Last Updated on November 27, 2025 by Bilal Hasdemir
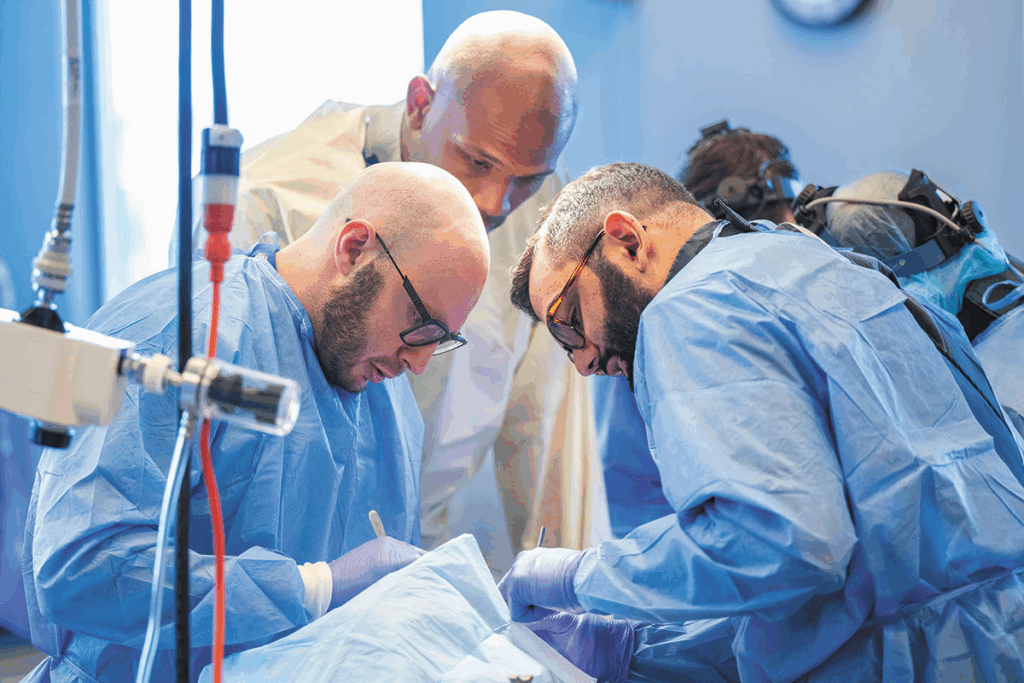
Spine surgery is a big deal and usually a last choice for spinal problems. Nearly 500,000 spine surgeries are done every year in the United States. Many of these surgeries lead to complications.
“We want to help patients make smart choices about their health. Thinking about spine surgery can be scary. It’s important to know the risks and the reasons to avoid spine surgery, and whether they outweigh the benefits.
It’s key to understand the risks of spine surgery to make good choices about your spine. We aim to give you a fair view. This helps you think about other treatments before surgery.
Knowing why spine surgery is suggested can help patients choose the right treatment. It’s a big step that comes after trying other options.
Doctors recommend surgery for serious pain or nerve problems. They look at other treatments first. Then, they weigh the surgery’s benefits and risks.
Some spinal issues might need surgery. These include:
These problems can really affect a person’s life. Surgery might be an option if other treatments don’t work.
Spine surgery has changed a lot, thanks to new tech and methods. Old open surgeries are now mostly replaced by minimally invasive procedures. These new methods aim to cut down on recovery time and damage.
The changes include:
These updates have helped many patients. But, it’s important to remember that each case is different. And, there’s always a chance of complications.

When thinking about spine surgery, it’s key to know the risks and benefits. This surgery can greatly change a patient’s life.
The decision to have spine surgery is big.Patients need to know the risks and benefits well to make a smart choice.
Research shows that spine surgery results can vary a lot. For example, a study in the Journal of Neurosurgery: Spine found 50% to 60% of patients see big improvements for some spinal issues.
But, the same study found many patients don’t see as much improvement or face complications. This shows why it’s vital to look at each case carefully.
Each spinal problem has its own risks and benefits with surgery. For instance, surgery for herniated discs or spinal stenosis might help some, but it also has risks like infection or nerve damage.
For degenerative disc disease, surgery might be considered if other treatments don’t work. But, the decision must consider the patient’s age, health, and the condition’s details.
Elderly patients face higher risks with spine surgery because of health issues or less ability to heal. Surgical problems in older patients can be serious. It’s important to think carefully about these risks and benefits.
In summary, while spine surgery might help some, it’s not without risks. Knowing these risks and benefits well is key for making good choices.
For some, spine surgery doesn’t bring the relief they hoped for. Instead, it leads to Failed Back Surgery Syndrome (FBSS). This condition causes ongoing or returning pain after surgery, greatly affecting a patient’s life quality.
Failed Back Surgery Syndrome is when patients keep feeling pain or symptoms after spine surgery. It’s not because the surgeon failed, but because of many factors. These include the initial problem, the surgery type, and the patient’s health.
FBSS can happen for many reasons. It might be due to poor surgery technique, not fully fixing the problem, or new issues from the surgery. Knowing these reasons helps surgeons and patients make better choices.
Research shows that spine surgery failure rates vary. For example, up to 40% of patients with lumbar spine surgery might face persistent pain or FBSS.
These numbers highlight the need to think carefully about spine surgery. It’s important to consider other treatments before deciding on surgery.
Failed back surgery can have lasting effects. It can cause chronic pain, reduced mobility, and affect mental health. Patients might feel depressed, anxious, and have a lower quality of life due to pain and limited movement.
The economic costs of FBSS are also high. They include extra medical bills, rehabilitation, and lost work time. So, it’s key to think about these long-term effects when choosing spinal treatment.
Spine surgery carries a big risk of nerve damage. This can greatly affect a patient’s life quality. The surgery involves working with delicate areas around the spinal cord and nerves. This increases the chance of injury to these important parts.
Nerve injuries during spine surgery can vary in severity and type. Some common types include:
Neurological complications from nerve damage during spine surgery can greatly affect a patient’s life. These complications may include chronic pain, muscle weakness, numbness, or tingling sensations. In severe cases, patients may experience paralysis or loss of bladder and bowel control. This can drastically change their daily lives and independence.
The impact on quality of life is not just physical; neurological complications can also lead to emotional and psychological distress. Patients may experience depression, anxiety, or frustration due to their changed circumstances. This highlights the need for care that addresses both physical and emotional needs.
We must carefully consider these risks when deciding on spine surgery. We need to weigh the possible benefits against the possible neurological complications. Understanding the types of nerve injuries and their long-term effects is key for making informed decisions about spinal health.
Infections and complications after spine surgery are serious. Patients need to know about these risks. Spine surgery can help many spinal conditions, but it comes with dangers.
Surgical site infections (SSIs) are common after spine surgery. These can be skin infections or deeper ones in the vertebrae or discs. It’s important to treat SSIs quickly to avoid more problems.
Studies show SSIs rates vary. This depends on the surgery type, patient health, and how the surgery is done. Keeping the surgery area clean and following care instructions can lower infection risk.
Spine surgery often uses rods, screws, and cages to support the spine. These implants help during healing but can fail. Failure might need more surgery, increasing risk and recovery time.
“The use of instrumentation in spine surgery has become more common, but it also introduces additional risks, including hardware failure and infection.”
Spine surgery can also cause problems that affect the whole body. These include DVT, pulmonary embolism, and heart issues. People with health problems before surgery are at higher risk. This highlights the need for a detailed check before surgery.
Knowing these risks is key for those thinking about spine surgery. Being informed helps patients make better choices. It also helps them work with doctors to avoid complications.
Many patients face chronic pain after spine surgery, even when they hope for relief. Spine surgery aims to ease back pain, but some patients find their pain doesn’t go away or even gets worse.
It’s important to understand why this happens. This knowledge helps manage expectations and look for other ways to treat pain. We’ll explore the reasons behind this issue and the hurdles in managing pain after surgery.
Several reasons can cause pain to stay or get worse after spine surgery. These include:
These factors show how complex spinal conditions are and how hard surgery can be to fix them.
Dealing with chronic pain after spine surgery is tough. Patients need a mix of treatments to find relief.
| Treatment Approach | Description | Potential Benefits |
| Pain Management Medications | Use of pharmaceuticals to control pain | Reduced pain levels, improved quality of life |
| Physical Therapy | Targeted exercises to improve mobility and strength | Enhanced functional ability, reduced pain |
| Alternative Therapies | Includes acupuncture, chiropractic care, and other non-pharmacological interventions | Potential for pain reduction, improved well-being |
By knowing why chronic pain happens after spine surgery and trying different treatments, patients and doctors can improve life quality together.
Recovering from spine surgery is a long and tough journey. It involves both physical and emotional challenges. It’s important for patients to know what to expect during this time.
The time it takes to recover from spine surgery varies. A simple discectomy might need less time than a complex spinal fusion surgery.
| Procedure | Typical Recovery Time | Key Activities During Recovery |
| Discectomy | 2-6 weeks | Light walking, gradual return to daily activities |
| Spinal Fusion | 3-6 months | Physical therapy, avoiding heavy lifting, bending |
| Laminectomy | 4-8 weeks | Rest, physical therapy, improving mobility |
Recovering from spine surgery is not just about physical healing. It also requires emotional strength. Patients often face pain, discomfort, and frustration.
Physical Therapy is key in the recovery process. It helps patients regain strength, improve mobility, and reduce pain. A good physical therapy plan can greatly improve surgery results.
Support from family, friends, and healthcare professionals is vital. Patients should share their feelings and concerns. They should also seek help when needed.
Spinal fusion aims to stabilize the spine but can lead to mobility problems. It’s meant to ease pain and stabilize the spine. Yet, it can cause complications that impact daily life. We’ll look at the long-term effects of spinal fusion, focusing on adjacent segment disease and its impact on daily activities.
Adjacent segment disease (ASD) is a major complication of spinal fusion. It happens when the segments next to the fusion site bear more stress, leading to faster wear and tear. This can cause new or worsening pain, possibly needing more surgery.
The risk factors for ASD include:
Accelerated degeneration can cause a series of problems, like herniated discs, spinal stenosis, and facet joint arthritis. It’s important for those thinking about spinal fusion to know these risks.
Spinal fusion surgery can greatly reduce a patient’s range of motion. By joining vertebrae, it limits flexibility in the spine. This can make everyday tasks harder, like bending, twisting, or lifting.
Some common issues patients face include:
It’s key for patients to talk to their healthcare provider about these possible limitations. This way, they can understand how spinal fusion might change their lifestyle and plan for it.
Knowing the true cost of spine surgery is key to making smart healthcare choices. Spine surgery is complex and often needed for many spinal issues. It comes with a big financial cost. This cost includes not just the surgery itself but also long-term care and possible complications.
The direct costs of spine surgery include hospital fees, surgeon charges, and anesthesia. These costs can range from $50,000 to over $150,000. This depends on the surgery’s complexity and the patient’s health.
Insurance coverage is important in reducing these costs. But, how much coverage you get varies a lot. It’s important to know what your insurance covers, including deductibles and co-pays.
There are hidden costs to spine surgery too. Recovery often involves physical therapy and may need more surgeries or long-term care. These costs can add up fast, making things harder financially for patients.
Another hidden cost is lost income from time off work. Recovery can take months, leaving patients without a paycheck. This can be hard to get back.
| Cost Category | Average Cost | Notes |
| Hospital Charges | $30,000 – $100,000 | Varied based on length of stay and services |
| Surgeon Fees | $5,000 – $20,000 | Dependent on surgeon’s experience and location |
| Rehabilitation Costs | $2,000 – $10,000 | Physical therapy and other recovery expenses |
| Lost Income | Varies | Dependent on patient’s salary and recovery time |
It’s important to understand these costs to make informed decisions. By looking at both direct and hidden costs, patients can better prepare for the financial side of spine surgery.
Spine surgery’s psychological impact is a big deal for both patients and doctors. It can change a person’s mental health and life quality a lot.
Research shows spine surgery patients face a higher risk of depression and anxiety. The stress and doubt about surgery outcomes can make these problems worse.
Recovering from surgery is not just about the body. It’s also about the mind. Patients might feel scared, anxious, frustrated, or disappointed.
Spine surgery affects family and social life too. The recovery is long and hard, needing help from family and friends.
But, the support can get tough. This is because the patient’s mood or behavior might change because of their condition or the surgery.
| Aspect | Pre-Surgery | Post-Surgery |
| Emotional State | Anxious, hopeful | Relieved, sometimes depressed |
| Family Support | High | Variable, sometimes strained |
| Social Activities | Limited due to pain | Gradually increasing |
It’s key to understand these impacts for full care. By knowing the mental and social challenges of spine surgery, doctors can help patients more.
People in high-risk groups, like older adults and athletes, face big challenges with spine surgery. They need special care and treatment plans that fit their needs.
Elderly people have a higher risk of problems during spine surgery. This is because of health issues, less energy, and taking many medicines. They are at risk for infections, heart problems, and longer recovery times.
Doctors should do detailed checks before surgery to lower these risks. Improving nutrition, managing health problems, and cutting down on medicines can help. Personalized care plans that consider the patient’s health and lifestyle are key.
Athletes and active people have their own set of challenges with spine surgery. They worry about how it will affect their career and lifestyle. They want to know when they can get back to their sport and if they’ll be as good as before.
Choosing to have surgery is a big decision for athletes. They must think about the benefits and risks. Rehab programs that match their sport can help them get back to their game.
It’s important to understand the effects of spine surgery on high-risk groups. This way, doctors can give better support and advice.
Getting a correct diagnosis is key to avoiding unnecessary surgeries in spinal health. If a diagnosis is wrong, it can lead to treatments that don’t fix the real problem. This includes surgeries that might not solve the patient’s symptoms.
Diagnosing spinal conditions can be tricky. Imaging like MRI or CT scans might not always show what’s wrong. This can cause doctors to guess wrong if they focus too much on the scans and not enough on the patient’s overall health.
It’s not always easy to match what scans show with what patients feel. Some people might have big problems on scans but feel fine. Others might be in a lot of pain but scans show little. This shows how important it is to link what scans show with how patients feel and act.
Getting advice from several doctors before spine surgery is wise. It lets patients hear different views on their condition and what treatment might work best.
By being thorough and careful in diagnosis and treatment planning, patients can lower the chance of wrong diagnoses leading to unnecessary surgery.
Back pain doesn’t have to mean surgery. There are many non-surgical treatments that work well. Many people find relief without the risks of surgery.
Physical therapy is key for back pain. It includes exercises to strengthen muscles, improve flexibility, and posture. Therapists also use heat, cold, and electrical stimulation to lessen pain and swelling.
Benefits of Physical Therapy:
Pain management is vital for treating back pain without surgery. This includes medication, injections, and other methods to reduce pain and improve life quality.
| Pain Management Strategy | Description | Benefits |
| Medication | Use of analgesics and anti-inflammatory drugs | Reduces pain and inflammation |
| Injections | Corticosteroid injections to reduce inflammation | Provides targeted relief |
| Nerve Blocks | Blocking pain signals to the brain | Effective for severe pain |
Changing your lifestyle can help a lot with back pain. This includes better ergonomics at work and home, staying healthy, and exercising regularly.
Ergonomic Tips:
By trying these non-surgical options, you can manage your back pain well. This improves your life quality a lot.
Back pain relief can often be found through non-invasive, evidence-based treatments. Surgery should be a last choice. So, it’s key to explore these alternatives first.
Conservative treatments include many therapies and interventions. They help reduce pain and improve function and quality of life. This makes them a great first step for many patients.
Non-invasive treatments have strong evidence supporting their effectiveness. Physical therapy is a key part of these treatments. It focuses on exercises to strengthen the back, improve flexibility, and posture.
Pain management strategies, like medication and injections, also play a big role. They provide relief when used carefully.
Other effective treatments include:
Complementary and alternative medicine (CAM) offers more options for back pain relief. These include:
By combining these treatments in a care plan, patients can see big improvements. They can feel better and live better lives.
Deciding on spine surgery needs careful thought. You must understand the surgery, its results, and other treatment options. This is key during your pre-surgery talk.
It’s important to ask the right questions to your surgeon. This ensures you’re well-informed. Here are some key ones:
These questions help you grasp the surgeon’s view. They aid in making a better choice.
| Question | Purpose | Example |
| Expected Outcomes | Understand the surgery’s goals | “How will this surgery improve my condition?” |
| Potential Risks | Know possible complications | “What are the most common complications associated with this surgery?” |
| Alternative Treatments | Look into non-surgical options | “Are there any non-surgical treatments that could be as effective?” |
While most surgeons give good advice, some red flags exist. Be cautious of:
Knowing these red flags helps you make a better choice. It’s wise to seek a second opinion if needed.
It’s very important for patients to make smart choices about their spine health before surgery. We’ve looked at the good and bad sides of spine surgery. This helps patients take charge of their health.
Knowing the possible problems and long-term effects of surgery is key. Patients can then choose what’s best for them. Options like physical therapy and pain management are good alternatives to surgery.
Being in control of your spine health is the goal. We urge patients to ask questions and get different opinions. This way, they can make choices that improve their life.
Spine surgery can lead to nerve damage and infection. It may also cause chronic pain. There’s also a risk of complications from spinal fusion, like disease in other segments. Knowing these risks helps in making informed choices.
Failed Back Surgery Syndrome (FBSS) is when pain persists after surgery. The exact rate of FBSS varies. But it’s a big concern, showing the importance of thinking carefully before surgery.
Yes, there are many non-surgical ways to manage back pain. These include physical therapy and lifestyle changes. They can be very effective and should be considered first.
Recovery from spine surgery can take a long time. It depends on the surgery type. Recovery times range from weeks to months. Patients face physical and emotional challenges during this time.
Spine surgery comes with financial costs. This includes direct medical expenses and insurance issues. There are also hidden costs like rehabilitation and lost income. Understanding these costs is key for making informed decisions.
Yes, spinal fusion can cause long-term mobility problems. This includes disease in other segments and faster degeneration. It can affect patients’ movement and daily activities.
Misdiagnosis can cause unnecessary surgery. This happens when symptoms don’t match images or when diagnosis is incomplete. Getting multiple opinions is important to avoid unnecessary surgery.
Spine surgery can deeply affect patients’ mental health. It can lead to depression and anxiety. It also impacts family and social relationships.
Yes, elderly patients face more risks with spine surgery. It’s important to weigh the benefits and risks carefully. Their overall health and recovery chances need to be considered.
Before spine surgery, ask your surgeon about risks and benefits. Also, ask about other treatments and recovery expectations. Knowing red flags in surgical advice is also important.
Conservative treatments, like non-invasive options and alternative medicine, can be very effective. They offer choices beyond surgery. They can help manage back pain well.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!