Last Updated on November 4, 2025 by mcelik

Did you know millions of people worldwide suffer from sciatica discomfort and lower back pain due to herniated discs? This condition makes simple tasks hard.
Feeling nerve compression sensation and disc pain can be scary and confusing. Herniated Disc Symptoms occur when the soft center leaks out, irritating nerves.
Knowing about these symptoms is key to finding the right treatment. We’re here to help you understand and find relief.
Key Takeaways
- Herniated disc symptoms can cause severe lower back pain and sciatica discomfort.
- Nerve compression sensation is a common effect of herniated discs.
- Understanding the symptoms is key to seeking appropriate treatment.
- Herniated disc symptoms can significantly impact daily activities.
- Proper diagnosis and treatment can provide relief from disc pain.
Understanding Herniated Discs: The Basics
A herniated disc happens when the soft center leaks through a tear in the outer layer. This can press on nerves, causing pain, numbness, or weakness. These symptoms can really affect a person’s life.
What Happens When a Disc Herniates
When a disc herniates, its soft center bulges out through a tear. This can irritate nerves, leading to pain or weakness in the back, legs, or arms. The process can happen suddenly or slowly over time.
The severity of symptoms depends on how bad the herniation is and if nerves are compressed. Sometimes, a herniated disc doesn’t cause much pain. But other times, it can be very painful and affect nerve function.
Common Causes of Disc Herniation
Disc herniation often comes from aging, wear and tear, and injury. As we get older, our discs dry out and become more likely to crack. Activities like heavy lifting or bending can also stress the discs and increase the risk of herniation.
- Traumatic injuries, such as those sustained in a car accident or fall, can cause a disc to herniate.
- Repetitive strain on the spine from activities like heavy lifting or bending can weaken the disc over time.
- Genetic predisposition can play a role in the likelihood of developing a herniated disc.
Risk Factors for Developing a Herniated Disc
Several factors can make you more likely to get a herniated disc. Being between 30 and 50 years old is a big risk. Jobs that involve heavy lifting or manual labor also increase the risk. Being overweight and having a family history of disc problems are other factors.
Knowing these risk factors and taking steps to prevent them can help. Keeping a healthy weight, exercising, and lifting properly can reduce your risk of getting a herniated disc.
Herniated Disc Symptoms: A Complete Guide

Knowing the signs of a herniated disc is key to managing it well. We’ll look at the different symptoms, how they develop, and how they can vary.
Initial Signs of Disc Herniation
The first signs of a herniated disc can be quite subtle. They often start with mild pain or discomfort in the affected area. Common early symptoms include:
- Localized pain: Pain or discomfort in the lower back or neck, depending on the location of the herniated disc.
- Stiffness: Reduced flexibility or stiffness in the back or neck.
- Numbness or tingling: Sensations of numbness or tingling in the arms or legs, depending on the nerves affected.
How Symptoms Develop Over Time
As the herniation gets worse, symptoms can get stronger and spread. How fast this happens can vary. But, common changes include:
- Radiating pain: Pain that spreads from the back or neck to the limbs, following the nerve path.
- Increased numbness or tingling: These feelings can get stronger and cover more of the limbs.
- Muscle weakness: Weakness in muscles supplied by the affected nerves, leading to functional issues.
Variations in Symptom Presentation
Herniated disc symptoms can differ a lot from person to person. Several factors can influence these differences:
- Location of the herniation: Herniations in the lumbar spine tend to cause lower back pain and radiating leg pain. Cervical herniations can cause neck pain and symptoms in the arms.
- Size of the herniation: Larger herniations can cause more severe symptoms due to greater nerve compression.
- Individual tolerance: People’s sensitivity to pain and discomfort can vary, affecting how symptoms are perceived and reported.
Understanding these differences is key to diagnosis and treatment. By recognizing the diverse ways herniated disc symptoms can show up, healthcare providers can offer more tailored care.
The Sensation of Lower Back Pain from Herniated Discs
Herniated discs can cause a wide range of lower back pain sensations. This pain can be mild or very debilitating. It varies among people based on the herniation’s severity, disc location, and overall health.
Dull vs. Sharp Pain Sensations
Lower back pain from herniated discs can feel like dull aches or sharp pains. Dull pain is a persistent, nagging discomfort over a broad area. Sharp pain is more localized and feels like a stabbing or shooting sensation.
- Dull pain may be caused by the disc bulge itself or by muscle tension.
- Sharp pain is often related to nerve irritation or compression.
Movement-Related Pain
Movement can greatly affect lower back pain from herniated discs. Activities like bending, lifting, or twisting can make the pain worse. These actions put more stress on the affected disc and nerves.
Some people feel pain when bending forward. This movement can compress nerves further. Others might experience sharp pains or shooting sensations down their legs, known as sciatica.
Positional Discomfort While Sitting and Standing
The body’s position can also affect discomfort levels. Sitting for a long time can increase disc pressure, making pain worse. Standing or walking can sometimes relieve this pressure, giving temporary relief. But standing for too long can also cause discomfort, especially if it involves staying in one position.
Finding a comfortable position is key to managing herniated disc discomfort. Some people find ergonomic furniture or adjusting their posture helpful in reducing strain on the lower back.
Radiating Pain: When Discomfort Travels
A herniated disc can cause severe pain that spreads from the back to the legs. This pain happens when the disc presses on a nerve root. It makes the pain move along the nerve’s path.
Understanding Sciatica and Radiculopathy
Sciatica and radiculopathy describe pain from herniated discs. Sciatica is pain along the sciatic nerve, from the back to the legs. Radiculopathy is any pain from nerve root irritation or compression, anywhere.
We’ll look at how these conditions affect daily life. Knowing the difference between sciatica and radiculopathy helps in diagnosis and treatment.
Patterns of Radiating Leg Pain
The way leg pain spreads can differ for everyone, based on the nerve root involved. Common patterns include:
- Pain starts in the lower back and goes to the buttocks, thighs, and legs.
- Numbness or tingling in the legs or feet.
- Leg muscle weakness, making it hard to stand or walk.
These symptoms can get worse with certain activities or positions, like sitting, standing, or bending.
Factors That Worsen Radiating Pain
Several things can make radiating pain worse, including:
- Physical activity: Movements like bending or lifting can put more pressure on the nerve.
- Prolonged sitting or standing: Staying in one position too long can irritate the nerve root.
- Coughing or sneezing: Sudden, forceful actions can increase pressure inside the spine, making symptoms worse.
Knowing these factors helps manage pain better. By avoiding these triggers, people can lessen their pain and live better.
Shooting and Spinal Nerve Pain Sensations
Spinal nerve pain and shooting sensations often mean nerve root irritation from herniated discs. These feelings can be very painful and affect your life a lot. We’ll look at what shooting pain is, symptoms of nerve root irritation, and how to tell different nerve pains apart.
Characteristics of Shooting Pain
Shooting pain feels sharp and stabbing, happening suddenly, and can be very intense. It’s usually from a nerve root getting irritated by a herniated disc. This pain travels along the nerve, hitting different parts of the body based on the disc’s location.
Many people describe the pain as a sharp electric shock. This shows how intense and sudden shooting pain is. Knowing what this pain feels like is key to managing it well.
Nerve Root Irritation Symptoms
Nerve root irritation can cause pain, numbness, and tingling. When a herniated disc irritates a nerve root, it can lead to radiculopathy. This is a condition with nerve pain and other neurological symptoms.
- Pain that radiates along the nerve path
- Numbness or tingling sensations
- Muscle weakness in the affected area
These symptoms can change in how bad they are and how they affect your daily life. It’s important to know these signs to get the right medical help.
Differentiating Between Types of Nerve Pain
It’s important to tell different nerve pains apart for diagnosis and treatment. Shooting pain is often from nerve root irritation, while burning pain might be from other nerve damage or conditions.
“Accurate diagnosis is key to effective treatment. Understanding the nature of the pain helps healthcare providers choose the right interventions.”
By knowing the differences in nerve pain, doctors can make treatment plans that really help patients.
Numbness and Tingling from Herniated Discs
Numbness and tingling are common in people with herniated discs. These feelings happen when the disc presses on nerves. This can mess up how nerves work.
“Pins and Needles” Sensations
The “pins and needles” feeling, or paresthesia, is a sign of nerve pressure from a herniated disc. It feels like a prickling or tingling, like when a limb “falls asleep.” This is a sign that a nerve is being pressed or irritated. Many people with herniated discs experience this, due to the disc material rubbing against a nerve root.
Patterns of Numbness in Different Body Areas
Numbness from herniated discs can show up in different body parts. For example, a lower back herniation can cause numbness in the legs or feet. A neck herniation can lead to numbness in the arms or hands. The pattern of numbness helps doctors figure out where the problem is. This helps us plan the best treatment.
“Understanding the pattern of numbness is key to diagnosing and treating herniated discs well,” notes the American Association of Neurological Surgeons (AANS).
When Numbness Indicates Serious Nerve Compression
While numbness is usually not serious, sometimes it means nerve compression that needs quick medical help. If numbness is severe, getting worse, or with other symptoms like weakness, seek help fast. It’s important to watch your symptoms and get help if they get worse. If numbness doesn’t go away or gets worse, it could mean serious nerve damage. Getting help early can prevent long-term problems.
Burning Sensations and Nerve Compression Feelings
Burning sensations are common in people with herniated discs. This happens because of nerve compression. When a disc herniates, it can press on nerves, causing discomfort.
Causes of Burning Pain
Herniated discs cause burning pain due to nerve compression or irritation. When a disc bulges or ruptures, it can press on nerves. This disrupts nerve function, causing sensations like burning, numbness, or tingling.
Nerve Compression Mechanism: The pressure on the nerve changes how it sends signals. This can lead to pain that feels like burning, often along the nerve’s path.
Common Locations for Burning Sensations
Burning sensations from herniated discs can happen in different parts of the body. For lumbar herniated discs, the pain often goes down the leg, known as sciatica. Cervical herniated discs can cause burning pain in the arm or shoulder.
- Lower Back Herniations: Typically cause burning sensations in the legs.
- Neck Herniations: Often result in burning pain in the arms or shoulders.
Distinguishing Burning Pain
It’s important to distinguish burning pain from other symptoms for accurate diagnosis and treatment. Burning pain from herniated discs often comes with numbness, tingling, or weakness. The pain’s location and how it feels can help doctors find the cause.
To tell burning pain from other pain, look at:
- The pain’s location and how it spreads.
- Other neurological symptoms, like numbness or tingling.
- What makes the pain better or worse.
Knowing these details helps diagnose the cause of the burning sensation and find the right treatment.
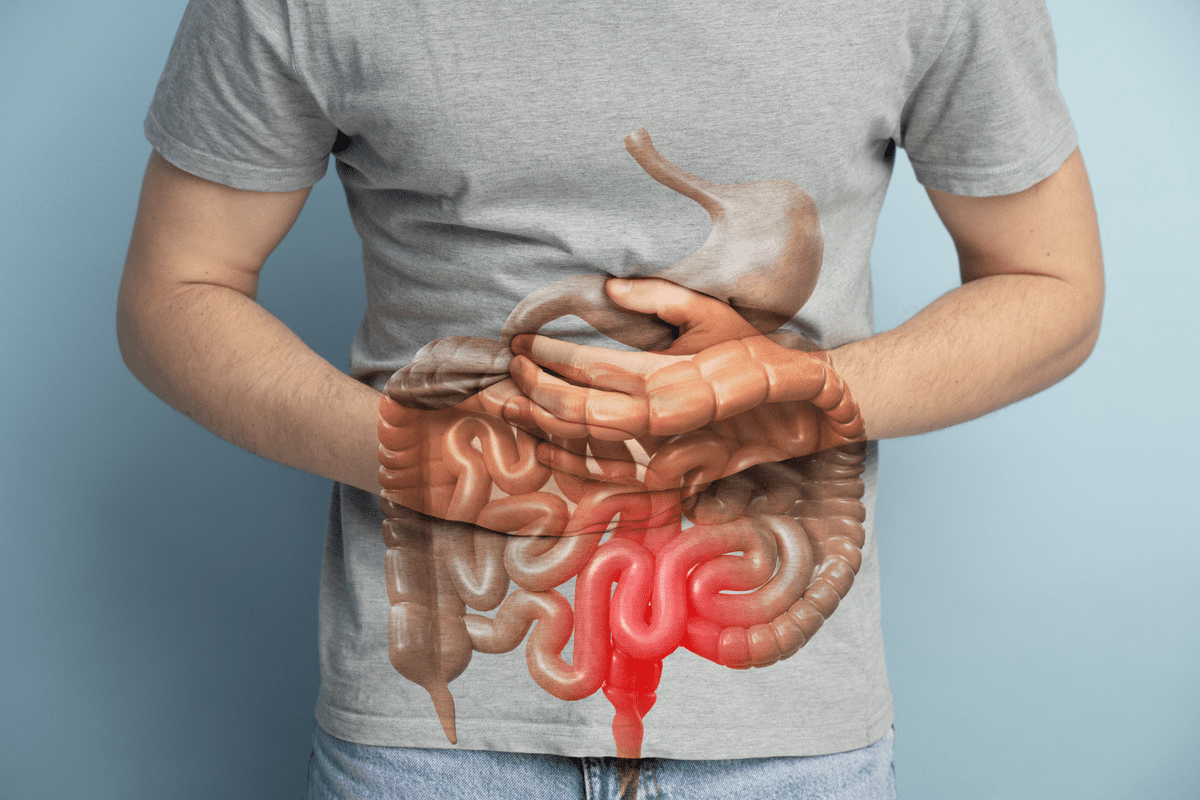
Muscle Weakness and Motor Symptoms
A herniated disc can cause muscle weakness by pressing on nerves. This can make it hard to do everyday tasks.
How Herniated Discs Affect Muscle Strength
When a disc herniates, it can press on nerves. This can mess up the signals to muscles, causing weakness. The weakness’s extent depends on the herniation’s location and severity.
Nerve compression is key in muscle strength. The more compression, the more weakness.
Common Areas of Weakness
Muscle weakness from a herniated disc varies by location. For example:
- Lower back (lumbar region) herniations can weaken legs.
- Neck (cervical region) herniations can weaken arms or hands.
Identifying specific areas affected is vital to understanding muscle strength.
Functional Limitations Due to Weakness
Muscle weakness from a herniated disc limits daily functions. Simple tasks like walking or lifting can be hard. In severe cases, it can affect daily life.
“Muscle weakness is a debilitating symptom that can drastically affect a person’s quality of life. Understanding its cause and addressing it appropriately is critical for recovery.” – An Orthopaedic Surgeon
The image below shows the complex link between nerve compression and muscle weakness. It requires careful diagnosis.
Herniated Disc in the Neck: Cervical Disc Symptoms
Symptoms of a herniated disc in the neck can vary. They can affect the neck, arms, and overall health. When a cervical spine disc herniates, it can irritate nearby nerves. This leads to different sensations and discomfort.
Unique Sensations of Cervical Herniation
Cervical herniation can cause sharp, shooting pains or a dull ache in the neck. These feelings can be constant or change based on activity and posture.
Some people feel increased pain when turning their head or moving their neck. This is because the herniated disc puts pressure on nerves, making pain worse.
Arm and Hand Symptoms
Pain or numbness in the arm and hand is a common symptom of a herniated disc in the neck. This can feel like tingling sensations or weakness in the muscles of the arm or hand. It can make everyday tasks hard to do.
The areas affected in the arm and hand vary. It depends on which nerve root is compressed by the herniated disc. For example, some people may feel symptoms in their fingers, while others may have pain or numbness in their wrists or forearms.
Headaches and Other Associated Symptoms
Herniated discs in the neck can also cause headaches. These headaches are often felt at the base of the skull or in the temples. They are a result of pain from compressed nerves in the cervical spine.
Some people may also feel dizziness or fatigue due to the discomfort and distraction from herniated disc symptoms. In severe cases, nerve compression can lead to serious symptoms like significant weakness or loss of coordination.
Limited Mobility and Stiffness in the Back
A herniated disc can cause a chain reaction of issues. This includes reduced mobility and back stiffness. These problems can make everyday activities hard.
Range of Motion Restrictions
A herniated disc can cause inflammation and irritation of the surrounding nerves. This leads to pain and stiffness. The discomfort can make it hard to bend or twist.
Patients often find it hard to move freely because of the pain. This limited mobility can be frustrating and debilitating.
Morning Stiffness vs. Activity-Related Stiffness
Morning stiffness is common in people with herniated discs. The stiffness is often worse in the morning due to the body’s natural inflammatory response. Activity-related stiffness happens after physical activities that make the condition worse.
It’s important to understand the difference between these stiffness types. Adjusting daily routines can help manage symptoms.
Impact on Daily Functioning
The limited mobility and stiffness from a herniated disc can affect daily life. Simple tasks like getting dressed or cooking can become hard. Even sitting for long periods can be challenging.
To lessen these effects, gentle exercises and stretches are recommended. They help keep flexibility and reduce stiffness.
A medical expert notes, “Maintaining a balance between rest and activity is key to managing herniated disc symptoms.”
“The key to managing herniated disc symptoms lies in understanding the condition and making appropriate lifestyle adjustments.” – Medical Expert
| Activity | Impact on Herniated Disc Symptoms | Recommendation |
| Bending | Can exacerbate symptoms | Avoid bending; use proper lifting techniques |
| Twisting | Can irritate the herniated disc | Minimize twisting motions; use core strength |
| Stretching | Can help maintain flexibility | Incorporate gentle stretches into daily routine |
Understanding the causes of limited mobility and stiffness helps individuals manage symptoms. This can improve their quality of life.
Pain When Bending and During Activities
For those with herniated discs, bending can be very painful. This pain is more than just a minor issue. It can really affect your daily life and how well you can do things.
Mechanics of Why Bending Hurts
Bending can make herniated disc symptoms worse because it adds pressure on the spine. When you bend, you might press the herniated disc more, which irritates the nerves and causes pain.
Bending involves complex spine movements like flexion and rotation. For people with herniated discs, these movements can make the condition worse, leading to more pain.
Activities That Commonly Trigger Pain
Many daily activities can make herniated disc pain worse. These include:
- Lifting heavy objects
- Bending or twisting
- Prolonged sitting or standing
- Engaging in strenuous exercise or sudden movements
Knowing which activities cause pain is key to managing symptoms well.
Strategies to Minimize Activity-Related Discomfort
To manage herniated disc pain during activities, you need the right techniques, lifestyle changes, and sometimes professional help. Here are some tips:
- Proper Lifting Techniques: Bend at the knees instead of the waist to lessen back strain.
- Regular Exercise: Do exercises that strengthen your back and abdominal muscles. This can help support your spine.
- Posture Correction: Keep good posture to reduce strain on your spine.
- Pacing Activities: Don’t overdo it. Pace your activities and take breaks regularly.
By using these strategies, people with herniated discs can reduce their pain and live better lives.
How Doctors Diagnose Herniated Disc Symptoms
To figure out if a herniated disc is causing a patient’s pain, doctors follow a detailed process. This process is key to finding the root of back pain and creating a good treatment plan.
Physical Examination Techniques
A physical exam is a big part of diagnosing a herniated disc. Doctors check the patient’s muscle strength, reflexes, and sensitivity to pain. They might do tests like the straight-leg raise to see if it makes the patient’s symptoms worse.
They also look at how well the patient can move. This helps doctors narrow down the possible causes of the symptoms and decide what tests to do next.
Imaging Studies and Their Findings
Imaging tests are very important in confirming a herniated disc diagnosis. Magnetic Resonance Imaging (MRI) is the top choice because it shows the discs, nerves, and tissues clearly. It can show where and how bad the herniation is, and if nerves are being compressed.
Computed Tomography (CT) scans or X-rays might be used, too. But MRI is usually the best because it’s very good at showing soft tissues.
Differentiating Herniated Disc Pain from Other Conditions
It can be hard to tell if someone has a herniated disc or something else. We have to think about other possible causes, like spinal stenosis or degenerative disc disease. A detailed medical history, physical exam, and imaging tests help us figure it out.
By using both clinical exams and advanced imaging, we can accurately find herniated discs. This helps us give patients the right treatment for their pain.
Treatment Options for Herniated Disc Discomfort
We know that herniated disc discomfort needs a detailed treatment plan. We’re here to help you understand your options. The right treatment depends on how bad the symptoms are, where the herniation is, and your overall health.
Conservative Management Approaches
First, we often try conservative management for herniated disc discomfort. This method aims to lessen pain, reduce swelling, boost mobility, and strengthen back muscles. Some common strategies include:
- Rest and activity modification
- Physical therapy exercises
- Chiropractic care
- Non-steroidal anti-inflammatory drugs (NSAIDs)
Physical therapy is key in this approach. It helps improve flexibility, strengthens spine-supporting muscles, and improves posture.
Medication Options for Pain Relief
Medicines can help a lot with herniated disc symptoms. Here are some common ones:
| Medication Type | Purpose | Examples |
| NSAIDs | Reduce pain and inflammation | Ibuprofen, Naproxen |
| Muscle Relaxants | Relieve muscle spasms | Cyclobenzaprine |
| Oral Steroids | Reduce severe inflammation | Prednisone |
Physical Therapy Interventions
Physical therapy is a big part of herniated disc treatment. It offers many ways to ease pain and improve function. These can include:
- Manual therapy techniques
- Exercise programs tailored to the patient’s needs
- Modalities such as heat, cold, or electrical stimulation
- Education on proper body mechanics and posture
Exercise programs are very important. They help strengthen muscles around the spine, which improves support and lowers injury risk.
Surgical Considerations
If conservative management doesn’t work, surgery might be needed. There are different surgical options for herniated discs, like:
- Discectomy: Removing the herniated part of the disc
- Microdiscectomy: A less invasive version of discectomy
- Spinal fusion: Joining the vertebrae together to stabilize the spine
Surgery is usually for severe cases with nerve compression causing a lot of pain, weakness, or neurological problems.
Self-Care Strategies for Managing Symptoms
Using the right self-care can really help people with herniated disc symptoms. By trying home remedies, making ergonomic changes, adjusting exercises, and sleeping properly, you can feel better. These steps can help you manage pain and boost your overall health.
Home Remedies for Pain Relief
Home remedies can really help with herniated disc pain. Using heat or cold packs on the area can lessen pain and swelling. Make sure to put a towel between the pack and your skin. Also, over-the-counter pain relievers can help, but always follow the dosage and talk to a doctor first.
- Apply heat or cold packs to the affected area
- Use over-the-counter pain relievers as directed
- Practice relaxation techniques such as deep breathing or meditation
Ergonomic Adjustments
Making your workspace ergonomic can really help your back. Make sure your workspace is set up right to avoid making things worse. Adjust your chair, monitor, and keyboard to keep good posture.
- Adjust your chair height to support your lower back
- Position your monitor directly in front of you at eye level
- Keep your keyboard and mouse close to your body
Exercise and Movement Modifications
Changing your exercise routine can help with herniated disc symptoms. Gentle exercises like yoga or swimming are good. Avoid heavy lifting or bending, and learn how to lift properly.
- Engage in low-impact exercises like yoga or swimming
- Avoid heavy lifting or bending
- Learn proper lifting techniques
Sleep Positioning for Symptom Relief
How you sleep can help with herniated disc symptoms. Sleeping on your back with a pillow under your knees or on your side with a pillow between your knees can ease spine strain.
- Sleep on your back with a pillow under your knees
- Sleep on your side with a pillow between your knees
- Avoid sleeping on your stomach
By using these self-care strategies every day, you can better manage your herniated disc symptoms. This can greatly improve your quality of life.
Conclusion: Living with and Managing Herniated Disc Symptoms
Understanding and managing herniated disc symptoms is key to a better life. We’ve looked at the different feelings caused by herniated discs, like lower back pain and numbness. Knowing the signs helps people get the right medical help and take care of themselves.
Dealing with a herniated disc needs a full plan. This includes trying conservative treatments, making lifestyle changes, and sometimes getting medical help. By managing symptoms well, people can feel less pain and do more every day. We stress the need for good herniated disc care, like using ergonomic tools, exercising right, and sleeping well.
By being proactive and working with doctors, people can handle herniated disc symptoms better. Our aim is to help and guide those affected. We want to empower them to manage their condition well and live comfortably with a herniated disc.
FAQ
What are the common symptoms of a herniated disc?
Symptoms include lower back pain and pain that shoots down your leg (sciatica). You might also feel numbness, tingling, muscle weakness, and have trouble moving. The severity and type of symptoms vary based on the herniation’s location and extent.
How does a herniated disc cause pain?
A herniated disc can irritate nearby nerves, causing inflammation and discomfort. This pain can stay in the back or spread to your legs or arms, depending on where the herniation is.
What is the difference between sciatica and radiculopathy?
Sciatica is pain that travels down the sciatic nerve, from your lower back to your legs. Radiculopathy is a broader term for symptoms caused by nerve compression. It includes pain, numbness, tingling, and weakness in various body parts, not just the legs.
Can a herniated disc cause numbness and tingling?
Yes, a herniated disc can cause numbness and tingling by pressing on nearby nerves. These feelings can happen in the areas served by the affected nerve, like your legs or arms.
How is a herniated disc diagnosed?
Doctors use a physical exam, medical history, and imaging like MRI or CT scans to diagnose. These tests confirm the herniated disc and rule out other causes of symptoms.
What are the treatment options for a herniated disc?
Treatment options include physical therapy, pain relief medication, and sometimes surgery. The choice depends on the severity of symptoms, the herniation’s extent, and individual factors.
Can I manage herniated disc symptoms at home?
Yes, you can manage symptoms with self-care. This includes home remedies, ergonomic adjustments, exercise modifications, and sleep techniques.
Will a herniated disc always require surgery?
No, surgery isn’t always needed. Many cases are managed with physical therapy, medication, and lifestyle changes. Surgery is considered for severe cases or when other treatments fail.
Can a herniated disc cause muscle weakness?
Yes, a herniated disc can weaken muscles by affecting nearby nerves. The weakness’s location depends on the herniation’s spot and the nerves involved.
How can I prevent herniated disc symptoms from worsening?
To prevent symptoms from getting worse, keep your back healthy with regular exercise, proper lifting, and good posture. Avoid heavy lifting, bending, or twisting to reduce discomfort.
Reference
- Dydyk, A. M., et al. (2023). Disk Herniation. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK441822/