Last Updated on November 20, 2025 by Ugurkan Demir
Aplastic anemia is a rare and serious disease. It happens when the bone marrow can’t make enough blood cells. This leads to pancytopenia and causes a lot of health problems and even death.
We will look at the important factors that affect the prognosis of this condition in adults. We will also talk about what it means for patients looking for treatment at places like Liv Hospital.
Knowing the prognosis of aplastic anemia is key to managing it well. It helps improve how patients do after treatment.
Key Takeaways
- Understanding the definition and impact of aplastic anemia on adults.
- Recognizing the importance of prognosis in managing the condition.
- Identifying key factors that influence aplastic anemia prognosis.
- Exploring treatment options and their effects on patient outcomes.
- Learning about the complete care given by specialized institutions.
Etiology of Aplastic Anemia in Adult Patients
The causes of aplastic anemia in adults are complex. They involve both genetic and environmental factors. Knowing these causes helps doctors predict outcomes and choose treatments.
Idiopathic Causes: The Unknown Origins
Many cases of aplastic anemia have no known cause, called idiopathic aplastic anemia. Research suggests that genetics and environment might play a role in these cases.
“The majority of aplastic anemia cases are idiopathic, highlighting the need for further research into the underlying causes.”
Source: Aplastic Anemia Research Foundation
Drug and Toxin-Induced Aplastic Anemia
Some drugs and toxins can cause aplastic anemia. Common culprits include certain antibiotics, anticonvulsants, and chemicals like benzene and pesticides.
| Drug/Toxin Category | Examples |
| Antibiotics | Chloramphenicol, Sulfonamides |
| Anticonvulsants | Phenytoin, Carbamazepine |
| Chemicals | Benzene, Pesticides |
Viral Infections and Autoimmune Triggers
Viral infections, like hepatitis and HIV, can lead to aplastic anemia. Autoimmune mechanisms might also be involved, where the immune system attacks the bone marrow by mistake.
We will look at how to diagnose and treat aplastic anemia in adults next. This will build on what we know about its causes.
Diagnostic Approach to Aplastic Anemia

To diagnose aplastic anemia, doctors use lab tests and bone marrow exams. This detailed method is key to confirming the diagnosis and understanding how severe the condition is.
Laboratory Findings and Blood Film Characteristics
Labs play a big role in diagnosing aplastic anemia. Key findings include:
- Pancytopenia, which means a drop in all blood cell types.
- A normocytic or macrocytic anemia, often with a low reticulocyte count.
- Neutropenia, which raises the risk of infections.
- Thrombocytopenia, leading to bleeding tendencies.
The blood smear usually shows few cells, with no abnormal cells or blasts. This helps tell aplastic anemia apart from other bone marrow issues.
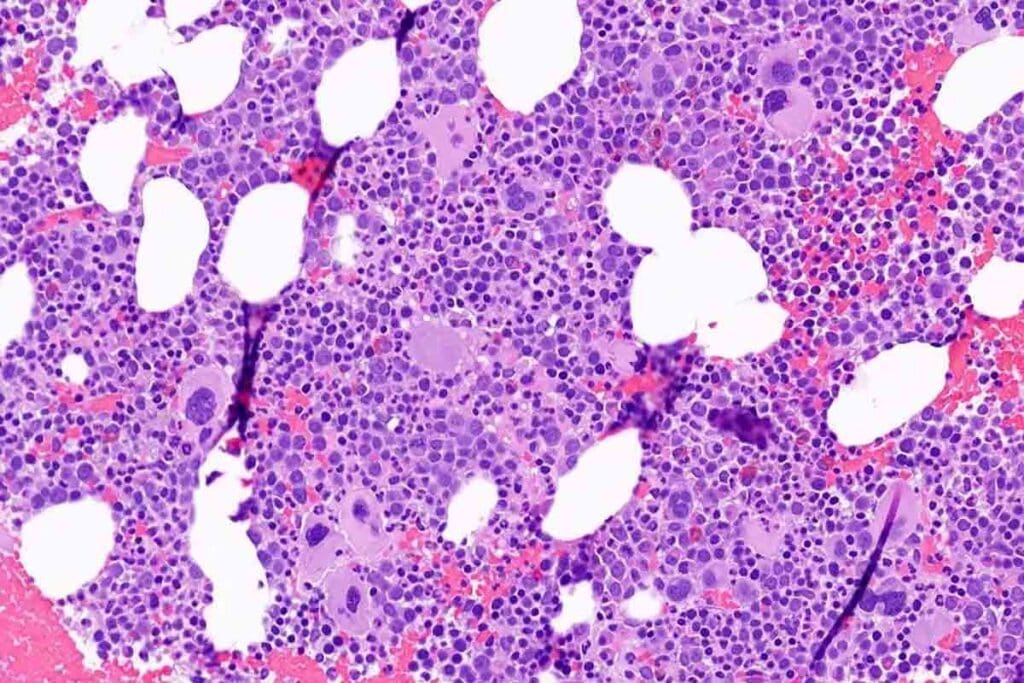
Bone Marrow Histology in Aplastic Anemia
Bone marrow biopsy is key to diagnosing aplastic anemia. The findings typically show:
- A hypocellular marrow, with a big drop in hematopoietic cells.
- An increase in fat cells changes the marrow’s look.
- Absence or reduction of megakaryocytes, myeloid, and erythroid precursors.
These signs are important for telling aplastic anemia apart from other pancytopenia causes.
Differential Diagnosis of Aplastic Pancytopenia
Other conditions can also cause pancytopenia, making diagnosis tricky. These include:
| Condition | Key Features |
| Myelodysplastic Syndromes (MDS) | Dysplastic cells, often with blasts in the marrow |
| Acute Leukemia | Blasts in the peripheral blood or bone marrow |
| Bone Marrow Infiltration | Presence of malignant cells or fibrosis in the marrow |
A detailed diagnostic process is needed to tell aplastic anemia apart from these conditions.
Classification of Disease Severity
Knowing how severe aplastic anemia is is key to figuring out the treatment. Doctors use a system to see how bad the bone marrow failure is. This helps them manage the disease better.
Aplastic anemia is split into levels based on how bad the bone marrow and blood cells are. These levels help doctors plan the best treatment and estimate how well a patient will do.
Criteria for Mild, Moderate, and Severe Aplastic Anemia
The severity of aplastic anemia is usually mild, moderate, or severe. Mild aplastic anemia has only a slight drop in blood cells, and patients might not show many symptoms. On the other hand, severe aplastic anemia has a big drop in all blood cells, showing a serious bone marrow failure.
The criteria for classifying the severity include:
- Absolute neutrophil count (ANC)
- Platelet count
- Reticulocyte count
- Bone marrow cellularity
These factors help doctors figure out how bad the disease is and pick the best treatment.
Very Severe Aplastic Anemia: Definition and Implications
Very severe aplastic anemia is when the blood cell drop is even worse, with an ANC of less than 0.2 x 10^9/L. This is a very serious condition that needs quick and strong treatment, like immunosuppressive therapy or a stem cell transplant.
Being diagnosed with very severe aplastic anemia means you need to act fast to avoid serious problems like infections and bleeding. Knowing the severity helps everyone involved make better choices about treatment and what to expect.
Treatment Approaches That Influence Prognosis
We treat aplastic anemia with a mix of immunosuppressive therapy, hematopoietic stem cell transplantation, and supportive care. The treatment choice greatly affects the patient’s outcome.
Immunosuppressive Therapy: First-Line Treatment
Immunosuppressive therapy (IST) is the first choice for many patients with aplastic anemia. It’s for those who can’t get a transplant or are waiting. IST usually includes antithymocyte globulin (ATG) and cyclosporine.
Benefits of IST:
- Improves blood counts
- Can make patients not need transfusions
- May increase survival chances
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation (HSCT) is a cure for aplastic anemia. It replaces the patient’s bone marrow with healthy stem cells from a donor.
| Donor Type | Success Rate | Graft-Versus-Host Disease (GVHD) Risk |
| Matched Sibling Donor | 80-90% | Moderate |
| Unrelated Donor | 70-80% | Higher |
| Haploidentical Donor | 60-70% | Higher |
Supportive Care Measures
Supportive care is key in managing aplastic anemia. It aims to ease symptoms and prevent problems.
Key Supportive Care Measures:
- Blood transfusions for anemia and low platelets
- Antimicrobial prophylaxis to prevent infections
- Growth factor support to boost blood cell production
Combining these treatments has greatly improved aplastic anemia outcomes. Healthcare providers can tailor treatments based on each patient’s needs.
Aplastic Anemia Prognosis in Adults: Overview of Outcomes
Adults with aplastic anemia face a complex prognosis. Modern treatments have greatly improved survival rates. This condition, where the bone marrow fails to make blood cells, has seen big changes in how it’s managed.
Historical Perspective on Survival Rates
Before modern treatments, the outlook was very bad. High death rates were due to infections, bleeding, and other issues from bone marrow failure. Many patients died soon after being diagnosed.
A study found that supportive care, like blood transfusions and antibiotics, helped improve outcomes.
“The prognosis of aplastic anemia has changed dramatically over the past few decades, largely due to advancements in immunosuppressive therapy and hematopoietic stem cell transplantation.”
Modern Five-Year Survival Statistics
Recently, the outlook for adults with aplastic anemia has gotten much better. New treatments, like immunosuppressive therapy and hematopoietic stem cell transplantation, have greatly improved survival rates. The five-year survival rate for adults with aplastic anemia has gone up, thanks to these modern treatments.
Key factors contributing to improved survival include:
- Early diagnosis and intervention
- Advances in immunosuppressive therapy
- Increased availability and success of hematopoietic stem cell transplantation
- Better supportive care measures
These changes have greatly improved the prognosis for adults with aplastic anemia. They offer hope for better outcomes and a better quality of life.
Key Factor 1: Age and Its Impact on Survival
Understanding how age affects aplastic anemia is key. Age is a big factor in how well someone does with the disease. Younger people usually do better than older ones.
Prognosis in Adults Under 40
Adults under 40 often do well with aplastic anemia. They usually respond well to treatments like immunosuppressive therapy and hematopoietic stem cell transplantation. Younger adults tend to live longer and have better outcomes than older adults.
Outcomes in Middle-Aged and Elderly Patients
But middle-aged and elderly patients face bigger challenges. They might have other health issues and not as strong bodies. This makes it harder for them to handle treatments.
Yet, new treatments and care have helped older adults, too. Tailored treatment approaches can make a big difference. They help improve life quality and survival chances.
Healthcare providers need to look at each patient’s situation closely. They should consider age and other important factors. This way, we can help everyone with aplastic anemia live better lives.
Key Factor 2: Disease Severity as a Prognostic Indicator
Disease severity is key in predicting outcomes for adults with aplastic anemia. It’s measured by blood counts and bone marrow cellularity. These help show how bad the bone marrow failure is and its effect on patients.
Blood Count Values and Survival Correlation
Blood counts are vital in showing how severe aplastic anemia is. Low counts of neutrophils, platelets, and red blood cells mean a worse outlook. Here’s what’s concerning:
- Severe neutropenia (ANC
- Thrombocytopenia (platelet count
- Severe anemia (hemoglobin
Research shows that those with severe pancytopenia at diagnosis face lower survival rates. Early treatment is key to bettering their chances.
Bone Marrow Cellularity and Long-term Outcomes
Bone marrow cellularity is also a key factor. Aplastic anemia is marked by a hypocellular bone marrow, filled with fat cells. How hypocellular it is shows how severe the disease is.
Those with very hypocellular marrow face a tougher prognosis than those with moderate hypocellularity. Recovery of bone marrow function, either on its own or with treatment, affects long-term outcomes.
| Bone Marrow Cellularity | Long-term Survival Rate |
| Severe Hypocellularity | Lower survival rates |
| Moderate Hypocellularity | Improved survival rates with treatment |
| Mild Hypocellularity | Higher survival rates |
In summary, disease severity is a major factor in predicting outcomes for aplastic anemia. Blood counts and bone marrow cellularity give vital clues about disease severity and its impact. Knowing this helps doctors plan better treatments and improve survival chances.
Key Factor 3: Response to Immunosuppressive Therapy
How well a person responds to immunosuppressive therapy is key in treating aplastic anemia. This therapy, which includes antithymocyte globulin (ATG) and cyclosporine, tries to stop the immune system from attacking the bone marrow. This helps improve blood counts.
Early Response Patterns and Their Significance
An early positive response to this therapy is a good sign. People who see improvements in their blood counts early on usually do better. This early success often means more reticulocytes and better blood cell counts.
Table: Early Response Patterns to Immunosuppressive Therapy
| Response Timeframe | Characteristics | Prognostic Implication |
| 1-3 months | Increase in reticulocyte count | Favorable prognosis |
| 3-6 months | Improvement in other blood cell lines | Better overall outcome |
Refractory Disease and Alternative Approaches
Some people don’t get better with the first treatment, known as refractory aplastic anemia. For these cases, doctors look at other options. This can include different treatments, new therapies, or even stem cell transplants.
Relapse Rates and Management Strategies
It’s a worry when someone’s condition gets worse after they seemed to get better. Research shows that how often this happens can vary. Doctors might try the treatment again, offer support, or even think about stem cell transplants.
Managing a relapse well means keeping a close eye on blood counts and bone marrow. Acting quickly can help avoid serious problems and improve chances of living longer.
Key Factor 4: Stem Cell Transplantation Outcomes
For many patients with aplastic anemia, stem cell transplantation is a life-saving option. The success of this treatment depends on the donor match and when it happens. Hematopoietic stem cell transplantation can lead to remission in aplastic anemia. The results vary based on the donor match and other factors.
Matched Sibling Donor Results
Having a matched sibling donor leads to better outcomes for stem cell transplantation. Survival rates are significantly higher than those from unrelated or haploidentical donors. Patients with a matched sibling donor face lower risks of graft-versus-host disease (GVHD) and other complications.
Unrelated and Haplocidentical Donor Outcomes
For those without a matched sibling donor, unrelated or haploidentical donors are options. While outcomes may not be as good, new transplant techniques have boosted survival rates. Careful donor selection and matching are key to reducing GVHD risk and achieving the best results.
Transplantation Timing and Its Effect on Prognosis
The timing of stem cell transplantation is vital for patient outcomes. Early transplantation is linked to better survival rates, mainly in severe aplastic anemia cases. The decision on when to transplant should consider the patient’s health, disease severity, and donor availability.
Understanding the factors that affect stem cell transplantation outcomes helps us guide patients and their families. This way, we can improve their chances of a successful treatment.
Key Factor 5: Comorbidities and Their Influence
It’s key to know how comorbidities affect aplastic anemia management. Comorbidities, or existing health issues, can change how well a treatment works for adults with aplastic anemia.
Impact of Pre-existing Conditions
Pre-existing conditions can make aplastic anemia worse. For example, diabetes, heart disease, and chronic infections can make treatment harder and affect survival chances. A patient with diabetes might face a higher risk of getting infections while on immunosuppressive therapy.
The table below shows how different pre-existing conditions can affect aplastic anemia outcomes:
| Pre-existing Condition | Impact on Aplastic Anemia Prognosis |
| Diabetes | Increased risk of infections during treatment |
| Heart Disease | Potential for cardiovascular complications |
| Chronic Infections | Increased risk of sepsis and other infections |
Management of Complications During Treatment
Managing complications well is key to better survival rates in aplastic anemia patients. This means proactive monitoring for infections, keeping blood counts in check, and adjusting treatment plans when needed.
For instance, patients on immunosuppressive therapy might need prophylactic antibiotics to avoid infections. Also, regular blood count checks can spot problems early, allowing for quick action.
Understanding comorbidities and using good management strategies can help healthcare providers get better results for adults with aplastic anemia.
Key Factors 6 and 7: Clonal Evolution and Supportive Care
Clonal evolution and supportive care are key in treating adults with aplastic anemia. They are closely linked to managing the disease and its outcome.
Risk of Progression to MDS or Leukemia
The risk of developing myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) is a big worry. Studies show that aplastic anemia patients face a higher risk. Regular checks and quick action are vital to lower this risk.
The reasons behind clonal evolution in aplastic anemia are complex. It involves genetics and the environment. Knowing these factors helps in finding ways to stop or slow down the disease’s progression.
Role of Transfusion Support and Growth Factors
Supportive care, like transfusions and growth factors, is very important. Transfusions help manage symptoms like anemia and low blood counts. This improves patients’ lives. Using blood products wisely is key to avoiding bad reactions.
Growth factors, like G-CSF, help make more blood cells. This can lower the chance of infections. But it’s important to weigh the benefits against the risks.
Quality of Life Considerations in Long-term Survivors
For those who survive aplastic anemia long-term, quality of life is very important. The disease and its treatment can deeply affect physical, emotional, and social health. Comprehensive care is needed to improve outcomes.
Survivors might deal with chronic tiredness, more infections, and treatment side effects. A team of doctors, including hematologists and supportive care experts, can help. They aim to improve life quality.
Conclusion: Future Directions in Aplastic Anemia Management and Prognosis
Aplastic anemia is a complex condition with many factors affecting its outcome. New treatments and ongoing research bring hope for better care. In Western countries, about 2 people per million get AA each year, showing the need for good management.
Immunosuppressive therapy and hematopoietic stem cell transplantation are the main treatments. Researchers are also looking at adding eltrombopag to these treatments.
Future work in treating aplastic anemia will focus on making treatments better and adding new therapies. As research grows, we expect to see better results for patients. This will help us understand what affects their prognosis better.
We aim to improve care and support for those with aplastic anemia. This will help them live better and longer lives.
FAQ
What is aplastic anemia?
Aplastic anemia is a rare blood disorder. It happens when the bone marrow can’t make enough blood cells. This leads to a lack of all blood cell types.
What are the causes of aplastic anemia in adults?
In adults, aplastic anemia can be caused by many things. This includes some drugs, toxins, viruses, and autoimmune diseases.
How is aplastic anemia diagnosed?
Doctors use tests to find aplastic anemia. These include looking at blood, doing a bone marrow biopsy, and checking the bone marrow cells.
What are the different classifications of aplastic anemia based on disease severity?
Aplastic anemia is divided into different levels. These levels depend on blood counts and how the bone marrow looks.
What treatment approaches are available for aplastic anemia?
There are several ways to treat aplastic anemia. These include medicines to stop the immune system, stem cell transplants, and supportive care like blood transfusions.
How does age affect the prognosis of aplastic anemia?
Age is very important in treating aplastic anemia. People under 40 usually do better than those older.
What is the significance of the response to immunosuppressive therapy in aplastic anemia?
How well a person responds to treatment is very important. Those who respond early tend to do better than those who don’t.
What are the outcomes of stem cell transplantation in aplastic anemia?
The success of stem cell transplants varies. The best results usually come from using a matched sibling donor.
How do comorbidities influence the prognosis of aplastic anemia?
Other health problems can make treatment harder. They can also affect how well a person does in the long run.
What is the risk of clonal evolution in aplastic anemia?
People with aplastic anemia might develop other blood disorders. This includes myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML).
What is the role of supportive care in aplastic anemia?
Supportive care is very important. It includes transfusions and growth factors to help manage symptoms and improve life quality.
What is the prognosis for adults with aplastic anemia?
The outlook for adults with aplastic anemia varies. It depends on how severe the disease is, the person’s age, and how well they respond to treatment. Modern treatments have helped improve survival rates.
References
- Bacigalupo, A. (1994). Long-term outcome of aplastic anemia in adults treated with antithymocyte globulin: Clinical predictors of survival. Blood, 84(11), 4188-4195. https://pubmed.ncbi.nlm.nih.gov/7803802/





