Last Updated on November 20, 2025 by Ugurkan Demir

Getting a diagnosis of acute myeloid leukemia in kids can be scary. But, thanks to new treatments, survival rates have gone up. Studies show that the 5-year survival rate for childhood AML is now 65-75%.
This improvement comes from better chemotherapy, stem cell transplants, and treatments that match each child’s needs.
Thanks to hard work in research, we now have more effective treatments. Knowing about childhood leukemia survival rates is key for families and doctors. The next parts will share seven important facts about childhood acute myeloid leukemia survival rate. We’ll look at the newest treatments and care options.
Key Takeaways
- Advances in chemotherapy have improved treatment outcomes.
- Stem cell transplantation has become a key treatment.
- Risk-adapted approaches tailor treatment to individual patient needs.
- The overall 5-year survival rate for childhood AML is 65-75%.
- Liv Hospital offers expert, patient-focused care for pediatric leukemia.
- Families get the latest and most effective treatments.
The Current State of Childhood Acute Myeloid Leukemia Survival Rate

Childhood AML survival rates have improved a lot. This is thanks to better medical treatments and care. Doctors and researchers are working hard to make treatments better for kids.
Overall 5-Year Survival Rates of 65-75%
The 5-year survival rate for kids with AML is now 65-75%. This is a big jump from before.
Back in the 1990s, the survival rate was around 40%. Now, it’s 65-75%. This shows how far we’ve come in treating AML with better chemotherapy, stem cell transplants, and care.
| Time Period | 5-Year Survival Rate |
| 1990s | 40% |
| Current | 65-75% |
Historical Improvement in Outcomes
Many things have helped kids with AML live longer. Better chemotherapy, stem cell transplants, and care have all played a part.
These changes have helped doctors understand AML better. They can now treat it more effectively. So, kids with AML have a better chance of surviving.
The ongoing rise in AML survival rates shows we need to keep researching. We must keep working on better treatments for kids.
Key Fact #1: How Age Affects AML Prognosis in Children
The outlook for kids with Acute Myeloid Leukemia (AML) changes a lot with age. Studies show that babies under one year old have much lower survival rates than older kids.
Infant vs. Older Child Survival Differences
Babies with AML, like those under 12 months, face big challenges. Their survival rates are often below 25% in some areas. Older kids usually do better because their treatments are more effective and tailored to their needs.
The big difference in survival rates between babies and older kids comes from several things. These include:
- Biological differences in the leukemia cells
- How well they respond to treatment
- How well they can handle strong treatments
Age-Specific Treatment Considerations
Treatment for AML in kids depends on their age. This is because the disease acts differently in different age groups. For babies, treatments are made to be less harsh but effective, considering their delicate bodies.
Some important things to think about for age-specific treatments are:
- Modified chemotherapy for babies
- Watching closely how well the treatment works and how it affects them
- New ways, like targeted therapies
Knowing these age-specific details is key to bettering outcomes for kids with AML. By customizing treatments, doctors can aim for higher survival rates and better lives for these children.
Key Fact #2: Genetic Subtypes and Their Impact on Survival
Childhood AML is not just one disease. Its outlook changes a lot based on the genetic subtypes. New genetic analysis tools help doctors sort AML into different types based on mutations.
Knowing the genetic subtypes is key to understanding the disease. It helps doctors plan better treatments. Some subtypes have better cure rates, while others are harder to treat.
Lower-Risk Gene Subtypes with 70-80% Cure Rates
Some AML subtypes in kids can be cured with just chemotherapy. For example, kids with the AML1-ETO gene have cure rates over 70-80% with the right treatment.
“The presence of certain genetic abnormalities, such as the t(8;21) or inv(16), confers a more favorable prognosis in pediatric AML patients, with cure rates significantly higher than the average.” As noted by pediatric hematology-oncology specialists.
| Genetic Subtype | Cure Rate | Treatment Approach |
| t(8;21) | 70-80% | Chemotherapy |
| inv(16) | 70-80% | Chemotherapy |
| Complex Karyotype | 20-40% | Intensive Chemotherapy and SCT |
High-Risk Genetic Markers
On the other hand, some genetic markers mean a tougher fight. Kids with complex karyotypes or FLT3-ITD mutations face lower survival chances. They might need stronger treatments, like stem cell transplants.
Genetic testing is vital for finding these subtypes early. It helps doctors tailor treatments for each child. This approach is changing how we treat childhood AML, bringing new hope for better outcomes.
Key Fact #3: Treatment Advances Driving Improved Outcomes
The way we treat childhood AML has changed a lot. New treatments are giving kids a better chance of beating the disease. Studies show these new methods are working well for kids with AML.
Modern Chemotherapy Protocols
Today’s chemotherapy is more advanced. It combines strong induction and consolidation phases. This approach is designed to work better and cause fewer side effects.
Intensive induction chemotherapy is really helping kids get into remission. The use of cytarabine and anthracyclines is key. Researchers are now looking at how to make these treatments even better.
Stem Cell Transplantation Innovations
Stem cell transplants are now a big part of treating AML in kids. They’re very important for kids with high-risk disease or who have had AML before. New ways of doing transplants are making them safer and more effective.
Haploidentical donors are also helping more kids get transplants. This is good news for those without a matched donor.
Risk-Adapted Treatment Approaches
Doctors are now tailoring treatments to each child’s risk level. This means giving the right amount of treatment to avoid too much harm. It’s all about finding the best balance.
They look at the leukemia’s genes and molecules to decide how to treat each child. Minimal residual disease (MRD) assessment helps them see how well the treatment is working. This way, they can adjust the treatment as needed.
With these new approaches, doctors can give kids with AML more personalized care. This is leading to better survival rates and a better quality of life for these young patients.
Key Fact #4: Comparing AML to ALL in Pediatric Patients
Pediatric AML and ALL have different survival rates. This is because of their unique biology. Knowing these differences helps in creating better treatments and improving patient care.
ALL’s Superior 85-90% Survival Rate
Acute Lymphoblastic Leukemia (ALL) has a much higher survival rate than AML. Children with ALL have a 5-year survival rate of 85% to 90%. This is thanks to better treatments and how well ALL cells react to chemotherapy.
B-Cell ALL’s Excellent Prognosis Exceeding 90%
B-cell ALL, a type of ALL, has a great prognosis. Its survival rate often goes over 90%. This high success rate is because of how well B-cell ALL responds to new treatments and targeted therapies.
Biological Differences Explaining Outcome Disparities
The survival rate difference between AML and ALL comes from their biological characteristics. ALL is more sensitive to chemotherapy. AML, on the other hand, is harder to treat and needs stronger therapies.
Also, AML and ALL have different genetic and molecular profiles. These differences affect how they behave and react to treatments. Understanding these helps in creating targeted therapies to improve outcomes for both AML and ALL.
Key Fact #5: Special Challenges of Infant Leukemia
Infant leukemia faces unique challenges that impact treatment success. Infants with leukemia have lower survival rates compared to older children. This is true in some regions, with event-free survival at 3 years below 25%. We will look into why this is and what makes infant leukemia different.
Survival Rates Below 25% in Some Regions
The survival rate for infants with Acute Myeloid Leukemia (AML) is much lower than for older kids. Studies show that the event-free survival rate at 3 years can be below 25% in some areas. This gap is due to several reasons, including different treatments and access to care.
| Region | Event-Free Survival Rate at 3 Years |
| Developed Countries | 20-25% |
| Developing Countries | <15% |
Unique Biological Features of Infant AML
Infant AML has distinct biological features compared to AML in older kids. These include mixed lineage leukemia (MLL) gene rearrangements, which are more common in infant AML and linked to a worse prognosis. Knowing these differences is key to creating targeted therapies.
Specialized Treatment Protocols
Because of the unique challenges and biological features of infant AML, special treatment plans have been made. These plans often include intensive chemotherapy regimens and sometimes hematopoietic stem cell transplantation. Researchers are working to improve these plans to better help infants with AML.
Research into targeted therapies based on infant AML’s molecular characteristics is promising. By studying the disease’s genetic and molecular makeup, scientists can create more effective and less harmful treatments.
Key Fact #6: Regional and Socioeconomic Factors Affecting Survival
Regional and socioeconomic factors greatly impact the survival rates of children with Acute Myeloid Leukemia (AML). These factors lead to big differences in healthcare results across various groups.
Developed vs. Developing Countries
Research shows big gaps in childhood leukemia survival rates between rich and poor countries. In wealthy nations, better healthcare and new treatments have raised survival chances. For example, a study in the Journal of Clinical Oncology found U.S. kids with AML have a 5-year survival rate of 65-75%.
In contrast, poor countries struggle with limited healthcare, a lack of specialized care, and outdated treatments. This results in lower survival rates.
Regional disparities in healthcare access and quality are key reasons for these gaps. In low-income countries, the lack of resources and infrastructure makes it hard to provide effective cancer care. The World Health Organization (WHO) reports that in some low-income countries, leukemia survival rates for kids can be as low as 10-20%.
Access to Specialized Pediatric Cancer Centers
Having access to specialized pediatric cancer centers is vital for survival. These centers offer teams of experts, advanced diagnostic tools, and new treatments. Kids treated here often live longer than those in general hospitals.
But not all areas have these centers. In many places, families must travel far or get care in bad facilities. This delays diagnosis and treatment, showing the need for better global healthcare and more support for cancer care in poor areas.
Working to fix these regional and socioeconomic gaps is key to better outcomes for kids with AML worldwide. We need to improve healthcare, make sure kids get to specialized centers, and fund research for new treatments. These steps are important for fair survival rates everywhere.
Key Fact #7: Long-Term Survival and Quality of Life
More kids are beating AML, which highlights the need to focus on their long-term health. As treatments get better, it’s key to understand and tackle the lasting effects of AML treatment.
Late Effects of Treatment
Survivors of childhood AML often deal with lasting side effects. These can affect their body, mind, and spirit. Some common issues include:
- Cardiac issues from certain chemo drugs
- Problems with learning and memory
- Emotional and psychological challenges like anxiety and depression
- Higher risk of getting other cancers
It’s vital to monitor and manage these effects to help survivors live well. Regular check-ups are key to catching and treating problems early.
Monitoring and Follow-up Protocols
Good monitoring and follow-up plans are essential for AML survivors. These plans usually include:
- Regular visits to healthcare providers
- Tests for heart health and other late effects
- Checks on cognitive function
With these plans, doctors can offer the right support and care to improve survivors’ lives.
Survivorship Programs
Survivorship programs are vital for AML survivors. They offer:
- Resources and support services
- Info on managing late effects and staying healthy
- Chances to connect with others who’ve gone through similar things
These programs help meet the unique needs of AML survivors, boosting their long-term health and happiness.
Understanding the Diagnosis Process for Childhood AML
Getting a childhood AML diagnosis is key to effective treatment. Diagnosing AML in kids involves several tests to confirm the disease and its type.
The first step is checking symptoms, which can be like other illnesses. Symptoms include fatigue, pale skin, and frequent infections. A detailed medical history and physical check are vital to spot any signs of leukemia.
Initial Symptoms and Evaluation
AML symptoms in kids can vary. Some might have bone or joint pain, while others might have big lymph nodes or a spleen. A complete blood count (CBC) is often the first test, showing blood cell count issues.
If the CBC shows leukemia, more tests are done to confirm and classify the AML. These tests help decide the best treatment.
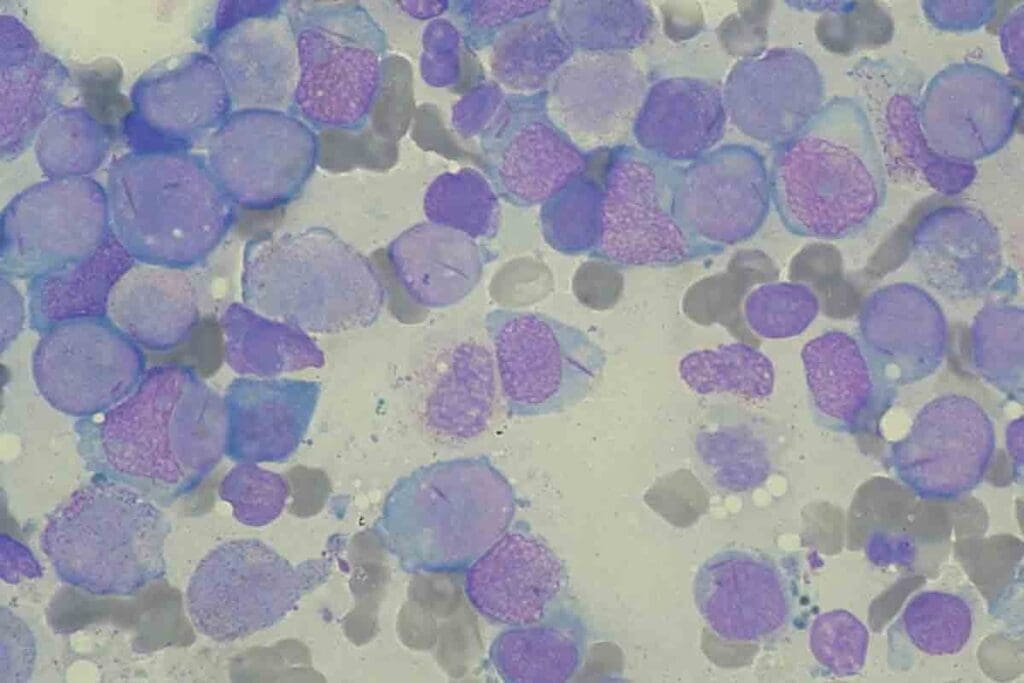
Diagnostic Tests and Classification
Tests for AML include bone marrow aspiration and biopsy, immunophenotyping, and genetic testing. Bone marrow tests remove a sample for examination. Immunophenotyping identifies the cell type, and genetic testing finds chromosomal issues.
The type of AML is determined by these tests. The French-American-British (FAB) classification and the World Health Organization (WHO) classification sort AML into subtypes based on cell and genetic features.
Accurate AML diagnosis and classification are vital for treatment planning. They help tailor treatments to meet each child’s needs.
Emerging Therapies Shaping the Future of Childhood AML Treatment
New treatments are changing how we fight childhood AML. These new methods come from ongoing research and tech advances.
Targeted Molecular Therapies
These therapies aim at the genetic roots of AML. They try to protect healthy cells, cutting down side effects and boosting life quality.
- FLT3 inhibitors: These drugs target the FLT3 gene mutation, common in AML patients.
- IDH1 and IDH2 inhibitors: These inhibitors target the IDH1 and IDH2 mutations, giving hope to patients with these genetic changes.
Studies show these targeted therapies are making a big difference for kids with AML. Recent research suggests, “Targeted therapies are a big step up in treating childhood AML. They offer more precise and possibly less harmful treatment options.”
“The development of targeted therapies is a key step forward in AML treatment. It opens up new ways to better patient outcomes.”
-Pediatric oncologists highlight.
Immunotherapy Approaches
Immunotherapy is another promising area in AML treatment. It uses the body’s immune system to fight cancer.
- CAR-T cell therapy: This method genetically modifies T cells to attack cancer cells.
- Monoclonal antibodies: These target specific proteins on cancer cells, marking them for the immune system to destroy.
Immunotherapy is a hopeful treatment for AML, even for those who have tried other treatments without success.
Precision Medicine Initiatives
Precision medicine is also key in AML treatment. It tailors treatment to each patient’s genetic makeup, aiming for better results and less harm.
- Genetic profiling: Advanced genetic testing finds the specific mutations causing the leukemia.
- Personalized treatment plans: Treatment is customized based on the patient’s AML genetic profile.
As research keeps moving forward, these new therapies will likely greatly improve AML treatment for kids.
Supporting Families Through the AML Treatment Journey
Families of children with Acute Myeloid Leukemia (AML) face a tough journey. The diagnosis is hard to take, and treatment is complex and emotionally tough.
It’s key to support families in all ways. This helps them deal with the diagnosis better.
Psychological Impact and Support Resources
The emotional impact of AML on families is huge. Every family member feels the strain of a child’s life-threatening illness.
“The emotional toll of a cancer diagnosis on families is profound, and it’s vital that we provide them with the support they need to cope.”
-As noted by a pediatric oncologist
Support resources are essential for managing stress and anxiety. They include:
- Counseling services for family members
- Support groups for parents of children with cancer
- Mental health professionals specializing in pediatric oncology
Navigating Treatment Decisions
Choosing a treatment for a child with AML is overwhelming. The disease’s complexity and treatment options need careful thought and guidance.
Families need help understanding the diagnosis and treatment plans. A team of healthcare professionals can offer this support.
| Support Mechanism | Description | Benefit |
| Multidisciplinary Team | A team of healthcare professionals providing complete care | Coordinated care and informed decision-making |
| Family Counseling | Counseling services for family members to cope with the diagnosis | Emotional support and resilience |
Financial Considerations
The cost of AML treatment is high. It includes hospital stays, medications, and travel. Families need help managing these costs.
Financial assistance programs can help. They include government programs, non-profit organizations, and hospital-based financial aid.
By giving families full support during AML treatment, we can improve their well-being. This helps them cope with the challenges they face.
Conclusion: Hope and Progress in Childhood AML Treatment
Childhood Acute Myeloid Leukemia (AML) treatment has made big strides in recent years. This brings new hope for better outcomes and survival rates. Despite its challenges, research and new treatments are pushing forward in AML care for kids.
Genetic profiling has led to more accurate risk assessments. This allows for treatments that are more tailored to each child. New molecular and immunotherapy options are also being developed to fight AML.
The outlook for AML care is bright, thanks to ongoing research. We’re learning more about the disease and finding new treatments. As treatments get better, we expect to see kids with AML living longer and better lives.
But hope in AML treatment isn’t just about medicine. Support for families going through treatment is key too. It’s important to have access to specialized care, psychological help, and financial aid.
FAQ
What is the current 5-year survival rate for childhood Acute Myeloid Leukemia (AML)?
The current 5-year survival rate for childhood AML is around 65-75%.
How does age affect the prognosis of AML in children?
Age is a big factor in AML prognosis in children. Infants usually have a worse outlook than older kids.
What are the genetic subtypes of AML that impact survival rates?
Some genetic subtypes of AML can be cured with just chemotherapy. But, others with high-risk genes face tougher challenges.
How do treatment advances impact childhood AML survival rates?
New chemotherapy methods, stem cell transplants, and tailored treatments have greatly improved AML outcomes in kids.
What is the difference in survival rates between AML and Acute Lymphoblastic Leukemia (ALL) in pediatric patients?
ALL has a better survival rate, around 85-90%. B-cell ALL’s prognosis is even higher, over 90%.
What are the special challenges associated with infant leukemia?
Infant leukemia has unique challenges and lower survival rates. In some places, survival rates are below 25%.
How do regional and socioeconomic factors affect childhood AML survival rates?
Access to top pediatric cancer centers and economic status greatly affect survival rates. Developed countries tend to have better outcomes.
What are the late effects of AML treatment, and how are they monitored?
Late effects include health issues. There are monitoring and follow-up plans to address these. Survivorship programs also support survivors.
What is the diagnosis process for childhood AML?
The process starts with symptoms and tests. Then, it involves classifying the leukemia to decide on treatment.
What emerging therapies are shaping the future of childhood AML treatment?
New treatments like targeted therapies, immunotherapy, and precision medicine are promising for AML in kids.
How can families be supported through the AML treatment journey?
Families can get help with emotional support, making treatment choices, and dealing with financial issues.
Is childhood AML curable?
Yes, with today’s treatments, many kids with AML can be cured. But outcomes depend on individual factors.
What is the childhood AML survival rate?
The survival rate for childhood AML has risen to around 65-75% over the years.
What is the prognosis for B-cell ALL in children?
B-cell ALL has a very good prognosis, with survival rates over 90%.
How does access to specialized pediatric cancer centers impact AML survival rates?
Getting treatment at specialized pediatric cancer centers greatly boosts AML survival rates. It shows the importance of experienced care.
References
- Buechner, J., Zwaan, C. M., Pabst, T., & Creutzig, U. (2023). Pediatric Acute Myeloid Leukemia — Past, Present, and Future. Frontiers in Pediatrics, 11, Article 8837075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8837075/
- National Cancer Institute. (2025, January). Childhood Acute Myeloid Leukemia Treatment (PDQ®). https://www.cancer.gov/types/leukemia/hp/child-aml-treatment-pdq





