It’s vital for doctors to know the normal hemoglobin range for pediatrics to spot anemia early and help keep children healthy. Hemoglobin levels change significantly as kids grow.
Age-specific hemoglobin values are key for accurate diagnosis and treatment. For example, newborns have a hemoglobin range of 14–24 g/dL, infants 2–6 months old have 10–17 g/dL, and children 6–12 years old have 11.5–15.5 g/dL.
At Liv Hospital, we are dedicated to top-notch pediatric care and follow global standards. This ensures doctors have the latest information on the normal hemoglobin range for pediatrics to provide precise and effective treatment.
Key Takeaways
- Hemoglobin levels vary by age in pediatric patients.
- Newborns have a hemoglobin range of 14-24 g/dL.
- Infants aged 2-6 months have a hemoglobin range of 10-17 g/dL.
- Children aged 6-12 years have a hemoglobin range of 11.5-15.5 g/dL.
- Age-specific hemoglobin values are critical for diagnosis and treatment.
- Liv Hospital follows international standards for pediatric care.
The Critical Role of Hemoglobin Assessment in Pediatric Care

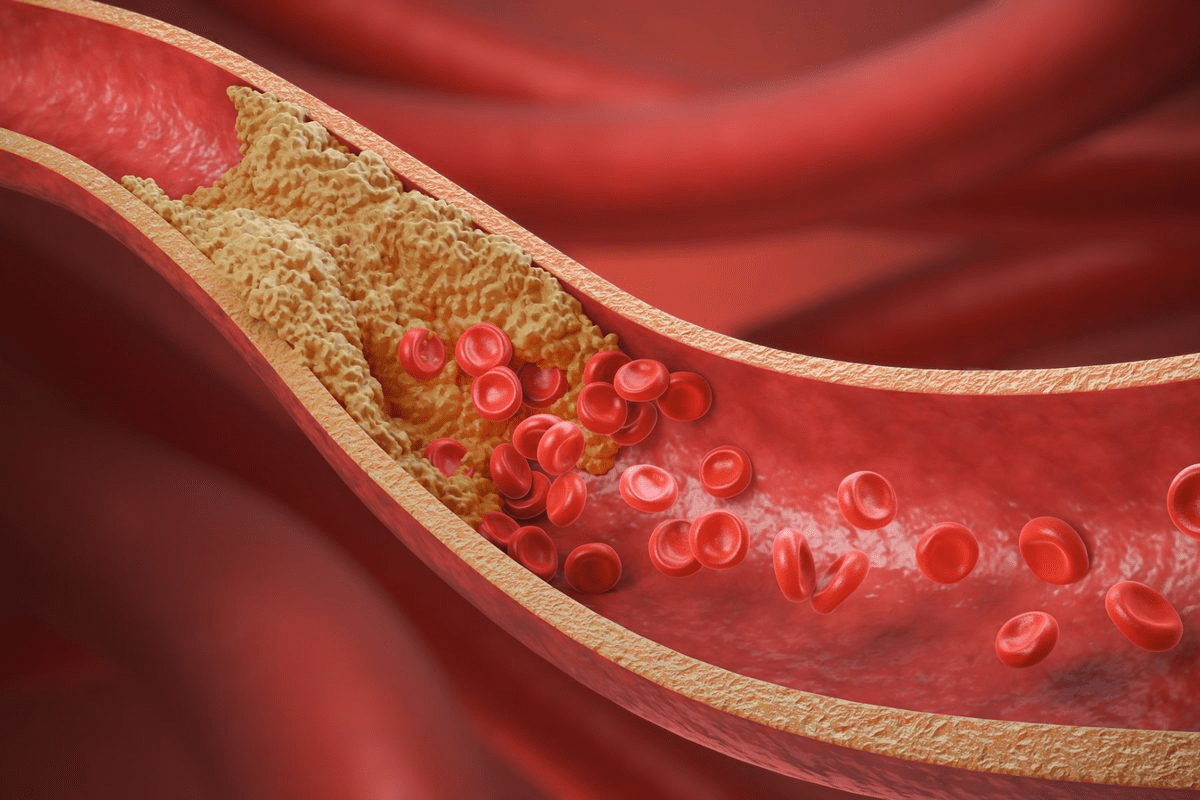
Hemoglobin assessment is key in pediatric care. It shows a child’s health status. It helps doctors find and track conditions like anemia, which affects a child’s growth and health.
Hemoglobin as a Vital Health Indicator in Children
Hemoglobin levels are important for checking a child’s health. Low levels can mean anemia, caused by poor nutrition, chronic diseases, or genetic issues. By watching hemoglobin levels, doctors can spot these problems early and start the right treatment.
Why Age-Specific Reference Ranges Are Essential
Using age-specific hemoglobin ranges is vital. Hemoglobin levels change as children grow. For example, newborns have more hemoglobin than older kids. Age-specific ranges help doctors give the right care and avoid mistakes.
| Age Group | Normal Hemoglobin Range (g/dL) |
| Newborns | 14-24 |
| Infants (2-6 months) | 10-17 |
| Children (1-5 years) | 11-14 |
Knowing these changes helps doctors give the best care and avoid wrong diagnoses.
Normal Hemoglobin Range for Pediatrics: A Complete Overview
The normal hemoglobin range for kids changes as they grow. It’s important to know these changes for each age. This helps doctors give the best care to their young patients.
Defining Normal Pediatric Hemoglobin Parameters
Hemoglobin levels in kids vary with age. At birth, they are high because of fetal hemoglobin. As kids get older, these levels change. It’s key to use age-specific ranges to check a child’s health.
Age-specific hemoglobin ranges are critical for diagnosing and treating health issues. For example, knowing the normal range for newborns, infants, and toddlers helps spot anemia or other blood disorders early.
| Age Group | Normal Hemoglobin Range (g/dL) |
| Newborns | 14-24 |
| Infants (2-6 months) | 10-17 |
| Toddlers (1-5 years) | 11-14 |
Physiological Factors Influencing Hemoglobin Levels in Children
Many factors affect hemoglobin levels in kids. One big factor is the natural drop in hemoglobin levels at 2-3 months. This is a normal part of growing up and not a sign of anemia.
Other factors include nutrition, genetics, and the environment. For instance, iron deficiency can lead to anemia in kids. Giving them the right nutrients can help manage this.
Knowing these factors and the normal ranges helps doctors give better care. They can offer specific treatments when needed.
Key Value #1: Hemoglobin Levels in Newborns (14-24 g/dL)
Newborns have hemoglobin levels between 14 to 24 g/dL. This is much higher than adults. It shows how special the needs are for newborns.
Physiological Basis for Elevated Neonatal Hemoglobin
Newborns need more oxygen because they are growing fast. Their bodies make more red blood cells and hemoglobin. This helps them get enough oxygen until they are born.
Key factors contributing to elevated neonatal hemoglobin include:
- Increased erythropoietin production
- Higher red blood cell mass
- Fetal adaptation to low oxygen environment
Clinical Implications and Monitoring Strategies
It’s important for doctors to know the normal hemoglobin range for newborns. They need to check hemoglobin levels often. This helps find problems like too much or too little hemoglobin.
Effective monitoring strategies include:
- Routine hemoglobin checks in the neonatal period
- Close observation for signs of anemia or polycythemia
- Follow-up testing as needed based on initial results and clinical presentation
Doctors can give the best care by knowing about newborn hemoglobin levels. They can make smart choices about tests and treatments.
Key Value #2: Hemoglobin Ranges in Early Infancy (10-17 g/dL)
In early infancy, hemoglobin levels usually fall between 10-17 g/dL. This is a big change from newborn levels. It’s a key time to watch how hemoglobin patterns change.
Transition from Newborn to Infant Hemoglobin Patterns
After birth, hemoglobin levels slowly drop. This drop is a natural part of growing up. It reaches its lowest point around 2-3 months. It’s important to keep an eye on this change to spot any health issues.
Monitoring Protocols for Infants 2-6 Months
For babies 2-6 months old, it’s important to check their hemoglobin often. This means:
- Regular visits to the pediatrician
- Tests to check hemoglobin levels
- Checking if they’re getting enough iron
Doctors need to watch for signs of anemia or other problems with hemoglobin. Here’s a basic plan for monitoring:
| Age | Hemoglobin Range (g/dL) | Monitoring Frequency |
| 2-3 months | 9-14 | Every 2 months |
| 4-6 months | 10-13 | Every 3 months |
Knowing the right hemoglobin ranges and how to check them helps doctors catch problems early. This way, they can help babies get better faster.
Key Value #3: The Physiologic Nadir at 2-3 Months
It’s key for doctors to know about the physiologic nadir in infants. This happens at 2-3 months, when hemoglobin levels naturally drop. It’s important to understand this to avoid mistaking it for a serious condition.
Understanding Physiologic Anemia of Infancy
Infants naturally have a drop in hemoglobin levels. This is because they switch from fetal to adult hemoglobin and their body’s red blood cell system matures. The nadir usually happens between 2-3 months, with hemoglobin levels between 9-11 g/dL.
Several factors cause this anemia. Newborns start with high levels of fetal hemoglobin. As they grow, adult hemoglobin takes over. Also, their body’s ability to make red blood cells is not yet fully developed.
Distinguishing Normal Nadir from Pathologic Anemia
It’s vital to tell the difference between normal and abnormal anemia in infants. Normal anemia is just a phase, but abnormal anemia means there’s a health problem. The main differences are how severe the anemia is, other symptoms, and the baby’s overall health.
| Characteristics | Physiologic Anemia | Pathologic Anemia |
| Hemoglobin Level | 9-11 g/dL | <9 g/dL |
| Age of Onset | 2-3 months | Variable |
| Symptoms | Typically asymptomatic | Pallor, fatigue, poor feeding |
Doctors need to watch infants closely during this time. They use both clinical checks and lab tests to tell normal anemia from the abnormal kind. Getting the diagnosis right is important. It helps avoid unnecessary treatments and makes sure babies with real anemia get help on time.
Key Value #4: Hemoglobin in Late Infancy (6-12 Months)
It’s important to know about hemoglobin levels in babies from 6 to 12 months. This is because they are usually getting better from a low point in health that happens at 2-3 months.
Recovery Patterns from Physiologic Nadir
After hitting the low point, babies start to make more red blood cells. This is because their bone marrow is working harder. Nutritional intake, like iron, helps a lot in this process.
Good nutrition is key for this recovery. Babies who drink breast milk or iron-fortified formula usually have better hemoglobin levels. This is compared to those who don’t.
Nutritional Influences on Hemoglobin Development
Nutrition greatly affects hemoglobin in late infancy. Iron intake is very important because it’s a big part of hemoglobin.
- Introduce iron-rich foods to babies around 6 months old.
- Babies who don’t get enough iron are more likely to get anemia.
- Breast milk or iron-fortified formula gives babies the iron they need.
Keeping an eye on nutrition can help avoid anemia. It also supports healthy hemoglobin levels in babies.
Key Value #5: Hemoglobin Ranges in Toddlers and Preschoolers
Hemoglobin levels in children aged 1-5 years are very important for their health. During this time, their hemoglobin levels usually settle down after the changes seen in infancy.
Normal Values for Children Ages 1-5 Years
The normal hemoglobin range for toddlers and preschoolers is between 11 and 14 g/dL. This range can change based on age, sex, and other factors. It’s important to check hemoglobin levels in this age group. This helps find anemia or other blood problems early.
| Age Group | Normal Hemoglobin Range (g/dL) |
| 1-2 years | 11.0-13.5 |
| 2-5 years | 11.5-14.0 |
Common Variations and Clinical Considerations
Many things can change hemoglobin levels in toddlers and preschoolers. These include not getting enough nutrients, chronic diseases, and genetic disorders. For example, iron deficiency is a big reason for anemia in young kids. It’s key to make sure they get enough iron through food or supplements.
“Iron deficiency anemia remains a significant public health issue among young children, necessitating regular screening and appropriate intervention.”
– Source: American Academy of Pediatrics
Doctors also need to think about other things that might affect hemoglobin levels. This includes lead exposure or ongoing infections. Keeping a close eye on hemoglobin levels and using good judgment is critical for managing them in young children.
In summary, knowing and watching hemoglobin levels in toddlers and preschoolers is essential. It helps keep them healthy and catches any problems early.
Key Value #6: School-Age Children Hemoglobin (11.5-15.5 g/dL)
Hemoglobin levels in school-age children stabilize and are influenced by various factors, including their activity level and overall health.
Stabilization of Hemoglobin Levels in Children 6-12 Years
Children between 6 and 12 years old see their hemoglobin levels stabilize. This is due to the body adapting to growth and development. The normal range for this age is between 11.5 and 15.5 g/dL.
Factors contributing to this stabilization include:
- Improved nutritional intake and absorption
- Enhanced erythropoiesis (red blood cell production)
- Stabilization of physiological processes
Activity Level and Hemoglobin Requirements
The activity level of school-age children affects their hemoglobin needs. More active kids might need higher hemoglobin levels to support their muscles. Increased physical activity can stimulate erythropoiesis, potentially leading to higher hemoglobin levels.
Doctors should look at a child’s activity level when checking their hemoglobin. For example, a child who plays sports regularly might need different hemoglobin levels than a less active child.
Key considerations for activity level and hemoglobin include:
- Assessing the intensity and frequency of physical activity
- Monitoring hemoglobin levels in relation to changes in activity level
- Adjusting nutritional recommendations to support hemoglobin production in active children
Key Value #7: Adolescent Hemoglobin Patterns
Puberty is a key time for changes in hemoglobin levels in teens. As they grow into adults, their hemoglobin patterns change a lot. These changes are due to many physical and hormonal shifts.
Gender Differences in Hemoglobin During Puberty
During puberty, boys and girls show different hemoglobin levels. Boys usually have more hemoglobin than girls. This is because sex hormones affect how the body makes red blood cells.
For example, androgens, or male sex hormones, help make more erythropoietin. This leads to more red blood cells and higher hemoglobin in boys. For more info on checking hemoglobin levels, doctors can look at the USPSTF recommendations.
| Age Group | Male Hemoglobin Range (g/dL) | Female Hemoglobin Range (g/dL) |
| 12-14 years | 13.0-16.0 | 12.0-15.5 |
| 15-17 years | 13.5-17.0 | 12.5-15.5 |
| 18 years and above | 14.0-18.0 | 12.0-16.0 |
Transition to Adult Reference Ranges
As teens get closer to being adults, their hemoglobin levels start to match adult ranges. This happens as they finish growing, hormones stabilize, and other body changes occur. It’s important for doctors to know these changes to manage hemoglobin-related issues well.
In summary, hemoglobin patterns in teens change a lot, with big differences between boys and girls. As they grow up, these patterns move towards adult levels. Doctors need to understand these changes to give the right care.
Evidence-Based Assessment of Pediatric Anemia
Identifying and managing pediatric anemia is key. This method uses the latest and most reliable data. It helps doctors diagnose and treat anemia in kids well.
Red Flags for Abnormal Hemoglobin Values
Spotting signs of abnormal hemoglobin is vital in pediatric care. Signs like pallor, fatigue, and poor growth can mean anemia. Doctors should watch for these and do detailed checks when they see them.
Low hemoglobin levels can point to serious issues. For example, significantly low hemoglobin might mean iron deficiency anemia or other nutritional problems.
Up-to-Date Diagnostic Protocols
Diagnosing pediatric anemia has changed with new evidence. Complete Blood Count (CBC) is a key tool. It shows important info on hemoglobin, MCV, and RDW.
More tests might be needed after the CBC. Iron studies and hemoglobin electrophoresis help find the cause of anemia. This guides the right treatment.
- Start with a CBC to check hemoglobin and red blood cell indices.
- More tests, like iron studies, might be needed to find specific issues.
- Think about nutrition and the environment’s effect on hemoglobin levels.
Following these protocols helps doctors diagnose and manage pediatric anemia accurately.
Population Differences and Special Considerations
Hemoglobin levels vary across different populations. This is due to factors like ethnicity, race, geography, and genetics. Each group has its own normal range.
Ethnic and Racial Variations in Normal Hemoglobin
Ethnic and racial differences affect normal hemoglobin levels. For example, people of African descent often have lower levels than those of European or Asian descent. A study in the Journal of Pediatrics found African American children have lower levels than Caucasian children.
The Centers for Disease Control and Prevention (CDC) notes a difference in hemoglobin ranges. African American children’s normal range is about 0.5-1 g/dL lower than Caucasian children’s. This is important for doctors to know when diagnosing anemia in kids.
| Ethnic Group | Normal Hemoglobin Range (g/dL) |
| Caucasian | 11.5-15.5 |
| African American | 11-14.5 |
| Asian | 11.5-15.5 |
Geographic and Environmental Factors
Where you live and your environment can also affect hemoglobin levels. For example, kids at high altitudes might have higher levels to handle lower oxygen. On the other hand, kids exposed to toxins or poor nutrition might be at risk for anemia.
“Children residing at high altitudes often develop adaptive mechanisms, including increased red blood cell production, to counteract the effects of hypoxia.”
– Journal of High Altitude Medicine and Biology
Genetic Hemoglobinopathies and Reference Ranges
Genetic conditions like sickle cell disease and thalassemia affect hemoglobin levels. These conditions often lead to abnormal levels that don’t reflect nutritional status or iron stores.
A study in the Journal of Pediatric Hematology/Oncology stressed the need to adjust reference ranges for these conditions. Doctors must be aware of these conditions when checking hemoglobin levels to avoid mistakes.
It’s key to understand these differences and special considerations. This helps in giving accurate diagnoses and effective care for kids with hemoglobin-related disorders.
Implementing Current Academic Protocols in Clinical Practice
Using the latest research in pediatric care has made hemoglobin assessment better. Healthcare providers can now be more accurate and effective in their assessments. This is thanks to the newest findings being used in practice.
Recent Research Advances in Pediatric Hemoglobin Assessment
New studies have greatly improved our knowledge of pediatric hemoglobin levels. It’s now clear that age-specific ranges are key for accurate assessments. For example, a study showed how important it is to consider changes in hemoglobin levels in young children.
Key findings from recent research include:
- More precise age-specific hemoglobin reference ranges have been established.
- Genetic factors that affect hemoglobin levels in kids have been identified.
- New tools for diagnosing hemoglobinopathies have been developed.
Multidisciplinary Approach to Hemoglobin Monitoring
For effective hemoglobin monitoring in kids, a team effort is needed. Pediatricians, hematologists, nutritionists, and others must work together. This team approach helps provide care that considers all factors affecting hemoglobin levels.
The benefits of a multidisciplinary approach include:
- Comprehensive assessment of factors influencing hemoglobin levels.
- Personalized treatment plans can be developed.
- Patient outcomes improve with coordinated care.
Digital Tools for Age-Specific Reference Range Application
Digital tools have changed how age-specific reference ranges are used in practice. Electronic health records (EHRs) and mobile apps give clinicians quick access to updated guidelines. This makes hemoglobin assessment more accurate and efficient.
| Digital Tool | Description | Benefits |
| EHR Systems | Electronic Health Records | Instant access to patient data and reference ranges |
| Mobile Apps | Applications for hemoglobin assessment | Portability and ease of use |
By using these digital tools and keeping up with research, clinicians can improve pediatric hemoglobin assessment. This leads to better patient care.
Conclusion: Optimizing Pediatric Care Through Accurate Hemoglobin Assessment
Getting the right hemoglobin levels is key for optimizing pediatric care. Knowing the pediatric hemoglobin levels for each age helps doctors spot and treat anemia and other issues.
This article gives seven important points for checking hemoglobin in kids. From babies to teens, accurate hemoglobin assessment helps doctors catch problems early. This leads to better care and results for kids.
Doctors can improve care by using the latest research and guidelines. They need to know how age affects hemoglobin and follow proven methods for checking and watching it.
In the end, optimizing pediatric care with accurate hemoglobin checks needs teamwork. It also means using new technology and keeping up with the latest in pediatric hemoglobin assessment.
FAQ
What is the normal hemoglobin range for newborns?
Newborns have a normal hemoglobin range of 14-24 g/dL. This is because of changes that happen during fetal development.
How do hemoglobin levels change during early infancy?
In early infancy, from 2-6 months, hemoglobin levels are between 10-17 g/dL. This change happens as they move from being newborns to infants.
What is the physiologic nadir, and when does it occur?
The physiologic nadir is a normal drop in hemoglobin levels. It happens around 2-3 months of age. It’s due to the breakdown of red blood cells and the body’s early response to making new ones.
How do nutritional factors influence hemoglobin development in late infancy?
Good nutrition, like enough iron, is key for hemoglobin growth in late infancy. Not getting enough iron can cause anemia, showing why watching what they eat is important.
What are the normal hemoglobin ranges for children aged 1-5 years?
Kids aged 1-5 years usually have hemoglobin levels between 11-14 g/dL. But, these can change a bit based on their age and other things.
How do hemoglobin levels change during adolescence?
In adolescence, hemoglobin levels can change based on gender. Boys usually have higher levels than girls. Levels tend to stabilize and get closer to adult ranges.
What are the red flags for abnormal hemoglobin values in pediatric patients?
Red flags include hemoglobin levels that are way off the normal range for their age. Also, look out for signs of anemia like being pale or tired. A family history of hemoglobin disorders is another warning sign.
How do ethnic and racial variations affect normal hemoglobin levels?
Ethnic and racial differences can affect normal hemoglobin levels. For example, people of African descent might have slightly lower average levels.
What is the role of digital tools in applying age-specific reference ranges for hemoglobin?
Digital tools, like electronic health records, help apply the right hemoglobin ranges for each age. This makes diagnosing and treating more accurate.
Why are age-specific reference ranges essential for hemoglobin assessment in pediatric care?
Age-specific ranges are vital because hemoglobin levels change a lot with age in kids. Using the right ranges helps make sure diagnoses and treatments are correct.
References
- MedlinePlus Medical Encyclopedia. (2024). Hemoglobin.