Last Updated on November 26, 2025 by Bilal Hasdemir

Getting a diagnosis of non-small cell lung cancer (NSCLC) can feel scary. But, new treatments offer hope to patients and their families. At Liv Hospital, we focus on you, guiding you through the best treatments for your situation.
We offer lung cancer treatment that’s just for you. We use the latest drugs and immunotherapy to help you beat cancer for good. We look at your cancer’s stage and type to make the right plan for you.
Our goal is to make your life better with the latest lung cancer treatment. Our team is dedicated to top-notch care for everyone, including international patients.
Key Takeaways
- Personalized treatment plans for NSCLC patients
- Advanced therapies like targeted drugs and immunotherapy
- Comprehensive evaluation of patient condition
- Focus on achieving long-term remission
- World-class healthcare for international patients
Understanding Non-Small Cell Lung Cancer (NSCLC)

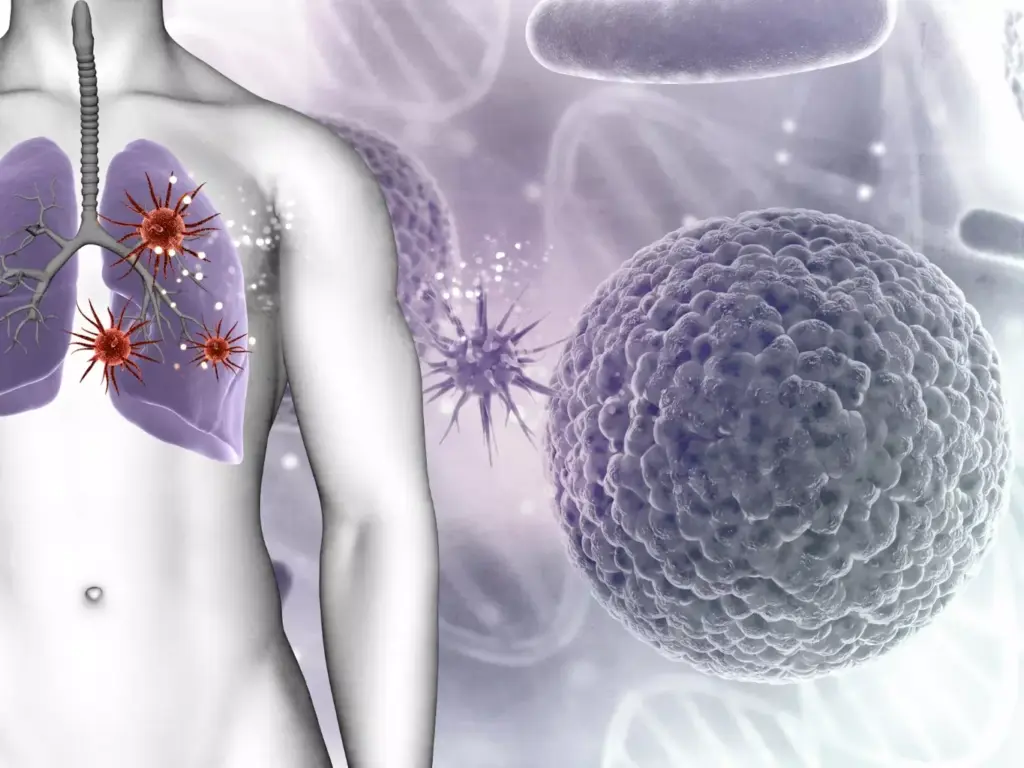
It’s key for patients to understand NSCLC to make sense of their diagnosis and treatment choices. NSCLC makes up about 85% of lung cancer cases. This makes it the most common lung cancer type.
Types and Prevalence of NSCLC
NSCLC includes several types, like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Each type has its own traits and might need different treatments.
Recent studies show how genetic testing is vital in NSCLC. It helps doctors find targeted therapies that work better for patients. Adenocarcinoma is the most common type, often found in non-smokers.
Staging and Its Impact on Treatment Selection
Staging NSCLC is key to figuring out how far the disease has spread. It’s important for picking the right treatment. We use CT scans, PET scans, and molecular tests to stage NSCLC accurately.
“Accurate staging is the cornerstone of effective NSCLC management, guiding treatment decisions that can significantly impact patient outcomes.”
Staging tells us if the cancer is just in one place or has spread. Knowing this helps us choose the best treatment. It could be surgery, radiation, chemotherapy, or a mix of these.
Treatment Option 1: Surgical Resection
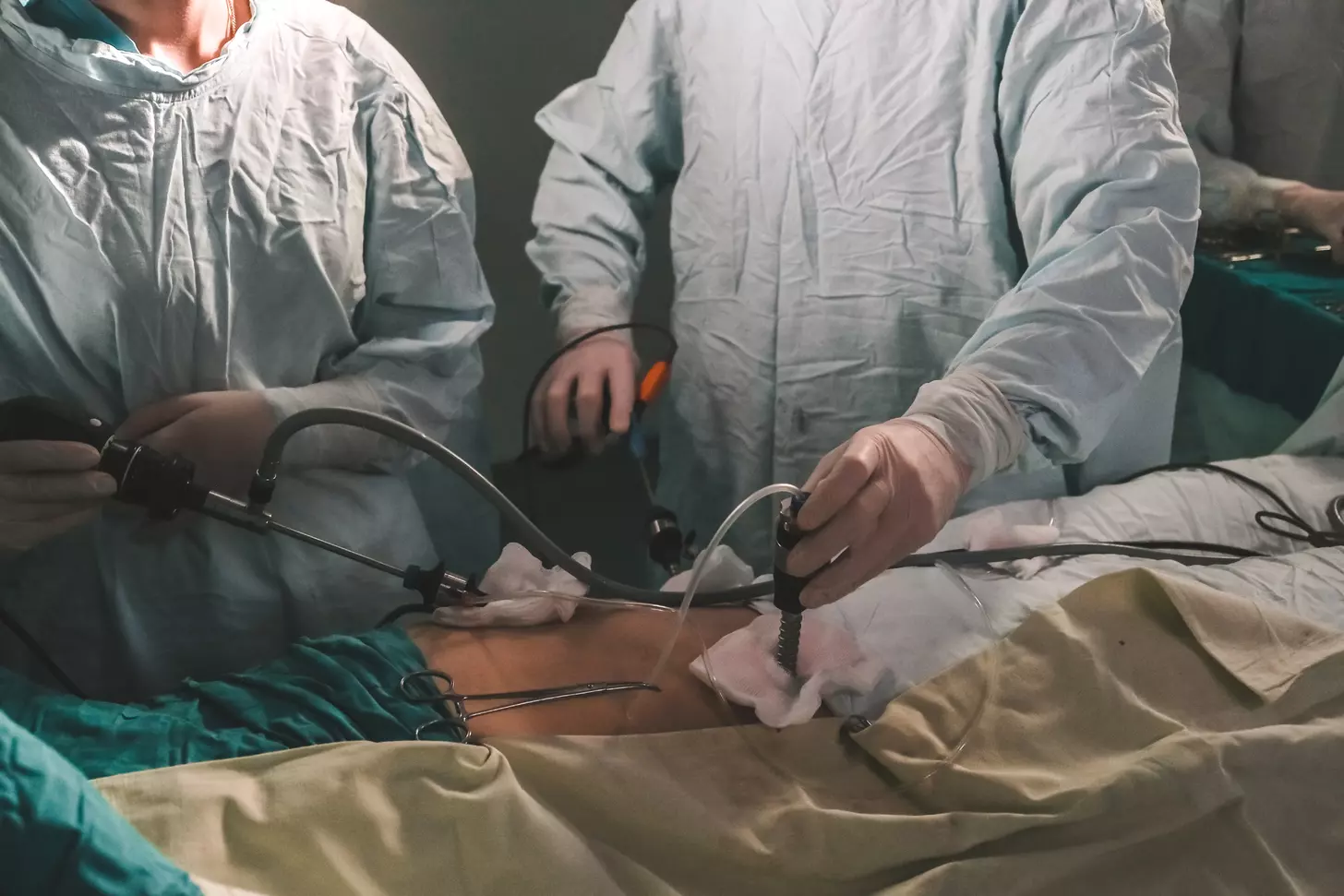
Surgical resection is a main treatment for Non-Small Cell Lung Cancer (NSCLC). It can be a cure for early-stage patients. We use the latest surgical methods to treat NSCLC patients effectively.
Thanks to new surgical techniques, like minimally invasive surgery, NSCLC patients are doing better. Our team focuses on personalized care. We tailor treatments to meet each patient’s needs.
Types of Surgical Procedures
We perform different surgeries for NSCLC, like lobectomy, segmentectomy, and wedge resection. The right surgery depends on the tumor’s size and location, and the patient’s health.
- Lobectomy: This involves removing a whole lobe of the lung. It’s often chosen for bigger tumors or those in one lobe.
- Segmentectomy: This surgery removes a lung segment. It’s for smaller tumors or when lung function is limited.
- Wedge Resection: This is for small, peripheral tumors. It removes a small, wedge-shaped lung section.
| Surgical Procedure | Description | Typical Indication |
|---|---|---|
| Lobectomy | Removal of an entire lobe | Larger tumors within a single lobe |
| Segmentectomy | Removal of a lung segment | Smaller tumors or limited lung function |
| Wedge Resection | Removal of a small, wedge-shaped section | Small, peripheral tumors |
Minimally Invasive Surgical Techniques
We use video-assisted thoracoscopic surgery (VATS) and robotic-assisted thoracic surgery (RATS) for less invasive surgeries. These methods have smaller incisions, less tissue damage, and less pain than open surgery.
These advanced techniques help improve patient outcomes and quality of life for those with NSCLC.
Treatment Option 2: Radiation Therapy
We use radiation therapy as a key treatment for NSCLC. We use advanced methods to target tumors well. This treatment is a non-surgical way to manage the disease.
Our radiation oncology team works hard to give the right amount of radiation to the tumor. They do this while keeping healthy tissues safe. New methods like Stereotactic Body Radiation Therapy (SBRT) are helping a lot, even for those who can’t have surgery.
External Beam Radiation Therapy
External Beam Radiation Therapy (EBRT) uses beams from outside the body to hit the tumor. It’s very good at treating NSCLC. It lets us give high doses of radiation to the tumor without harming nearby tissues.
We use the latest in EBRT, like Intensity-Modulated Radiation Therapy (IMRT) and Image-Guided Radiation Therapy (IGRT). These help us be more precise and cut down on side effects. They let us adjust the treatment to fit the patient’s body and how the tumor moves.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) is a big step forward in treating early-stage NSCLC. It gives high doses of radiation in just a few sessions. It’s great for those who can’t have surgery or have few other options.
SBRT is very precise, allowing us to give high doses of radiation to the tumor. This helps keep the tumor from growing back. Our team is skilled in SBRT, giving patients a non-invasive option that can greatly improve their quality of life.
We mix advanced radiation therapy techniques into our treatment plans. This helps us treat NSCLC well while keeping side effects low. We’re committed to using the newest technology and best practices to give our patients the best care.
Treatment Option 3: Traditional Chemotherapy
For those with advanced NSCLC, traditional chemotherapy is key. We focus on effective treatments with fewer side effects. This helps improve patient outcomes.
Traditional chemotherapy is important for treating NSCLC, mainly for advanced cases. Platinum-based chemotherapy regimens have shown to increase survival rates. These regimens mix a platinum-based drug with other chemotherapy agents.
Platinum-Based Chemotherapy Regimens
Platinum-based chemotherapy is a mainstay for NSCLC, mainly for advanced cases. Combining platinum drugs with agents like docetaxel, gemcitabine, or pemetrexed boosts effectiveness. We customize these treatments based on each patient’s health, tumor details, and past treatments.
Managing Chemotherapy Side Effects
We take a thorough approach to manage side effects. This includes antiemetic therapy to prevent nausea and vomiting. We also use hematopoietic growth factors to support blood cell production. This ensures patients can handle treatment and keep their quality of life high.
Managing side effects well means watching closely and acting fast. We work closely with patients to tackle any issues that come up during treatment. We make changes as needed to ensure the best care.
Treatment Option 4: Targeted Therapy for Non-Small Cell Lung Cancer
We offer targeted therapies that are made for each patient’s NSCLC. These treatments work better because they match the cancer’s molecular makeup. Thanks to these therapies, many NSCLC patients with certain genetic changes are seeing better results.
EGFR Tyrosine Kinase Inhibitors
Patients with EGFR mutations benefit from EGFR tyrosine kinase inhibitors. These drugs block the EGFR protein. This protein is key in cell growth and survival. By stopping it, these drugs slow or stop cancer cell growth.
Examples of EGFR tyrosine kinase inhibitors include:
- Erlotinib
- Gefitinib
- Afatinib
- Osimertinib
ALK, ROS1, and BRAF Inhibitors
For those with ALK, ROS1, or BRAF genetic changes, targeted therapies are a good option. ALK inhibitors like crizotinib and alectinib work well for ALK rearrangements. ROS1 inhibitors, including crizotinib, are also effective for ROS1 fusions in NSCLC.
BRAF inhibitors, like dabrafenib, help patients with BRAF V600E mutations. These treatments have better response rates and survival rates than traditional chemotherapy. They offer new hope for those with these genetic changes.
Treatment Option 5: Immunotherapy
Immunotherapy is a big step forward in treating NSCLC. It uses the body’s immune system to fight cancer cells. This gives hope to those with advanced disease.
Checkpoint Inhibitors (PD-1/PD-L1)
Checkpoint inhibitors, like PD-1 and PD-L1, are key in fighting NSCLC. They let the immune system attack cancer cells better. PD-1 inhibitors have greatly improved survival rates for advanced NSCLC patients. PD-L1 inhibitors also offer lasting benefits for some patients.
Choosing the right checkpoint inhibitor depends on the patient’s tumor and past treatments. We watch how patients react and adjust treatments to get the best results.
Managing Immune-Related Adverse Events
Immunotherapy is effective but comes with risks. Immune-related adverse events (irAEs) can happen, from mild to severe. These include skin rashes, diarrhea, and fatigue, but serious issues like pneumonitis and hepatitis can also occur. It’s important to catch and manage these issues early to keep therapy going.
We take a proactive stance on managing irAEs. We monitor patients closely and teach them about their treatment. This way, we can quickly address any problems and keep immunotherapy working for our patients.
Treatment Option 6: Combination Chemoimmunotherapy
We’re moving towards using combination chemoimmunotherapy as a first choice for NSCLC. This method combines chemotherapy’s power with immunotherapy’s ability to boost the immune system. It could lead to better fights against tumors.
First-Line Combination Regimens
Our first-line treatments mix platinum-based chemotherapy with a checkpoint inhibitor. This could be a PD-1 or PD-L1 inhibitor. Studies show this combo can help patients with advanced NSCLC live longer and have better outcomes.
Key Components of Combination Chemoimmunotherapy:
- Platinum-based chemotherapy
- Checkpoint inhibitors (PD-1/PD-L1)
- Potential for enhanced anti-tumor immune response
Efficacy and Toxicity Considerations
Combination chemoimmunotherapy looks promising but comes with more side effects. We weigh the benefits and risks for each patient. We look at the tumor type, molecular details, and the patient’s health.
| Treatment Regimen | Efficacy Outcomes | Toxicity Profile |
|---|---|---|
| Platinum-based chemotherapy + PD-1 inhibitor | Improved OS and PFS | Increased risk of immune-related adverse events |
| Platinum-based chemotherapy + PD-L1 inhibitor | Enhanced response rates | Higher incidence of grade 3-4 adverse events |
To lessen side effects, we offer full supportive care and watch patients closely. We aim to find the best balance between fighting cancer and keeping patients healthy and happy.
Treatment Option 7: Chemoradiation Therapy
For patients with locally advanced NSCLC, chemoradiation therapy is key. It combines chemotherapy and radiation therapy. We offer chemoradiation therapy options to manage NSCLC effectively. This method is a standard treatment for locally advanced NSCLC, improving local control and survival.
Concurrent vs. Sequential Approaches
Chemoradiation therapy can be given in two ways: concurrently or sequentially. Concurrent chemoradiation means giving chemotherapy and radiation therapy at the same time. This makes cancer cells more sensitive to radiation. Sequential chemoradiation means giving them one after the other, which might reduce side effects.
We customize treatment plans based on the patient’s needs. We consider tumor size, location, and health. This way, we aim to get the best results with fewer side effects.
Toxicity Management Strategies
Managing side effects is key in chemoradiation therapy. We make sure patients can handle treatment without big problems. We use many strategies to reduce side effects, like watching symptoms closely and acting fast.
Some strategies we use include:
- Regular assessment of patient-reported symptoms
- Adjustments to treatment plans as needed
- Supportive care measures to manage side effects
Treatment Option 8: Ablative Therapies for Localized Disease
We offer ablative therapies as a less invasive way to treat localized NSCLC. This approach helps improve patient results. Ablative therapies are great for those who can’t have surgery.
Radiofrequency Ablation
Radiofrequency ablation (RFA) uses electrical currents to create heat and kill cancer cells. RFA is best for treating small, localized tumors. It targets the tumor well without harming nearby healthy tissue.
A study in the Journal of Clinical Oncology showed RFA works well for early-stage NSCLC. Its non-invasive nature makes it a good choice for those who can’t have surgery.
Cryotherapy and Microwave Ablation
We also use cryotherapy and microwave ablation. Cryotherapy freezes tumor cells to death. Microwave ablation heats and kills cancer cells with microwave energy.
| Ablative Therapy | Mechanism | Benefits |
|---|---|---|
| Radiofrequency Ablation | Heat generated by electrical currents | Precise targeting, minimally invasive |
| Cryotherapy | Freezing tumor cells | Effective for small tumors, preserves surrounding tissue |
| Microwave Ablation | Microwave energy heating | Rapid heating, effective for larger tumors |
A study in the Journal of Thoracic Oncology shows these therapies are valuable for localized NSCLC.
“Ablative therapies are increasingly being used to treat patients with early-stage NSCLC who are not surgical candidates, promising outcomes.”
We aim to give our patients effective, less invasive treatments. These options improve their quality of life and outcomes.
Treatment Option 9: Novel Targeted Therapies and Clinical Trials
We lead in NSCLC treatment, giving access to new targeted therapies and clinical trials. Our dedication to the latest research means we offer our patients the best treatments.
Emerging Molecular Targets
Research has found new targets for NSCLC, like KRAS, MET, and RET changes. New therapies targeting these are showing great promise in trials.
- KRAS inhibitors might help NSCLC patients with certain KRAS mutations.
- MET inhibitors work well for patients with MET exon 14 skipping mutations.
- RET inhibitors are being tested for NSCLC patients with RET fusions.
These new targets and therapies are big steps forward in treating NSCLC personally.
Accessing Clinical Trials
We help our patients join clinical trials for new NSCLC treatments. Trials offer a chance at life-saving treatments and help research progress.
To join trials, patients are checked to see if they qualify. Our team helps find the right trials and guides through the process.
- Initial screening to see if they can join.
- Talking about the benefits and risks of joining.
- Working with trial coordinators to sign up.
By joining trials, we give our patients new treatments and help fight NSCLC.
Treatment Option 10: Palliative and Supportive Care
Managing NSCLC goes beyond just treatments. We focus on palliative and supportive care too. Our goal is to give top-notch healthcare that meets all our patients’ needs. This helps improve their life quality during treatment.
Symptom Management Strategies
Symptom management is key in palliative care. It aims to reduce the physical and emotional pain of NSCLC. We use many ways to manage pain, shortness of breath, and other symptoms. This makes patients more comfortable and happy.
Pain management is customized for each patient. We use medicines and sometimes procedures to help. We also tackle symptoms like dyspnea and fatigue with proven methods.
Integration with Disease-Directed Therapy
Palliative care works hand in hand with treatments for NSCLC. We make sure patients get all the support they need. This covers their physical, emotional, and social health.
By mixing palliative care with treatments for NSCLC, we see better results. Patients live better lives. This way, we manage symptoms, lessen side effects, and offer emotional support.
Our dedication to palliative and supportive care shows our commitment to NSCLC management. We put our patients’ well-being first, no matter the stage of their journey.
Conclusion: Advances in NSCLC Treatment and Future Directions
The treatment for non-small cell lung cancer (NSCLC) has changed a lot in recent years. This is thanks to new targeted therapies, immunotherapy, and other innovative methods. These changes have greatly improved how well patients do.
We are committed to keeping up with these new treatments. This way, we can give our patients the best care possible. We are always watching for new research and treatments to help our patients.
New targeted therapies and immunotherapy have given us more ways to fight NSCLC. We aim to provide care that meets each patient’s specific needs. Our goal is to offer compassionate and complete care.
FAQ
What is non-small cell lung cancer (NSCLC)?
NSCLC is a common lung cancer type, making up about 85% of cases. It includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma subtypes.
How is NSCLC staged, and why is staging important?
NSCLC staging uses imaging and molecular tests to measure disease spread. It’s key for choosing the right treatment and understanding the patient’s outlook.
What are the treatment options for NSCLC?
Treatments for NSCLC include surgery, radiation, and chemotherapy. There’s also targeted therapy, immunotherapy, and combination treatments.
What is targeted therapy, and how is it used in NSCLC treatment?
Targeted therapy uses drugs that target cancer cell mutations. In NSCLC, it includes EGFR and ALK inhibitors for specific genetic changes.
What is immunotherapy, and how is it used in NSCLC treatment?
Immunotherapy boosts the immune system to fight cancer. It uses PD-1 and PD-L1 inhibitors for advanced NSCLC.
What are the benefits and risks of combination chemoimmunotherapy?
Combination chemoimmunotherapy can improve outcomes but may increase side effects. We weigh the benefits and risks to best help patients.
What is palliative and supportive care, and how is it integrated with disease-directed therapy?
Palliative care addresses physical, emotional, and social needs. It helps manage symptoms like pain and improves quality of life.
Are there any clinical trials available for NSCLC treatment?
Yes, we offer clinical trials for innovative treatments not available through standard care.
How is NSCLC treatment personalized to individual patients?
We tailor treatment based on the patient’s condition and cancer characteristics. This ensures a personalized plan.
What are the latest advancements in NSCLC treatment?
NSCLC treatment is constantly evolving. Ongoing research finds new targets and develops innovative therapies.
Reference
National Cancer Institute (NCI). Non-Small Cell Lung Cancer Treatment (PDQ). https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq
American Cancer Society (ACS). Treating Non-Small Cell Lung Cancer. https://www.cancer.org/cancer/types/lung-cancer/treating-non-small-cell.html
Cancer Research Institute (CRI). Immunotherapy for Lung Cancer. https://www.cancerresearch.org/immunotherapy-by-cancer-type/lung-cancer