery | Location | Potential Consequence |
| Coronary Artery | Heart | Heart Attack |
| Carotid Artery | Neck/Brain | Stroke |
| Femoral Artery | Leg | Peripheral Artery Disease |
It’s key to know the causes and risks of arterial thrombosis. This knowledge helps prevent it. By understanding where and how clots form, people can manage their risk better and get help when needed.
Superficial Venous Thrombosis and Coronary Thrombosis
Clots can form in veins near the skin or in the heart’s arteries. It’s important to know about these conditions to understand their risks and how to act.
Superficial Thrombophlebitis: Clots Near the Surface
Superficial thrombophlebitis happens when clots form in veins close to the skin. This can cause pain and swelling. We’ll look at what causes it, its symptoms, and how to treat it.
Causes and Symptoms: It often comes from varicose veins, vein injury, or infection. You might feel pain, see redness, and notice swelling.
Coronary Thrombosis and Heart Attacks
Coronary thrombosis is when a clot blocks a heart artery. This can lead to a heart attack, harming the heart muscle. We’ll talk about what causes it, its symptoms, and the dangers it poses.
Risk Factors: High blood pressure, high cholesterol, smoking, and diabetes increase the risk. Knowing these can help prevent coronary thrombosis.
| Condition | Causes | Symptoms |
| Superficial Thrombophlebitis | Varicose veins, trauma, and infection | Pain, redness, swelling |
| Coronary Thrombosis | High blood pressure, high cholesterol, smoking, and diabetes | Chest pain, shortness of breath, dizziness |
Small Clots: When to Worry
Not all clots are the same. Some are small and harmless, while others are dangerous. We’ll discuss when small clots are a concern and what makes them serious.
Small clots can be minor or serious, depending on where they are and why. For example, small clots in veins might be uncomfortable but are safer than clots in heart arteries, which can cause heart attacks.
Determining Severity: A clot’s danger depends on its size, location, and any health issues. We’ll explore how these factors affect a clot’s risk.
Diagnosing Different Types of Blood Clots
Diagnosing blood clots requires a mix of clinical checks and advanced imaging. It’s key to figure out the right treatment and avoid complications.
Clinical Assessment
The first step is a detailed clinical check. This looks at the patient’s health history, symptoms, and risk for clots. Doctors check for swelling, redness, and pain in the affected limb. They also consider the patient’s overall health and any conditions that might lead to clots.
A medical expert says,
“A thorough clinical check is vital for spotting high-risk patients and guiding more tests.”
Imaging Techniques
Imaging is critical for confirming blood clots. It uses various methods:
- Ultrasound: This non-invasive method uses sound waves to see blood vessels and find clots.
- MRI (Magnetic Resonance Imaging): MRI gives detailed images of the body’s inside, spotting clots in different spots.
- CT Scan (Computed Tomography): CT scans use X-rays to make detailed images, finding clots in the lungs or elsewhere.
Laboratory Tests
Laboratory tests are also key in diagnosing blood clots. They help find underlying conditions and assess risk. Common tests include:
- D-dimer test: This blood test checks D-dimer levels, a sign of clot dissolution.
- Complete Blood Count (CBC): A CBC looks for blood cell count issues that might show clotting or bleeding problems.
- Coagulation studies: These tests check blood clotting factors, helping diagnose clotting disorders.
By using clinical checks, imaging, and lab tests, doctors can accurately diagnose blood clots. They then create a treatment plan.
Treatment and Prevention Strategies
Treatment and prevention of blood clots need a detailed look. We’ll explore the many ways to manage blood clots. This includes understanding different treatments and lifestyle changes.
Medication Options
Anticoagulant medications are key in treating and preventing blood clots. They stop the body’s clotting process, lowering clot risk. Common ones are warfarin, apixaban, and rivaroxaban. It’s vital to follow a healthcare provider’s advice when taking these drugs.
Surgical Interventions
Sometimes, surgery is needed to treat blood clots. Procedures like thrombectomy remove the clot. Catheter-directed thrombolysis dissolves clots directly. These are for severe cases or when other treatments fail.
Lifestyle Changes to Prevent Blood Clots
Preventing blood clots means making big lifestyle changes. Regular exercise, a healthy weight, and avoiding sitting too long help. Quitting smoking and drinking less also lowers the risk.
Combining medication, surgery, and lifestyle changes helps manage and prevent blood clots. Working with healthcare providers is key to finding the right plan for you.
Conclusion: Understanding the Risks and Taking Action
It’s important to know about blood clot risks to keep your heart healthy. Blood clots can block blood flow, causing serious problems like deep vein thrombosis (DVT) and pulmonary embolism (PE). Spotting the signs and knowing the risk factors helps you act fast.
Acting against blood clots means knowing the dangers of different types. A clot moving in your blood, called an embolus, is very risky.
To lower your risk of blood clots, live a balanced life, drink plenty of water, and don’t stay too long without moving. Catching and treating clots early is key to avoiding big problems.
We urge you to take care of your health by learning about blood clot risks and acting when needed. This way, you can greatly lower your chance of serious blood clot-related conditions.
FAQ
What is a blood clot?
A blood clot is a mass of blood cells and proteins that stick together. This happens in response to injury or other factors.
What are the different types of blood clots?
There are many types of blood clots. These include thrombus, embolus, arterial clots, and venous clots. Each type has its own characteristics and effects.
What is the difference between a thrombus and an embolus?
A thrombus forms in a blood vessel. An embolus is a clot that breaks loose and travels through the blood. It can block other areas.
Are blood clots hard or soft?
Blood clots can be either soft or hard. Fresh clots are usually soft. Older clots become harder.
What is a stationary clot called?
A stationary clot is called a thrombus.
What is a clot that is circulating in the blood called?
A clot that moves in the blood is called an embolus.
What are the symptoms of Deep Vein Thrombosis (DVT)?
Symptoms of DVT include swelling, pain, and redness in the affected limb. Some cases may not show symptoms.
How is Pulmonary Embolism (PE) diagnosed?
PE is diagnosed with clinical assessment, imaging like CT scans, and lab tests.
What are the risk factors for developing arterial thrombosis?
Risk factors for arterial thrombosis include high blood pressure, high cholesterol, smoking, and diabetes.
How can blood clots be prevented?
Blood clots can be prevented with lifestyle changes. These include regular exercise, a healthy weight, and avoiding immobility. Medications like anticoagulants also help.
What is superficial thrombophlebitis?
Superficial thrombophlebitis is a condition where a clot forms in a superficial vein. It causes inflammation and pain.
What is coronary thrombosis?
Coronary thrombosis is when a clot forms in the coronary arteries. It can lead to a heart attack.
Are small clots a cause for concern?
Yes, small clots can be a concern. If they break loose and travel to critical areas, like the lungs or brain, they can cause serious problems.
References:
- Lurie, J. M. (2019). Virchow’s triad in “silent” deep vein thrombosis. Thrombosis Research, 184, 1–3. https://www.sciencedirect.com/science/article/pii/S2213333X19301702
- Alqahtani, J. S., & Aljohani, M. J. (2023). Deep Venous Thrombosis. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK507708/








