We are dedicated to sharing detailed info about B-ALL leukemia. This disease impacts the blood and bone marrow. It’s caused by too many immature B-cell lymphoblasts, making it a type of acute lymphoblastic leukemia (ALL).
B-ALL leukemia often hits kids, but it can also affect adults. Knowing the symptoms, how to diagnose it, and treatment choices is key. In this piece, we’ll dive into the essential facts about B ALL leukemia. We aim to give you important insights into this condition.
Key Takeaways
- Understanding B-ALL leukemia and its symptoms
- The importance of early diagnosis and treatment
- Overview of treatment options for B-ALL leukemia
- The role of multidisciplinary care in managing B-ALL
- Advances in research and prospects for B-ALL patients
What is B ALL Leukemia? Definition and Medical Terminology
B-Cell Acute Lymphoblastic Leukemia, or B-ALL, is a blood cancer. It affects the blood and bone marrow. It happens when immature B-cells grow too much in the bone marrow.
Knowing the medical terms for B-ALL is key for patients and doctors. The term “B-ALL” stands for B-Cell Acute Lymphoblastic Leukemia. It’s different from other leukemias because it affects B-cells, which are important for fighting infections.
Understanding B-Cell Acute Lymphoblastic Leukemia
B-Cell Acute Lymphoblastic Leukemia is a type of Acute Lymphoblastic Leukemia (ALL). It’s marked by the fast growth of immature B-cells. These cells can’t fight infections well. If not treated quickly, it can get worse fast.
B-ALL Medical Abbreviation Explained
The “B-ALL medical abbreviation” means B-Cell Acute Lymphoblastic Leukemia. Doctors and medical writers use it a lot. Knowing this term helps to understand medical records and talk to doctors better.
Differences Between B-ALL and Other Leukemia Types
B-ALL is different from other leukemias like Chronic Lymphocytic Leukemia (CLL) or Acute Myeloid Leukemia (AML). The main differences are the type of blood cell affected and how fast the disease grows. B-ALL affects B-cells and grows quickly.
| Leukemia Type | Cell Type Affected | Disease Progression |
| B-Cell Acute Lymphoblastic Leukemia (B-ALL) | B-cells | Acute/Rapid |
| Chronic Lymphocytic Leukemia (CLL) | B-cells | Chronic/Slow |
| Acute Myeloid Leukemia (AML) | Myeloid cells | Acute/Rapid |
The Biology and Pathophysiology of B-ALL Disease
B-ALL is a disease where bad B-cell precursors build up in the bone marrow. This stops normal blood cell making. It’s a key sign of the disease.
How B-ALL Affects Bone Marrow Function
The bone marrow makes all blood cells. In B-ALL, it’s filled with bad B-cell lymphoblasts. These cells can’t work right.
This messes up making healthy blood cells. Patients often get anemia, infections, and bleeding problems. This is because they don’t have enough good blood cells.
The Role of B-Cell Lymphoblasts in Disease Development
B-cell lymphoblasts are key in B-ALL. They don’t turn into good B cells. Good B cells help fight off infections.
These bad cells build up in the bone marrow and other places. This stops normal blood making and causes leukemia symptoms.
Genetic mutations turn normal B-cell precursors into bad lymphoblasts. Knowing about these changes helps us find new treatments.
Genetic and Molecular Characteristics
B-ALL has complex genetics and molecules. Some genetic changes, like the Philadelphia chromosome, mean a worse outlook. But others might be better.
Genetic testing and molecular diagnostics are getting better. They help us understand B-ALL in each patient. This lets us make treatments that fit each person’s needs.
Epidemiology of B-ALL Leukemia: Who Is at Risk?
Age Distribution: Children vs. Adults
B-ALL is a big deal in kids, making up 80% of all leukemia cases in them. It mostly strikes between 2 and 5 years old. In adults, it’s less common, making up 20% of ALL cases. But it’s often tougher to treat in adults.
Knowing who gets B-ALL helps doctors plan better. Kids usually do better because they can handle strong treatments. Adults face tougher challenges because of their age and other health issues.
Genetic Risk Factors
Genetics is key in B-ALL. Some genetic conditions, like Down syndrome, raise the risk. Certain genetic changes, like the Philadelphia chromosome, are also important.
Scientists have found many genetic mutations that help B-ALL grow. These changes affect how B-cells develop. Knowing this helps doctors find new treatments.
Environmental Triggers and Associations
Not all causes of B-ALL are known, but some environmental factors might play a part. Ionizing radiation, for example, is linked to B-ALL. This is seen in people exposed to radiation from nuclear accidents or medical treatments.
Some chemicals and pesticides might also increase the risk. But more research is needed to confirm this. It’s important to understand how genes and environment interact to prevent B-ALL.
Recognizing B-ALL Symptoms: Early Warning Signs
It’s important to know the signs of B-Cell Acute Lymphoblastic Leukemia (B-ALL) for early treatment. B-ALL shows itself in different ways, affecting the body and immune system. Spotting these signs early can help get the right treatment fast.
Common Physical Symptoms
B-ALL can cause many physical symptoms. These happen because the disease affects the bone marrow and the immune system. Some common signs include:
- Pale skin due to anemia
- Easy bruising or bleeding
- Petechiae (small red spots on the skin)
- Fatigue or feeling weak
Systemic Manifestations
B-ALL also has systemic symptoms that affect overall health. These symptoms include:
- Fever, often recurrent
- Frequent infections due to a weakened immune system
- Loss of appetite and weight loss
- Swollen lymph nodes, liver, or spleen
These symptoms can really impact daily life. They need quick medical attention to manage the disease well.
When to Seek Medical Attention
Knowing when to see a doctor is key. If you or someone you know has several symptoms, it’s time to get help. Here are some signs to watch for:
| Symptom | Duration/Action |
| Persistent fatigue | Lasting more than 2 weeks |
| Unexplained fever | Recurring or lasting more than 3 days |
| Easy bruising/bleeding | Without apparent cause or injury |
| Frequent infections | More than usual or severe |
Getting B-ALL treated early can make a big difference. So, watch for these symptoms and seek medical help when needed.
Comprehensive Diagnostic Approach for B-Cell Lymphoblastic Leukemia
Diagnosing B-Cell Acute Lymphoblastic Leukemia (B-ALL) needs many steps. Getting the right diagnosis is key to choosing the best treatment. We will explain the main steps to find B-ALL.
Initial Blood Tests and Physical Examination
The first steps in diagnosing B-ALL include blood tests and a physical check-up. Blood tests look for abnormal white blood cells, which might mean leukemia. A complete blood count (CBC) is a very important first test. The physical check might show signs like swollen lymph nodes or a big spleen.
“Finding B-ALL early is very important,” say top hematologists. A good first check-up is the start of more tests.
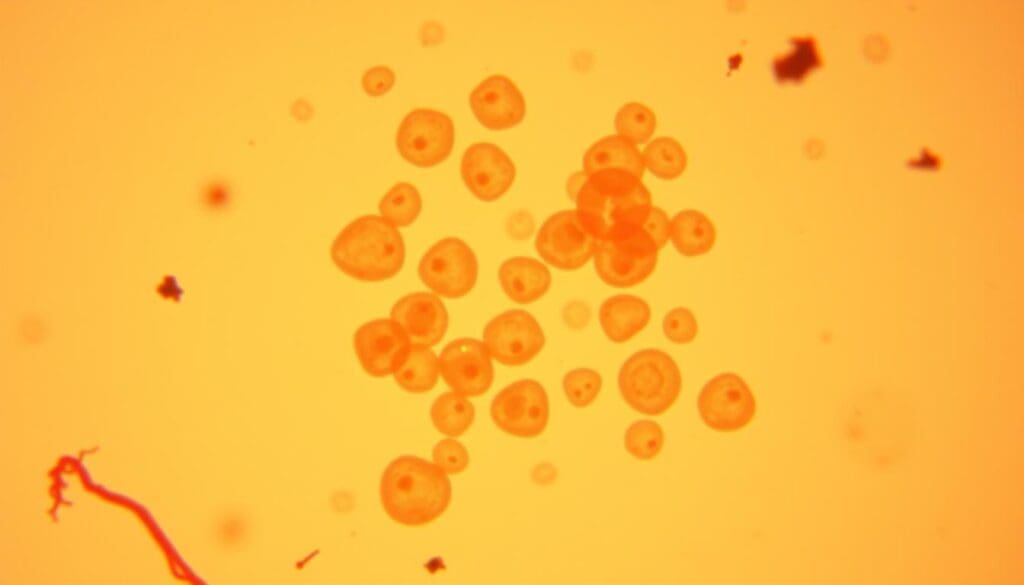
Bone Marrow Biopsy: Procedure and Findings
A bone marrow biopsy is a key test for B-ALL. It takes a bone marrow sample, usually from the hip, for a closer look. Finding lymphoblasts in the bone marrow is a big sign of B-ALL. This test shows how far the disease has spread and helps decide treatment.
Advanced Diagnostic Methods: Flow Cytometry and Genetic Testing
More advanced tests are also very important. Flow cytometry checks the leukemia cells. Genetic tests look for specific changes in the genes. These tests give important clues about the disease.
- Flow cytometry finds special markers on the cells.
- Genetic tests find genetic changes.
- These tests help tailor treatments.
Imaging Studies in B-ALL Evaluation
Imaging tests like X-rays, CT scans, or PET scans check how far the disease has spread. They help figure out the disease’s stage and how well treatment is working. These tests are key to managing the disease well.
In summary, finding B-ALL involves many steps. Using a detailed approach ensures the right diagnosis and the best treatment plan.
Modern Treatment Protocols for B-ALL Leukemia
The treatment for B-cell Acute Lymphoblastic Leukemia (B-ALL) has changed a lot in recent years. This brings new hope to patients and their families. We now understand the disease better and have more effective treatments.
Phase-Based Chemotherapy Approaches
Chemotherapy is key in treating B-ALL. It is given in different phases to work best and be safer. The phases are induction, consolidation, and maintenance.
In the induction phase, we try to get rid of all leukemia cells. The consolidation phase uses strong chemotherapy to kill more cancer cells. The maintenance phase helps keep the disease under control for a long time.
Targeted Therapies: Precision Medicine in B-ALL
Targeted therapies are also important in B-ALL treatment. They aim to kill cancer cells without harming healthy tissues. Tyrosine kinase inhibitors (TKIs) and monoclonal antibodies are examples. They help patients with certain genetic profiles.
Revolutionary CAR T-Cell Therapy
CAR T-cell therapy is a new and exciting way to treat B-ALL. It changes a patient’s T-cells to fight cancer. This therapy has shown great results in patients who have tried other treatments.
Stem Cell Transplantation: Indications and Process
Stem cell transplantation is an option for some B-ALL patients. It replaces the patient’s bad bone marrow with healthy stem cells from a donor. We decide if this is right for each patient based on their health and the disease.
By using these modern treatments, we can give better care to B-ALL patients. We make sure each patient gets the best treatment for them. This helps improve their outcomes and quality of life.
Monitoring Treatment Response: The Critical Role of MRD Testing
Monitoring how well a treatment works is key in B-ALL leukemia care. We use advanced tests to see if a patient is responding to treatment. Minimal Residual Disease (MRD) testing is a vital tool in this process.
Understanding Minimal Residual Disease
Minimal Residual Disease (MRD) means a small number of cancer cells left after treatment. MRD testing finds these cells. It shows if the treatment has killed the cancer or if some cells remain.
How MRD Testing Guides Clinical Decisions
MRD testing is essential for making treatment choices in B-ALL. It shows how well the treatment is working.
Latest Technologies in Disease Monitoring
New MRD testing methods have made monitoring more accurate. Flow cytometry and molecular diagnostics are used to spot MRD. These advances help us find cancer cells more precisely, guiding better treatment plans.
Prognosis and Success Rates: The Encouraging Outlook for B-ALL Patients
Medical treatments have greatly improved for B-Cell Acute Lymphoblastic Leukemia patients. This is true, even more so for kids, where cure rates have jumped up.
Pediatric Success Stories: 90% Cure Rates
Children with B-ALL are now seeing cure rates of up to 90%. This is thanks to better and more focused treatments. Early diagnosis and treatment are key to these high success rates.
Adult Prognosis Factors
Adults with B-ALL face a less hopeful outlook than kids. Yet, new treatments have also boosted adult outcomes. Important factors include age, health, and genetic markers. These help doctors create the best treatment plans for each patient.
Long-term Survival and Quality of Life
Surviving long-term and maintaining quality of life are now major goals. We’re working hard to reduce side effects and improve survivors’ well-being. This includes managing long-term issues and providing support services.
As we keep pushing forward in B-Cell Leukemia treatment, the future looks bright. With new research and therapies, we expect even better outcomes and quality of life for those with this disease.
Advanced Care Options: Multidisciplinary Approaches at Specialized Centers
At places like Liv Hospital, patients with B-ALL leukemia get top-notch care. These centers have the latest technology and teams of experts. They work together to give patients the best care possible.
The Importance of a Complete Care Team
A team of experts is key to B-ALL leukemia treatment. This team includes doctors, radiologists, and more. They all work together to make a treatment plan just for the patient.
This teamwork brings many benefits. It means better communication, more accurate diagnoses, and access to more treatments. It also helps manage side effects better.
Comprehensive care teams are vital for B-ALL patients. They make sure patients get the best care they can.
Liv Hospital’s Approach to B-ALL Treatment
Liv Hospital aims to give patients with B-ALL the best medical care. We use the latest research and guidelines to treat patients. This ensures they get the most effective treatments.
Liv Hospital’s team works with patients and their families. They create a treatment plan that fits each patient’s needs. This teamwork improves patient outcomes and quality of life.
International Treatment Protocols and Standards
Liv Hospital follows global standards for B-ALL leukemia treatment. We keep our protocols up to date with new research and technology. This ensures patients get the best care based on the latest knowledge.
By sticking to international treatment protocols, we offer patients the most effective treatments. Our focus on quality care shows in our patient results. It’s why we’re known as a top B-ALL treatment center.
Conclusion: Living with B-ALL and Future Directions in Treatment
As we wrap up our look at B-Cell Acute Lymphoblastic Leukemia (B-ALL), it’s clear that full care is key for better patient results. We’ve covered the details of B-ALL, from what it is and its medical terms to the newest treatments and tests.
New studies and better treatments are making life better for B-ALL patients. The focus is on treatments that target the disease and CAR T-Cell therapy. These steps show how vital it is to keep up with medical progress.
Places like Liv Hospital use a team approach to give patients the best care. They use the latest research and treatments to help B-ALL patients live well and fully.
Looking ahead, our dedication to top-notch healthcare and support for international patients won’t change. We’ll keep helping B-ALL patients, guiding them every step of the way.
FAQ
What is B-ALL leukemia?
B-ALL (B-cell Acute Lymphoblastic Leukemia) is a blood and bone marrow cancer. It happens when there are too many immature white blood cells, called lymphoblasts.
What are the symptoms of B-ALL leukemia?
Symptoms include feeling very tired, looking pale, and getting sick often. You might also bruise easily, have bone pain, swollen lymph nodes, and lose weight.
How is B-ALL leukemia diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests to find out if you have B-ALL. They also do imaging studies to see how far the disease has spread.
What is the treatment for B-ALL leukemia?
Treatment includes chemotherapy, targeted therapies, and sometimes CAR T-cell therapy. In some cases, a stem cell transplant is needed, based on how well you respond to treatment.
What is minimal residual disease (MRD) testing?
MRD testing looks for cancer cells left after treatment. It helps doctors decide on further treatment and check the risk of the cancer coming back.
What is the prognosis for B-ALL patients?
The outlook depends on your age, the disease’s genetics, and how well you respond to treatment. Kids often have a good chance of being cured, but adults face more challenges, including genetic factors.
What is CAR T-cell therapy?
CAR T-cell therapy is a new treatment. It changes your T-cells to fight cancer cells. It’s a hope for those with B-ALL that doesn’t respond to other treatments.
How does B-ALL affect bone marrow function?
B-ALL harms bone marrow by filling it with cancer cells. This reduces the production of healthy blood cells.
What are the genetic risk factors for B-ALL?
Some genetic changes, like the Philadelphia chromosome, can raise your risk of getting B-ALL. They can also affect how well you’ll do with treatment.
What is the role of a multidisciplinary care team in treating B-ALL?
A team of doctors, including hematologists and oncologists, works together. They provide the best care for B-ALL patients, aiming for the best results.
What is the significance of international treatment protocols in B-ALL care?
International protocols ensure patients get the same, proven treatments. This improves care and helps find new ways to fight B-ALL.
References:
- Inaba, H., & Mullighan, C. G. (2020). Pediatric acute lymphoblastic leukemia. Hematology/Oncology Clinics of North America, 34(6), 1001-1024. https://pubmed.ncbi.nlm.nih.gov/33020092/










