Last Updated on November 20, 2025 by Ugurkan Demir

Anaemia in newborns is a serious issue often caused by rhesus disease. It happens when the mother’s blood type doesn’t match the baby’s, leading to haemolytic anaemia. This is because of blood group incompatibility, mainly with Rh or ABO types.
Liv Hospital focuses on families, giving them the knowledge they need. They help identify symptoms and causes of rhesus disease in newborns. Knowing about this condition is key for quick action and treatment.
Key Takeaways
- Rhesus disease is a leading cause of anaemia in newborns.
- Blood group incompatibility is the primary cause of HDFN.
- Prompt recognition and treatment are critical.
- Liv Hospital offers a patient-centered approach.
- International expertise backs the treatment protocols.
Understanding Anaemia in Newborn Babies

Anaemia in newborns means they have low hemoglobin levels. This can affect their health and growth. Hemoglobin is a protein in red blood cells that carries oxygen. Newborns can get anaemia from different reasons like blood group issues, infections, or genetic problems.
Definition and Normal Hemoglobin Levels
Anaemia in newborns is when their hemoglobin is below what’s normal for their age. Normal hemoglobin levels in newborns are between 14 to 24 g/dL. Low hemoglobin levels can reduce oxygen to tissues and organs, causing health problems.
The normal hemoglobin range for newborns is as follows:
- At birth: 14-24 g/dL
- 1-2 weeks: 12-20 g/dL
- 1-3 months: 9.5-13.5 g/dL
Impact on Newborn Development and Health
Anaemia can greatly affect a newborn’s growth and health. Severe anaemia can cause:
- Poor weight gain
- Delayed development
- Increased risk of infections
- In severe cases, heart problems and even death
Also, anaemia can have long-term effects on a child’s health and development. It’s important to find and treat anaemia early to avoid these issues.
Anaemia in Newborn: Causes and Classification

It’s important to know why newborns get anaemia and how it’s classified. Anaemia can happen for many reasons, from normal changes to serious health issues.
Physiological Anaemia of Infancy
Physiological anaemia is common in newborns, but more so in preterm babies. It happens when they switch from fetal to adult hemoglobin. Monitoring hemoglobin levels is key to tell if it’s just a normal change or something more serious.
Pathological Causes of Newborn Anaemia
Pathological anaemia in newborns can come from hemorrhage, hemolysis, or less red blood cell production. Bleeding can happen during birth or because of issues with the placenta. Hemolysis, or breaking down of red blood cells, can be caused by blood group differences, like Rh or ABO incompatibility. This can lead to rhesus haemolytic disease.
Haemolytic Anaemia in Newborns
Haemolytic anaemia means red blood cells break down too early. It can be caused by blood group differences, infections, or genetic problems with red blood cells. Early diagnosis and treatment are vital to avoid serious problems.
Knowing if a newborn’s anaemia is physiological or pathological helps doctors decide how to treat it. Understanding the cause is key to giving the right care.
Rhesus Disease: Primary Cause of Haemolytic Anaemia in Newborns
When a mother’s blood type doesn’t match her baby’s, Rhesus disease can occur. This disease causes severe anaemia in newborns. It happens when the mother’s immune system attacks the baby’s red blood cells, destroying them.
What is Rhesus Disease?
Rhesus disease, or Rh disease, happens when blood types don’t match between mother and baby. This mismatch makes the mother’s immune system attack the baby’s red blood cells. This leads to anaemia, where red blood cells are destroyed too quickly.
Pathophysiology of Rhesus Incompatibility
The mother’s immune system gets sensitized to the baby’s Rh-positive blood. This can happen during pregnancy, childbirth, or when their blood mixes. Once sensitized, the mother’s body makes antibodies that can harm an Rh-positive baby in future pregnancies.
The severity of Rhesus disease varies. Mild cases might cause only a little anaemia. But severe cases can lead to serious anaemia, heart problems, and even death.
Maternal-Fetal Blood Interactions
The way maternal and fetal blood interact is key to Rhesus disease. During pregnancy, the placenta keeps their blood separate. But sometimes, fetal blood can get into the mother’s, causing an immune reaction. This risk is higher during childbirth or abortion, when blood mixing is more common.
Knowing how these blood interactions work helps manage Rhesus disease. Giving Rh immunoglobulin to Rh-negative mothers can prevent the disease. Monitoring for sensitization and managing pregnancies with Rh incompatibility are also important to avoid complications.
7 Key Symptoms of Rhesus Disease in Newborns
Rhesus disease in newborns shows several key symptoms. Healthcare providers must recognize these signs. This disease, also known as hemolytic disease of the newborn (HDN), happens when the mother’s and baby’s blood types don’t match.
Pale Skin and Jaundice
Pale skin is a main symptom of Rhesus disease. It’s caused by anemia from destroyed red blood cells. Newborns also often have jaundice, which makes their skin and eyes yellow. This is because of high bilirubin levels.
Rapid Breathing and Elevated Heart Rate
Newborns with Rhesus disease breathe fast and have a high heart rate. Their bodies try to make up for less oxygen in their blood because of anemia.
Lethargy and Poor Feeding Patterns
Lethargy and poor feeding patterns are common too. These signs show how severe the disease is. The newborn might be too weak to eat well.
Hypotonia (Low Muscle Tone)
Some newborns with Rhesus disease have hypotonia, or low muscle tone. This is a sign of how the disease affects their health and development.
The other three key symptoms include:
- Enlarged liver or spleen
- Swelling or edema
- Hemolytic anemia
| Symptom | Description |
| Pale Skin | Resulting from anemia caused by red blood cell destruction |
| Jaundice | Yellowing of skin and eyes due to elevated bilirubin |
| Rapid Breathing | Compensatory mechanism for reduced oxygen-carrying capacity |
| Lethargy | Indicative of overall disease severity and weakness |
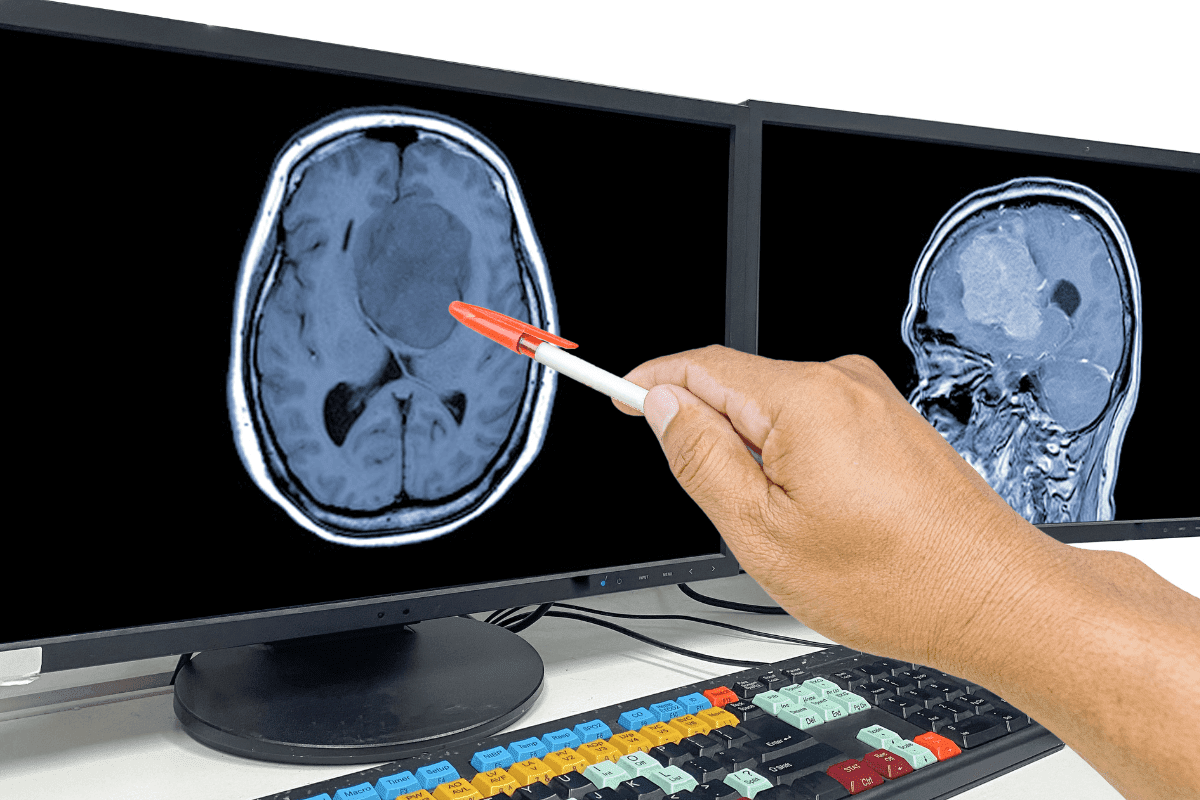
Diagnosing Anaemia and Rhesus Disease in Newborns
Diagnosing anaemia and Rhesus disease in newborns requires several steps. These include a clinical assessment and advanced lab tests. Finding these conditions early is key to treating them effectively.
Clinical Assessment and Physical Examination
A thorough physical check-up is the first step. Healthcare providers look for signs like pale skin, jaundice, and fast breathing. These signs can point to anaemia or Rhesus disease.
Key clinical findings include:
- Pale or jaundiced skin
- Rapid breathing or elevated heart rate
- Lethargy or poor feeding patterns
- Hypotonia (low muscle tone)
Laboratory Tests for Low Hemoglobin in Infants
Lab tests are vital for diagnosing anaemia and Rhesus disease. These tests include:
| Test | Purpose |
| Complete Blood Count (CBC) | Measures hemoglobin levels and red blood cell count |
| Bilirubin Levels | Assesses jaundice severity |
| Direct Coombs Test | Detects antibodies against red blood cells |
A study in the Journal of Pediatrics found that early treatment of Rhesus disease improves outcomes. It says early diagnosis and treatment are critical.
“The diagnosis of Rhesus disease requires a combination of clinical assessment and laboratory tests to identify affected newborns and guide treatment decisions.”
Prenatal Screening and Monitoring
Prenatal screening is key to spotting pregnancies at risk for Rhesus disease. It checks for maternal RBC antibodies and monitors their levels.
During prenatal care, doctors track antibody levels. This helps predict if interventions like intrauterine transfusions will be needed.
Good prenatal screening and monitoring can lower the risk of Rhesus disease complications in newborns.
Treatment Approaches for Rhesus Haemolytic Disease
Managing Rhesus haemolytic disease is key to helping newborns. This condition happens when the mother’s and baby’s blood types don’t match. A detailed treatment plan is needed to lessen its impact.
Intrauterine Transfusions for Fetal Anaemia
Intrauterine transfusions are vital for babies with severe anaemia from Rhesus incompatibility. This method involves giving compatible blood to the fetus under ultrasound. It boosts the baby’s hemoglobin and lowers the risk of serious problems.
Key benefits of intrauterine transfusions include:
- Improved fetal hemoglobin levels
- Reduced risk of heart failure and other complications
- Enhanced chances of a successful pregnancy outcome
Phototherapy for Neonatal Jaundice
Phototherapy is a common treatment for neonatal jaundice, a side effect of Rhesus haemolytic disease. It uses light to break down bilirubin. This reduces the risk of brain damage and other serious issues.
Exchange Transfusion Procedures
Exchange transfusion is needed for severe jaundice or anaemia. It replaces the baby’s blood with donor blood to quickly lower bilirubin. This improves oxygen delivery to the body’s tissues.
The process of exchange transfusion is carefully monitored to ensure the newborn’s safety and the effectiveness of the treatment.
Supportive Care and Monitoring
Supportive care is essential for Rhesus haemolytic disease. Newborns need constant monitoring for anaemia, jaundice, and other issues. They also need nutritional support for growth and development.
- Regular monitoring of hemoglobin and bilirubin levels
- Nutritional support and guidance on feeding
- Follow-up appointments to assess long-term outcomes
Healthcare providers use a variety of treatments to improve outcomes for babies with Rhesus haemolytic disease.
Long-term Effects and Complications of Untreated Rhesus Disease
Untreated Rhesus disease can harm a newborn’s health and future. It can cause severe anemia and lead to brain damage and hearing loss. This can affect a child’s development and quality of life.
Neurological and Developmental Outcomes
Untreated Rhesus disease can harm a child’s brain and development. It can cause permanent brain damage, leading to conditions like cerebral palsy. Early treatment is key to avoid these problems (National Center for Biotechnology Information).
Hearing and Vision Impairments
Rhesus disease can also cause hearing and vision problems. It can lead to deafness and vision issues, including blindness. Regular checks and early treatment are important to prevent these issues.
Follow-up Care Requirements
Children with Rhesus disease need ongoing care to monitor their health. They need regular doctor visits, hearing and vision tests, and developmental screenings. A team of healthcare professionals can help manage these children’s needs.
| Complication | Potential Long-term Effect | Follow-up Care |
| Kernicterus | Neurodevelopmental impairment, cerebral palsy | Regular neurological assessments, physical therapy |
| Sensorineural Deafness | Hearing loss | Audiological evaluations, hearing aids |
| Severe Jaundice | Vision impairments, blindness | Ophthalmological exams, vision therapy |
In conclusion, untreated Rhesus disease can have severe and lasting consequences for newborns. Understanding these risks and implementing appropriate follow-up care can significantly improve long-term outcomes for affected children.
Prevention Strategies for Rhesus Disease
Rhesus disease prevention has made big strides, cutting down on Rh-induced Hemolytic Disease of the Newborn (HDFN). The main goal is to understand how Rh sensitization works and use effective ways to stop it.
Rh Immunoglobulin (RhIg) Administration Protocol
Rh Immunoglobulin (RhIg) is key in stopping Rhesus disease. It’s given to Rh-negative moms at certain times in and after pregnancy. RhIg has greatly helped lower the risk of Rh-induced HDFN.
The RhIg shot plan includes:
- Getting it at 28 weeks of pregnancy
- After the baby is born if it’s Rh-positive
- After any events that might cause sensitization, like amniocentesis or bleeding
Prenatal Care Guidelines for Rh-negative Mothers
For Rh-negative moms, prenatal care is all about watching for Rh sensitization signs. This means:
- Regular blood tests for Rh antibodies
- Checking on the baby’s health with ultrasound and other tests
- Planning for possible treatments, like intrauterine transfusions, if needed
Spotting and handling Rh sensitization early is key to avoiding serious problems for the baby.
Genetic Counseling and Family Planning
Genetic counseling is vital for Rh-negative people, even more so if they’ve had Rh sensitization before. Counselors share the risks of Rh incompatibility and how to manage them in future pregnancies.
Symptoms of Rhesus Disease in Adults: A Rare Occurrence
While Rhesus disease mostly hits newborns, adults can rarely get symptoms from Rh sensitization. This might happen after getting blood from an Rh-positive donor. Knowing these risks is important for adult care.
Conclusion
Anaemia in newborns can be very serious if not caught early. Rhesus disease is a big reason for this problem. Knowing the signs is key to spotting it fast.
The symptoms of Rhesus disease in babies can vary. They might look pale, have jaundice, breathe fast, or seem very tired. Giving Rh immunoglobulin to Rh-negative moms during pregnancy can prevent it.
Spotting anaemia early in babies is very important. It helps avoid serious problems later on. Doctors can do better for babies with Rhesus disease by knowing how to treat it.
We can stop Rhesus disease before it starts. This includes checking for it during pregnancy. By acting fast, we can make sure babies stay healthy.
FAQ
What is Rhesus disease and how does it affect newborns?
Rhesus disease, also known as Rh incompatibility, happens when a mother’s Rh-negative blood reacts to her baby’s Rh-positive blood. This reaction leads to the production of antibodies. These antibodies can destroy the baby’s red blood cells, causing haemolytic anaemia.
What are the symptoms of Rhesus disease in newborns?
The symptoms of Rhesus disease in newborns include pale skin and jaundice. They also have rapid breathing, lethargy, and hypotonia. Poor feeding patterns and an elevated heart rate are also signs.
How is anaemia in newborns diagnosed?
Anaemia in newborns is diagnosed through clinical assessment and physical examination. Laboratory tests, like complete blood count (CBC) and blood smear, are also used. These tests check for low hemoglobin levels and red blood cell abnormalities.
What is the treatment for Rhesus haemolytic disease?
Treatment for Rhesus haemolytic disease includes intrauterine transfusions and phototherapy. Exchange transfusion procedures and supportive care are also used. These help manage anaemia, jaundice, and other complications.
Can Rhesus disease be prevented?
Yes, Rhesus disease can be prevented. Rh immunoglobulin (RhIg) administration to Rh-negative mothers during pregnancy and after delivery helps. Prenatal care guidelines and genetic counseling are also important.
What are the long-term effects of untreated Rhesus disease?
Untreated Rhesus disease can lead to neurological and developmental issues. It can also cause hearing and vision impairments. This highlights the need for early detection and proper treatment.
Can adults experience symptoms of Rhesus disease?
While rare, adults can experience symptoms related to Rh incompatibility. This is not typically referred to as Rhesus disease. It mainly affects newborns.
How is haemolytic anaemia in newborns managed?
Haemolytic anaemia in newborns is managed by treating the underlying cause, like Rhesus disease. Supportive care, including transfusions and phototherapy, is also used. Monitoring is done to prevent complications.
What is the role of prenatal screening in preventing Rhesus disease?
Prenatal screening is key in identifying Rh-negative mothers. It helps monitor their pregnancy to prevent Rhesus disease. This is done through timely administration of RhIg and other interventions.
References
- NHS. (2021). Rhesus disease – Symptoms.