Induction chemotherapy AML is the first and most critical step in treating Acute Myeloid Leukemia (AML). This phase aims to destroy leukemia cells in the blood and bone marrow, helping patients reach complete remission.
One of the most common induction treatments is the 7+3 chemotherapy regimen, which combines cytarabine and an anthracycline. This approach has been proven effective in helping many patients recover and move to the next phase of therapy — consolidation.
At Liv Hospital, we are committed to improving outcomes for AML patients through advanced treatment methods and personalized care. Our expert team offers full support throughout each stage of AML therapy, ensuring the best possible experience for every patient.
Key Takeaways
- The 7+3 chemotherapy regimen is a widely used treatment for AML.
- Remission induction and consolidation are the two main phases of AML treatment.
- Liv Hospital provides quality-driven protocols and patient-centered care.
- The 7+3 regimen combines cytarabine and an anthracycline.
- Effective treatment of AML requires immediate and thorough care.
Understanding Acute Myeloid Leukemia (AML)

Acute Myeloid Leukemia (AML) is a serious condition. It happens when abnormal white blood cells grow fast in the bone marrow. This stops normal blood cells from being made, causing health problems.
What is AML and How Does It Develop?
AML is a blood cancer that starts in the bone marrow and quickly spreads to the blood. It can also go to other parts of the body, like the lymph nodes and liver. It’s caused by genetic changes in bone marrow cells, often due to various factors.
These genetic changes make abnormal cells grow without control. They take over the bone marrow, leaving not enough room for healthy cells. This leads to anemia, infections, and bleeding problems.
Risk Factors and Prevalence in the United States
Several things can increase your risk of getting AML. These include age, genetic factors, exposure to certain chemicals, and past chemotherapy or radiation. Most AML cases happen in people over 65.
In the U.S., AML is rare, making up about 1% of all cancers. Yet, it’s a common leukemia in adults. Every year, around 20,000 new AML cases are diagnosed in the U.S.
Why Immediate Treatment is Critical
Getting treatment right away is key for AML. The disease can get worse fast if not treated. The goal is to get rid of the leukemia cells and let the bone marrow make normal blood cells again.
If AML isn’t treated quickly, it can cause serious problems. These include infections, organ failure, and even death. So, it’s important to know about the need for immediate treatment and the options available.
The Basics of Induction Chemotherapy for AML
Patients with AML start with a tough treatment phase called induction chemotherapy. It’s the first and most intense part of treatment. The goal is to get rid of leukemia cells fast, as AML grows quickly.
What Defines Induction Therapy in Leukemia Treatment
Induction therapy is very intense. It aims to get rid of leukemia cells from the bone marrow and blood. The 7+3 regimen, a mix of cytarabine and an anthracycline, is often used for AML patients.
“The main aim of induction chemotherapy is to get to complete remission,” says a top hematologist. “This means no leukemia cells in the bone marrow or blood, and normal blood production.”
Primary Goals of AML Induction Treatment
The main goal of induction chemotherapy is to reach complete remission (CR). This means no leukemia cells in the bone marrow or blood. Getting to CR is key for better survival and quality of life for AML patients.
- Eliminate leukemia cells from the bone marrow and blood
- Restore normal hematopoiesis
- Improve patient outcomes and survival rates
How Complete Remission is Defined and Measured
Complete remission is clear by certain rules. These include no leukemia cells in the bone marrow, normal blood counts, and no leukemia outside the bone marrow. Doctors use bone marrow biopsies and blood tests to check how well the treatment is working.
| Criteria | Description |
| Bone Marrow Blast Percentage | Less than 5% |
| Peripheral Blood Counts | Normalization of neutrophil and platelet counts |
| Extramedullary Disease | Absence of leukemia outside the bone marrow |
A recent study found, “Getting to complete remission is a big win in AML treatment. It gives patients a chance at long-term survival and even a cure.”
Anatomy of the 7+3 AML Protocol
Knowing the 7+3 AML protocol is key for doctors and patients dealing with AML. This treatment mix of cytarabine and anthracyclines is a mainstay in fighting Acute Myeloid Leukemia.
Historical Development of the Standard Regimen
The 7+3 protocol started as an effort to standardize AML treatment. Developed decades ago, it has grown through trials and studies to become a widely accepted standard today.
Its history includes:
- Early trials showing its success
- Improvements in how it’s given
- Studies comparing it to other treatments
Cytarabine: The “7” Component Explained
Cytarabine is a critical part of the 7+3 regimen, given for 7 days straight. It stops leukemia cells from growing by messing with DNA synthesis.
The “7” in 7+3 means 7 days of cytarabine, usually 100-200 mg/m². This long time helps it work best against leukemia.
Anthracyclines: Understanding the “3” Component
Anthracyclines, like daunorubicin or idarubicin, are given for the first 3 days. They break DNA strands, causing leukemia cells to die.
The type and dose of anthracycline can change based on the patient and where they get treated. Common doses include:
- Daunorubicin at 45-60 mg/m² for 3 days
- Idarubicin at 12 mg/m² for 3 days
Understanding cytarabine and anthracyclines helps doctors tailor the 7+3 protocol for each patient. This makes the treatment more effective and easier to handle.
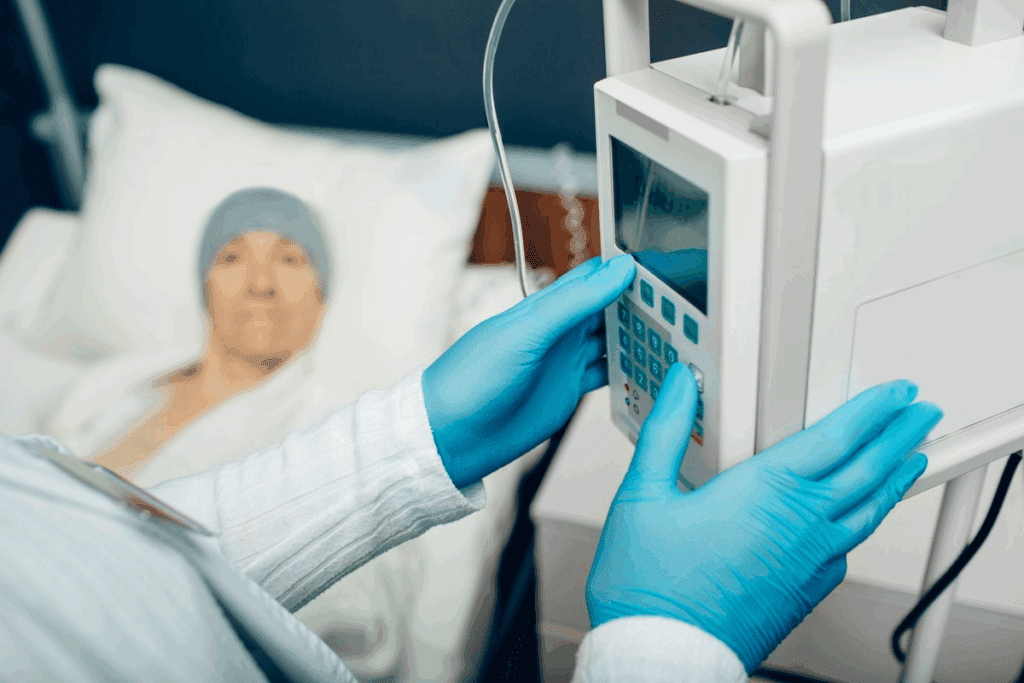
What to Expect During 7+3 Chemotherapy
The 7+3 chemotherapy regimen is a key part of AML treatment. Knowing what to expect can help reduce anxiety. We aim to give you a detailed overview to prepare you for what’s ahead.
Pre-Treatment Evaluation and Preparation
Before starting 7+3 chemotherapy, patients get a thorough check-up. This includes blood tests, bone marrow biopsies, and heart and kidney checks. These tests make sure everything is working right before treatment starts.
Preparation is key to managing side effects and challenges. Patients are advised to:
- Maintain good oral hygiene to prevent infections
- Follow a nutritious diet to support their immune system
- Stay hydrated to help their body recover
- Arrange for support at home, as the treatment can impact their ability to perform daily tasks
The Hospital Stay: Typical Duration and Environment
Patients usually need to stay in the hospital during the induction phase. This is because of the risk of severe side effects like neutropenia and infections. The hospital stay allows for close monitoring and quick action if problems arise.
The hospital stay can last from 3 to 4 weeks. During this time, patients are in a safe environment to reduce infection risk. The hospital staff provides supportive care, including:
| Supportive Care Measure | Purpose |
| Blood transfusions | To manage anemia and low platelet counts |
| Antibiotics | To prevent or treat infections |
| Nutritional support | To ensure adequate nutrition despite mucositis or other eating difficulties |
Daily Monitoring and Supportive Care
Daily monitoring is key during 7+3 chemotherapy. Healthcare providers watch for signs of infection, bleeding, and other complications. They adjust the treatment plan as needed. Supportive care is tailored to the individual’s needs, addressing side effects like nausea, fatigue, and mucositis.
“The care and support received during my 7+3 chemotherapy were exceptional. The medical team’s attentiveness made a significant difference in my treatment journey.” – A patient testimonial
By understanding what to expect during 7+3 chemotherapy, patients can better prepare themselves for the challenges and milestones ahead. Our goal is to provide complete support and guidance throughout this critical phase of AML treatment.
Effectiveness of the 7+3 Regimen in AML Treatment
The 7+3 chemotherapy regimen is key in treating Acute Myeloid Leukemia (AML). It leads to high complete remission rates. We look at how well it works for different ages and its effect on survival over time.
Complete Remission Rates Across Age Groups
The 7+3 regimen works best for younger patients. Research shows that those under a certain age do better with this treatment.
Age plays a big role in how well the 7+3 regimen works.
Predictors of Treatment Response
Several things can predict how well a patient will do with the 7+3 regimen:
- Genetic Mutations: Some genetic changes can impact treatment response.
- Overall Health: Patients in better health tend to do better.
- Initial Response: How well a patient responds to the first treatment is key to long-term survival.
Long-term Survival Statistics and Trends
Survival rates for AML patients treated with the 7+3 regimen vary:
- Younger patients who achieve complete remission have a higher chance of long-term survival. Some studies show 5-year survival rates up to 40%.
- Older patients face challenges with long-term survival. But, better supportive care has helped improve outcomes.
The 7+3 regimen is a vital part of AML treatment. Its success is seen in complete remission rates and long-term survival. Knowing what predicts treatment response helps tailor therapy to each patient’s needs.
Managing Side Effects of 7+3 Chemotherapy
Managing side effects is key for comfort and success in 7+3 chemotherapy. This treatment is good against Acute Myeloid Leukemia (AML). But, it can cause side effects that affect a patient’s life quality.
Immediate Side Effects and Their Management
Patients on 7+3 chemotherapy face side effects like nausea, vomiting, fatigue, and infection risk. Supportive care strategies are vital to lessen these effects.
- Nausea and Vomiting: Antiemetic meds help prevent and treat nausea and vomiting.
- Fatigue: Rest, nutrition, and energy-boosting meds help manage fatigue.
- Infection Risk: Using prophylactic antibiotics and monitoring closely helps manage infection risk.
Long-term Complications to Consider
7+3 chemotherapy is key for AML treatment but has long-term risks. These include:
- Cardiac Toxicity: Anthracyclines in the regimen can harm the heart. It’s important to check heart function before, during, and after treatment.
- Secondary Malignancies: There’s a small chance of getting secondary cancers from the treatment. Long-term follow-up is needed to catch any early.
Supportive Care Strategies During Treatment
Supportive care is essential for managing side effects during 7+3 chemotherapy. This includes:
| Supportive Care Measure | Description |
| Nutritional Support | Ensuring enough nutrition to keep strength up and aid recovery. |
| Hydration | Keeping hydrated to avoid dehydration and support health. |
| Emotional Support | Offering psychological support through counseling, support groups, and family support. |
By using these supportive care strategies, we can greatly improve the treatment experience for patients on 7+3 chemotherapy.
Advancements in Induction Chemotherapy for AML
The treatment for Acute Myeloid Leukemia (AML) is changing fast. This is thanks to new research and better ways to do induction chemotherapy. We’re finding new ways to make the 7+3 protocol better.
Evolution of the Standard 7+3 Protocol
The 7+3 regimen is a key part of AML treatment. It’s been updated to be more effective and safer. Scientists are looking at new anthracyclines and better dosing to cut down on side effects. They want to help more patients get into complete remission and live longer.
Adding new drugs to the 7+3 mix is another area of focus. Mixing old drugs with new ones might help beat resistance. This could lead to better results for patients.
Dose Intensification Strategies
Increasing the doses of chemotherapy is a promising idea. By using more of the key drugs, doctors hope to get better results. But, they also worry about more side effects.
Researchers are working to find the best doses and who will benefit most. They’re also looking at ways to reduce side effects from higher doses.
Risk-Adapted Approaches to Induction
Using treatments based on how high the risk is is becoming more common. By looking at genetic and molecular details, doctors can choose the right treatment for each patient.
This way, treatments can be more effective and safer. As we learn more about AML, this approach will likely become even more important.
Targeted Therapies Enhancing the 7+3 AML Protocol
Targeted therapies are changing how we treat Acute Myeloid Leukemia (AML). They are making the 7+3 chemotherapy protocol better. This shift is improving patient results.
FLT3 Inhibitors: Midostaurin and Crenolanib
FLT3 inhibitors are a new hope for AML treatment. Midostaurin was the first approved FLT3 inhibitor. It has greatly improved survival for patients with FLT3 mutations. Crenolanib is also being tested for better results.
Using FLT3 inhibitors with the 7+3 protocol is a big step forward. It’s a big help for patients with FLT3 mutations.
Venetoclax Plus 7+3 Combination Therapy
Venetoclax is a BCL-2 inhibitor that works well with the 7+3 regimen. It has boosted response rates and survival for AML patients. Adding venetoclax to the 7+3 protocol is a big win for treatment.
More studies are needed to confirm venetoclax’s benefits. But early results look very promising.
Other Emerging Targeted Approaches
Other targeted therapies are also being developed. They target different genetic mutations and pathways in AML. These new approaches aim to keep improving treatment results for AML patients.
As we learn more about AML, new targeted therapies will be key. They will shape the future of AML treatment.
Alternative Options for Ineligible Patients
Not all AML patients can handle intensive induction. There are other ways to treat Acute Myeloid Leukemia. Each patient is different, so what works for one might not work for another.
Determining Eligibility for Intensive Induction
Who can get intensive induction chemotherapy depends on several things. These include the patient’s health, age, and AML type. We look at these carefully to choose the best treatment.
Age is not the only thing that matters. It’s the patient’s overall health and fitness that counts.
Hypomethylating Agents as Alternative Therapy
Hypomethylating agents like azacitidine and decitabine are options for those who can’t have intensive treatment. They change DNA in cancer cells, helping control AML. Research shows they can increase survival chances for some patients.
Low-Intensity Regimens and Their Outcomes
For those who can’t handle strong chemotherapy, low-intensity regimens are available. These treatments are less aggressive but can help manage AML. Results depend on the patient’s condition and how well they respond.
| Treatment Regimen | Patient Group | Outcome |
| Hypomethylating Agents | Elderly or unfit patients | Improved survival rates |
| Low-Intensity Chemotherapy | Patients with comorbidities | Managed AML progression |
Clinical Trial Opportunities
Clinical trials can offer new treatments for some patients. We suggest eligible patients consider these trials. Clinical trials can provide insights into new treatments and may offer better outcomes.
The Post-Induction Treatment Journey
After getting rid of leukemia with induction chemotherapy, the next step is the post-induction treatment. This phase aims to kill any leftover leukemia cells. This helps lower the chance of the disease coming back.
Consolidation Therapy Approaches
Consolidation therapy is key in the post-induction phase. It’s designed to cut down leukemia cells even more. High-dose cytarabine is often used for this in AML patients who have reached complete remission. The treatment plan depends on the patient’s age, health, and leukemia type.
- Cytarabine-based regimens are standard for consolidation therapy.
- The number of consolidation cycles can vary based on patient response and tolerance.
- Some patients may be candidates for clinical trials involving new consolidation strategies.
Role of Stem Cell Transplantation
Stem cell transplantation can be a cure for many AML patients, mainly those with high-risk disease. Allogeneic stem cell transplantation, where stem cells come from a donor, can fight off leftover leukemia cells.
We think about stem cell transplantation for patients with:
- High-risk cytogenetic or molecular features.
- Relapsed or refractory disease.
- Poor response to initial induction chemotherapy.
Maintenance Strategies and Monitoring
After consolidation therapy or stem cell transplantation, it’s important to keep an eye out for any signs of relapse. Maintenance therapy, like targeted agents, helps keep the disease in remission.
Managing Relapse After 7+3 Therapy
Dealing with relapse after 7+3 therapy is tough. Options include salvage chemotherapy, targeted therapies, and clinical trials. The right treatment depends on how long the patient was in remission, their health, and previous treatments.
We stress the need for a personalized approach to relapse management. This considers the patient’s disease and health.
Conclusion: The Evolving Landscape of AML Treatment
AML treatment is changing fast. The AML treatment evolution is fueled by new research. This includes better induction chemotherapy, targeted therapies, and care after treatment.
We’re moving towards treatments that are more tailored to each patient. This means using existing treatments better and finding new ones. For example, adding FLT3 inhibitors and venetoclax to the standard 7+3 chemotherapy is a big step forward.
Looking ahead, we expect even better results for AML patients. Thanks to ongoing research and teamwork, we’re on the verge of major breakthroughs. This will greatly improve care and support for patients everywhere.
FAQ
What is the 7+3 chemotherapy regimen used for?
The 7+3 chemotherapy regimen is a common treatment for Acute Myeloid Leukemia (AML). It combines cytarabine and an anthracycline to help patients achieve complete remission.
How does the 7+3 regimen work?
This regimen works by giving cytarabine for 7 days and an anthracycline for 3 days. It aims to kill leukemia cells in the bone marrow, aiming for complete remission.
What are the primary goals of AML induction treatment?
The main goals of AML induction treatment are to remove leukemia cells and restore normal bone marrow. It also aims to improve long-term survival rates.
What is complete remission in AML, and how is it measured?
Complete remission in AML means no leukemia cells in the bone marrow or blood, with normal bone marrow function. It’s checked through bone marrow biopsies, blood counts, and other tests.
What are the common side effects of 7+3 chemotherapy?
Common side effects include nausea, vomiting, fatigue, hair loss, and a higher risk of infections. This is due to low blood counts.
How are side effects of 7+3 chemotherapy managed?
Side effects are managed with supportive care. This includes anti-nausea meds, antibiotics, blood transfusions, and nutritional support. It helps keep patients comfortable and ensures they stick with treatment.
Are there alternative treatments for patients ineligible for intensive induction chemotherapy?
Yes, there are alternatives. Hypomethylating agents and low-intensity regimens are options for those not eligible for intensive chemotherapy.
What is the role of consolidation therapy after achieving complete remission?
Consolidation therapy aims to get rid of any remaining leukemia cells after complete remission. It reduces the risk of relapse and improves survival chances.
How does stem cell transplantation fit into the post-induction treatment journey?
Stem cell transplantation is key for some patients after induction. It replaces damaged bone marrow with healthy stem cells, aiming to cure AML.
What advancements are being made in AML treatment?
New advancements include combining targeted therapies with the 7+3 regimen. There are also dose intensification strategies and risk-adapted approaches. These aim to improve treatment outcomes and offer new options for AML patients.
What are FLT3 inhibitors, and how are they used in AML treatment?
FLT3 inhibitors, like midostaurin and crenolanib, are targeted therapies. They are used with the 7+3 regimen to improve outcomes for AML patients with specific genetic mutations.
What is venetoclax, and how is it used in AML treatment?
Venetoclax is a targeted therapy used with the 7+3 regimen or alone for AML patients. It’s a good option for older patients or those with comorbidities.
References:
- Othus, M., Tallman, M. S., & Walter, R. B. (2022). Improved outcomes with “7+3” induction chemotherapy for acute myeloid leukemia. Clinical Leukemia, 16(2), e198-e205. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9827148/


































