Last Updated on November 27, 2025 by Bilal Hasdemir

Finishing chemotherapy is a big win for cancer patients. It’s a sign of progress and the start of a new journey. At Liv Hospital, we know this is just the beginning of your recovery and adjustment.
Many patients wonder what comes next and how to recover well. We’re here to guide you through the recovery plan.
We’ll talk about the physical and emotional changes you might face. We’ll also cover follow-up care and long-term effects. Our aim is to offer full support and info to help you through this important time.
A study in BMC Cancer shows the right timing for starting therapy is key. Starting between 7 and 10 weeks after surgery doesn’t increase death risk.
Key Takeaways
- Recovery after chemotherapy involves physical and emotional adjustment.
- The next steps after chemotherapy may include surgery, radiation, or monitoring, depending on the cancer type.
- Timing is critical in starting adjuvant chemotherapy.
- Follow-up care is vital for managing long-term effects.
- Comprehensive support is available to help navigate the recovery period.
The Milestone of Your Final Chemo Treatment

The day of your last chemo session is here. It brings relief and uncertainty. Finishing chemotherapy is a big win, ending a tough treatment period. Understanding the emotional and physical sides of your final treatment is key.
The Emotional Impact of Completing Treatment
Finishing chemo can stir up many feelings. You might feel relieved it’s over but also worried about what’s next. It’s normal to feel this way, and having support is vital.
It’s okay to feel uncertain about what’s next. Your healthcare team is there to help. They can offer advice on managing your feelings and adjusting to life after chemo.
Physical Sensations During Your Last Session
In your final chemo session, you might feel numb or emotional. You could also face some physical side effects, but they might be milder than before.
Common physical sensations include:
- Fatigue
- Nausea
- Hair loss (if not already experienced)
- Changes in appetite
What to Bring and Who to Bring Along
For your last chemo session, bring someone for emotional support. It could be a family member, friend, or caregiver. Having them there can make the experience more special and help you deal with your feelings.
Items to bring along:
| Item | Purpose |
|---|---|
| Comfortable clothing | Enhance your comfort during the session |
| Snacks and water | Stay hydrated and energized |
| Books or entertainment | Pass the time during the session |
| Support person | Provide emotional support |
Immediate Post-Treatment Period: The First 72 Hours

After your last chemotherapy session, the next 72 hours are vital. They help you manage side effects and start your recovery. It’s important to know what to expect and have a plan to handle it.
Managing Side Effects That May Intensify
Some patients may feel side effects more intensely after their last treatment. These can include fatigue, nausea, and changes in blood counts. Having a support system, like family or friends, can help manage these effects.
Common side effects to watch for:
- Fatigue and weakness
- Nausea and vomiting
- Changes in appetite
- Increased risk of infection
Hydration and Nutrition Recommendations
Keeping hydrated and eating well is key during recovery. Drinking water and eating a balanced diet can help lessen side effects. We recommend drinking lots of water and eating foods rich in nutrients.
| Food Group | Recommended Foods | Benefits |
|---|---|---|
| Proteins | Lean meats, fish, eggs, dairy | Rebuilds tissues, supports immune function |
| Fruits and Vegetables | Berries, leafy greens, citrus fruits | Rich in antioxidants, vitamins, and minerals |
| Whole Grains | Brown rice, quinoa, whole wheat bread | Provides fiber, vitamins, and minerals |
When to Contact Your Healthcare Team
Knowing when to contact your healthcare team is important. If you have severe side effects, like trouble breathing or severe pain, call them right away.
Signs that require immediate medical attention:
- Fever above 100.4°F (38°C)
- Severe pain or difficulty breathing
- Signs of dehydration
- Severe nausea or vomiting
Being aware of what to expect and having a plan can make the first 72 hours easier. Remember, recovery takes time. Be patient and don’t hesitate to ask for help when you need it.
The First Month After Chemotherapy
The first month after chemotherapy is a key time for recovery and adjustment. It’s important to understand the changes your body goes through and how to manage them well.
Gradual Changes in Side Effects
In the first month, you might feel tired, nauseous, and experience hair loss. These side effects will lessen as your body heals.
Common side effects to watch for:
- Fatigue and weakness
- Nausea and changes in appetite
- Hair loss or changes in hair texture
- Changes in bowel habits
As these side effects fade, you’ll start to feel more like yourself. But, how quickly you recover can differ for everyone.
Energy Conservation Strategies
It’s key to save energy in the first month after chemotherapy. Your body is healing, and you need to pace yourself to avoid getting too tired.
Effective energy conservation tips:
- Prioritize tasks and focus on the most important ones
- Take regular breaks to rest
- Delegate tasks to family and friends when possible
- Engage in gentle exercises, like walking, to maintain strength
By managing your energy, you can make the most of your recovery time and avoid burnout.
Emotional Adjustments and Coping Mechanisms
The emotional journey after chemotherapy can be tough. You might feel a mix of emotions, from relief to anxiety about the future.
Coping mechanisms to consider:
- Mindfulness and meditation practices
- Support groups for sharing experiences and advice
- Counseling or therapy to address emotional concerns
- Engaging in hobbies and activities that bring joy
Using these coping mechanisms can help you deal with the emotional changes of recovery from chemotherapy.
Common Post Chemotherapy Effects and How to Manage Them
After chemotherapy, patients may face several common effects that can affect their recovery. It’s important to know about these effects and how to manage them. This knowledge is key to a successful recovery.
Fatigue and Energy Fluctuations
Fatigue is a big issue for many after chemotherapy, lasting months. Fatigue is not just feeling tired; it’s a deep exhaustion that can affect daily life and quality of life. To manage fatigue, pace activities, take breaks, and eat a healthy diet. For more tips, check out post-chemotherapy care resources.
Energy levels can also change a lot during the day. Keeping a diary to track energy can help plan activities. This way, you can do more when you have more energy.
Chemo Brain and Cognitive Changes
“Chemo brain” is a term for cognitive changes after chemotherapy, like memory issues and trouble focusing. The exact cause is not fully understood, but it’s believed to be related to the effects of chemotherapy on the brain. To manage chemo brain, try mentally stimulating activities, use memory aids, and stay active.
Neuropathy and Physical Discomfort
Neuropathy, or nerve damage, is a common side effect of chemotherapy. It can cause numbness, tingling, and pain in hands and feet. To manage neuropathy, try medications, physical therapy, and alternative therapies like acupuncture. Talk to your healthcare team about your symptoms to find the best treatment.
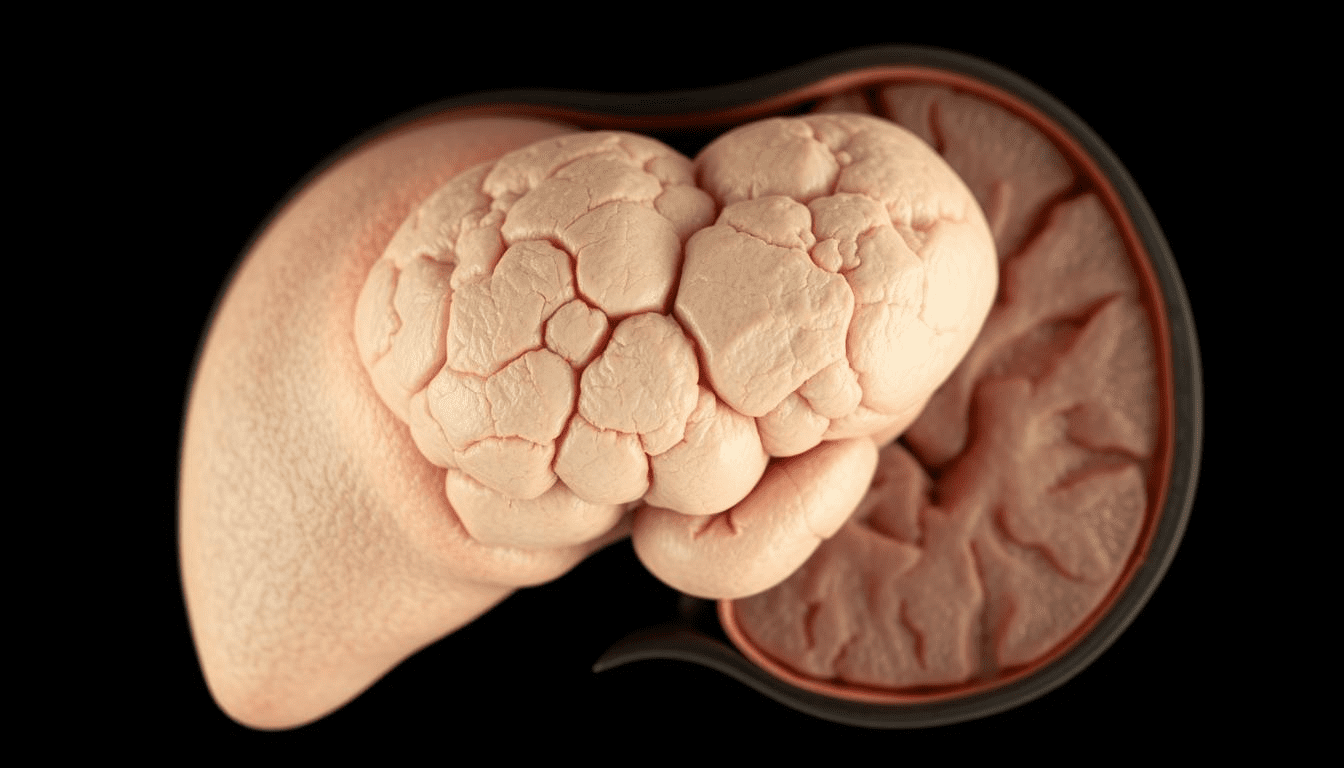
Immune System Recovery
Chemotherapy can weaken the immune system, making patients more prone to infections. Recovering immune function is a critical aspect of post-chemotherapy care. Support your immune system by practicing good hygiene, getting vaccinated, and living a healthy lifestyle. This includes eating well and exercising regularly.
By understanding and addressing these common post-chemotherapy effects, patients can better navigate their recovery journey and improve their overall well-being.
Chemotherapy Recovery Time: What to Expect
Chemotherapy recovery times vary a lot. It’s key to know what to expect. While it’s hard to say exactly how long it will take, studies give us some clues.
The Six-Month Recovery Milestone
Most people start feeling better around six months after treatment. This is a big step as the body heals and energy comes back. But, remember, getting better is slow, and some side effects can last longer.
During these six months, patients often face many physical and emotional changes. Fatigue, nerve issues, and brain fog are common. But, these usually get better with time.
Individual Factors Affecting Recovery Speed
Things like your health and the type of chemo you got can change how fast you recover. For example, those with health problems or more intense chemo might need more time.
Age, diet, and support also play big roles in recovery. Older people might take longer to get back on their feet. Eating well and having a strong support system can help a lot.
Setting Realistic Expectations
It’s important to have realistic hopes when going through chemo. Knowing recovery takes time can help you deal with feelings of disappointment. Talking openly with your doctors is also key to handling any issues that come up.
Being well-informed and ready can help you face the recovery journey. It’s a step towards getting your health and happiness back.
Follow-Up Care After Your Last Chemo Treatment
After finishing chemotherapy, the next step is follow-up care. This includes regular checks and support to make sure you’re recovering well. Follow-up care is key to your recovery, with regular visits and checks to keep an eye on your health.
Scheduling Your First Post-Treatment Appointment
It’s important to book your first post-treatment visit soon after finishing chemo. This visit lets your healthcare team check your health, address any immediate issues, and plan your follow-up care. You’ll get a full check-up, including a physical exam and possibly some tests to track your recovery.
Before your appointment, write down any questions or concerns you have. This could be about managing side effects, getting back to normal, or your follow-up care plan. You might also want to talk about your survivorship care plan with your doctor.
Recommended Testing and Monitoring Schedule
Your testing and monitoring schedule will be tailored to your cancer type, treatment, and health. It might include regular visits with your oncologist, imaging tests, and blood tests to check for tumor markers or other health signs.
| Test/Procedure | Frequency | Purpose |
|---|---|---|
| Oncologist Check-ups | Every 3-6 months initially | Monitor recovery, address concerns |
| Imaging Tests (CT, MRI) | As recommended by your doctor | Monitor for cancer recurrence |
| Blood Tests | Regularly scheduled | Monitor health indicators, tumor markers |
Creating a Survivorship Care Plan
A Survivorship Care Plan is a personal document that outlines your cancer diagnosis, treatment, and follow-up care. It’s a guide for you and your healthcare team to ensure you get the best care during recovery. The plan includes details about your cancer, treatments, possible late effects, and follow-up care recommendations.
Key components of a Survivorship Care Plan:
- Diagnosis and treatment summary
- Potential late effects of treatment
- Follow-up care schedule
- Recommendations for healthy living
- Contact information for your healthcare team
By following your Survivorship Care Plan, you can actively participate in your recovery. This ensures you get the care and support you need as you move forward.
What Is the Next Treatment After Chemotherapy?
Chemotherapy is often just one part of a treatment plan. Knowing what’s next can help you prepare. The next treatment depends on the cancer type, stage, and how well you responded to chemotherapy.
For many, treatment doesn’t end with chemotherapy. Knowing your options can make you feel more in control.
Surgery as a Follow-Up Option
In some cases, surgery is recommended after chemotherapy. It’s used to remove any remaining tumors or cancerous tissues. This is often the case when the cancer is localized and can be surgically removed.
Surgery can provide a definitive treatment by removing the visible tumor, potentially improving outcomes. Your surgical team will discuss the risks and benefits of the procedure, as well as what to expect during recovery.
Radiation Therapy Considerations
Radiation therapy may be suggested as a follow-up treatment. It targets any remaining cancer cells in a specific area. This is useful for cancers that are more likely to recur locally.
Radiation therapy can be delivered externally or internally, depending on the location and type of cancer. Your radiation oncologist will outline the treatment plan and possible side effects.
Targeted Therapies and Immunotherapies
Targeted therapies and immunotherapies are advanced treatment options after chemotherapy. These treatments target specific characteristics of cancer cells or enhance the body’s immune response against cancer.
Targeted therapies can be more precise, potentially reducing harm to healthy cells. Immunotherapies, on the other hand, can stimulate the immune system to recognize and attack cancer cells more effectively.
Maintenance Therapies for Certain Cancers
For certain types of cancer, maintenance therapies may be recommended after chemotherapy. These therapies help prevent recurrence. They can include medications that continue to target cancer cells or support the body’s recovery.
The decision to use maintenance therapy depends on your cancer’s characteristics and your overall health. Your healthcare team will discuss the benefits and risks.
Nutrition and Exercise During Recovery After Chemotherapy
Recovering from chemotherapy involves nutrition and exercise. These are key to rebuilding strength and health. Understanding their role is vital for our well-being.
Eating right is essential for healing. A diet full of fruits, veggies, whole grains, and lean proteins helps. It manages side effects and boosts energy.
Dietary Recommendations for Rebuilding Strength
To regain strength, focus on nutrient-rich foods. Include:
- Lean proteins like chicken, fish, and legumes
- Whole grains such as brown rice, quinoa, and whole-wheat bread
- A variety of colorful fruits and vegetables
- Healthy fats found in nuts, seeds, and avocados
Safe Exercise Progression Plans
Exercise is vital for recovery. It boosts physical and mental health. Start with gentle activities like walking or yoga. Then, increase intensity as you get stronger.
Working with a physical therapist is helpful. They can create a plan that fits your needs and abilities.
Working with Nutritionists and Physical Therapists
Team up with nutritionists and physical therapists for personalized help. They craft plans that meet your nutritional and physical needs. This ensures a better recovery.
By combining good nutrition and exercise, we can improve our health and well-being.
Emotional and Psychological Recovery
Finishing chemotherapy doesn’t mean you’re done recovering. Your emotional and psychological health needs care too. Healing after treatment is about more than just getting better physically.
Post-Treatment Depression and Anxiety
Feeling down or anxious after treatment is normal. These feelings can come from relief, fear, or adjusting to a new life. Recognizing these emotions is the first step towards healing.
If these feelings last, get professional help. Counseling and therapy can help you manage your emotions better.
Fear of Recurrence Management
Many worry about cancer coming back after treatment. Regular check-ups, support groups, and mindfulness can help manage this fear.
Mindfulness practices, such as meditation and deep breathing, can help reduce anxiety and fear, helping you focus on recovery.
Support Groups and Counseling Resources
Support groups and counseling are key for emotional recovery. They offer a place to share, get support, and learn from others facing similar challenges.
Studies show these resources are vital for emotional challenges during recovery. We suggest exploring them as part of your recovery plan.
Redefining Your “New Normal”
After treatment, finding your “new normal” is important. This means adjusting to physical and emotional changes and finding joy in life again.
Creating a survivorship care plan can guide you through this new chapter. It should include regular check-ups, lifestyle changes, and managing long-term effects.
| Strategies for Emotional Recovery | Description | Benefits |
|---|---|---|
| Mindfulness and Relaxation | Practices such as meditation and deep breathing | Reduces anxiety and fear, improves mental well-being |
| Support Groups | Sharing experiences and receiving support from others | Provides emotional support, reduces feelings of isolation |
| Counseling and Therapy | Professional help to manage emotions and adjust to new reality | Helps manage depression and anxiety, improves coping mechanisms |
Returning to Work and Daily Activities
After chemotherapy, the next big step is going back to work and doing daily things. This helps you feel normal again and boosts your well-being.
Timing Your Return to Work
Figuring out when to go back to work is tough. You need to think about how your body and mind are doing. Talking to your healthcare team can help figure out the best time based on your recovery.
Some people might do better with a slow return to work. Starting with part-time hours or easier tasks can help your body get used to work again.
Workplace Accommodations to Consider
When you go back to work, you might need some special help. This could be things like flexible hours, a comfy workspace, or easier tasks. These changes can make your transition smoother.
- Flexible working hours to manage fatigue
- Ergonomic workspace adjustments for comfort
- Temporary job modifications to reduce physical strain
The Americans with Disabilities Act (ADA) says employers must make reasonable changes for people with disabilities. This includes those who have had cancer treatment.
Gradually Resuming Social Activities
Going back to social events is a big part of getting back to life. It’s best to start with small, easy gatherings. Then, you can do more and bigger things as you get more energy.
Keeping in touch with friends and family is great for your mind and heart. But, don’t forget to rest too. Too much can make you tired.
Communicating Your Needs to Others
Telling others about what you need is very important. Being clear about your limits helps your boss, coworkers, and friends know how to support you.
“Open and honest communication about your needs and boundaries is key for a supportive environment during your recovery.”
By talking about what you need, you can make your work and social life more supportive. This helps you recover and get back to normal faster.
Long-Term Effects to Monitor Years After Treatment
After chemotherapy, it’s important to know about long-term effects on your health. Some side effects may last a long time or even show up later. Knowing about these effects helps keep you healthy after treatment.
Potential Organ-Specific Concerns
Some chemotherapy drugs can harm specific organs. For example, some may hurt your heart, leading to problems like heart failure. Others might affect your kidneys or lungs. Regular check-ups and screenings are key to watching these organs.
Organ-specific concerns can include:
- Cardiac issues due to certain anthracyclines
- Respiratory problems from drugs like bleomycin
- Nephrotoxicity affecting kidney function
- Ototoxicity leading to hearing loss
Secondary Cancer Risks
One big worry is the chance of getting secondary cancers. Some chemotherapy can damage DNA, which might cause new cancers. The risk depends on the type of chemotherapy, how much you got, and your health.
Talking to your doctor about your risk is very important.
| Chemotherapy Type | Secondary Cancer Risk | Monitoring Recommendations |
|---|---|---|
| Alkylating agents | Higher risk of myelodysplastic syndrome and acute myeloid leukemia | Regular blood counts, bone marrow biopsies as needed |
| Topoisomerase II inhibitors | Increased risk of acute myeloid leukemia | Periodic blood counts, monitoring for signs of leukemia |
Fertility and Hormonal Considerations
Chemotherapy can affect your fertility and hormones. How much it affects you depends on your age, the type of chemotherapy, and how much you got. If you’re worried about fertility, talking about freezing eggs or sperm before treatment is a good idea.
Hormonal changes can also happen, leading to early menopause or other hormone problems. Regular checks can help manage these issues.
Recommended Screening Guidelines
Following screening guidelines is key to watching for long-term effects. This might include regular imaging, blood tests, and physical exams based on your treatment and risk factors.
Screening guidelines may recommend:
- Annual echocardiograms for those at risk of cardiac issues
- Regular mammograms and other cancer screenings
- Periodic assessment of thyroid function
- Monitoring for signs of neuropathy or other neurological effects
By staying informed and following these guidelines, you can manage your health better after chemotherapy.
Conclusion: Embracing Life Beyond Chemotherapy
Finishing chemotherapy is a big step, starting a new chapter in your life. As you move into life after chemotherapy, focus on support and self-care. We’ve looked at how to manage side effects and get stronger through food and exercise.
Life after chemotherapy means finding a new normal and thriving. Cancer survivor stories show the power of staying strong and having support. By taking care of your body and mind, you can find your strength again and move forward with confidence.
Remember, your recovery journey is unique. It’s about healing, rebuilding, and finding yourself again. We’re here to support you, providing care and guidance to help you adjust to your new life.
FAQ
What happens after my final chemotherapy treatment?
After your last chemotherapy session, you start a new recovery phase. You might feel different physically and emotionally. It’s key to have a plan for managing side effects and follow-up care.
How long does it take to recover from chemotherapy?
Recovery time from chemotherapy varies. It depends on the treatment type, your health, and the cancer type. Generally, it takes several months to a year or more to fully recover.
What are the common post-chemotherapy effects, and how can I manage them?
Common effects include fatigue, energy changes, and cognitive issues. You might also experience neuropathy and immune system suppression. To manage these, try self-care, lifestyle changes, and medical support like nutrition counseling and physical therapy.
What should I expect during my first post-treatment appointment?
At your first post-treatment visit, your healthcare team will check your health. They’ll discuss any concerns and plan your follow-up care. This includes testing and monitoring schedules.
What are the next steps after chemotherapy, and how do I determine the best course of treatment?
Next steps depend on your cancer type, treatment goals, and health. Your team will discuss options like surgery, radiation, and targeted therapies. They’ll help choose the best treatment for you.
How can I manage my energy levels and cope with emotional adjustments after chemotherapy?
To manage energy and emotions, pace yourself and conserve energy. Seek support from loved ones and mental health professionals. Prioritize self-care and practice relaxation techniques.
What dietary recommendations can help me rebuild strength after chemotherapy?
Eat a balanced diet with protein, complex carbs, and healthy fats to rebuild strength. Stay hydrated and consider a personalized meal plan with a nutritionist.
How can I safely resume exercise after chemotherapy, and what are the benefits?
Start exercising slowly and with your healthcare team’s guidance. Exercise can improve physical function, reduce fatigue, and boost well-being. Begin with low-intensity activities and gradually increase.
What are the possible long-term effects of chemotherapy, and how can I monitor them?
Chemotherapy can lead to organ issues, secondary cancer risks, and fertility concerns. Your team will outline screening guidelines and monitoring schedules to keep you informed.
How can I cope with the fear of recurrence, and what resources are available?
To cope with recurrence fear, seek support from loved ones and mental health professionals. Prioritize self-care and engage in stress-reducing activities. Your healthcare team can offer guidance and resources.
When can I return to work and daily activities after chemotherapy?
Returning to work and daily activities depends on your recovery, job needs, and health. Discuss your plans with your healthcare team and employer for a smooth transition.
What kind of support is available for managing post-treatment depression and anxiety?
Support includes counseling, support groups, and mental health professionals. Your healthcare team can provide guidance and referrals to access these resources.
How can I create a survivorship care plan, and what does it entail?
A survivorship care plan outlines your follow-up care and strategies for managing long-term effects. Your healthcare team will help create a plan tailored to your needs.