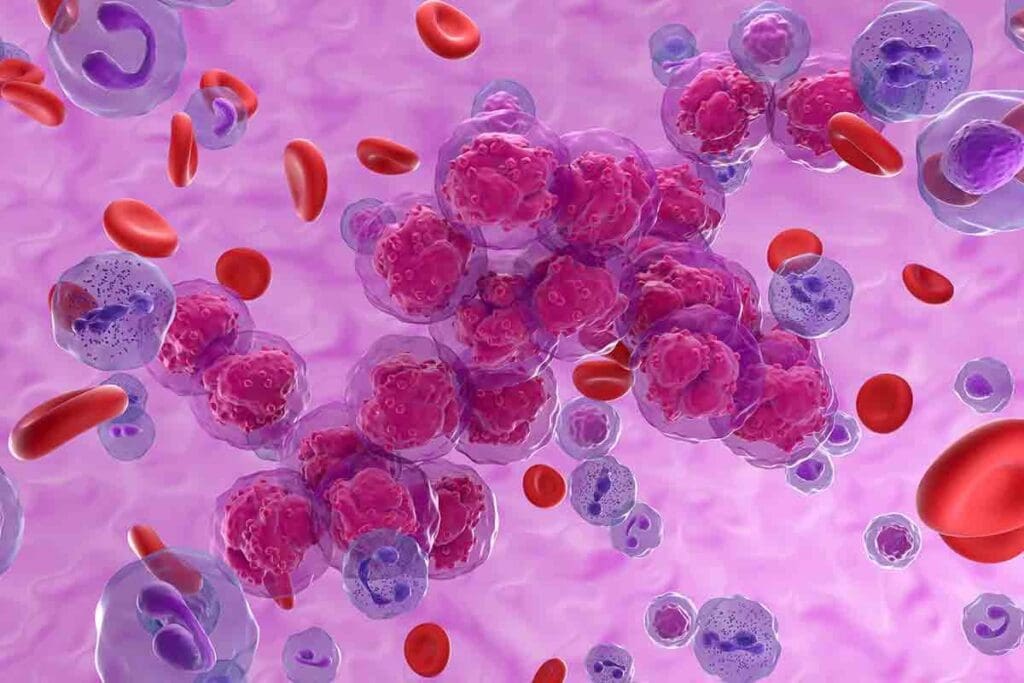
Getting a diagnosis of leukemia for a child can be scary. But it’s good to know that survival rates have gotten much better. Leukemia, the top cancer in kids, now has a brighter outlook.
The most common leukemia in kids, called acute lymphoblastic leukemia (ALL), has a survival rate of over 85% if caught early. Today, the five-year survival rate for leukemia in kids is over 86%. This gives families hope during a tough time.
Key Takeaways
- Leukemia is the most common cancer in children, making up about 30% of all childhood cancers.
- The five-year survival rate for children with leukemia has improved significantly.
- Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in children.
- Early diagnosis and appropriate treatment have significantly improved survival rates.
- The overall five-year survival rate for children with leukemia is now over 86%.
The Dramatic Improvement in Overall Pediatric Leukemia Survival Rates

Childhood leukemia used to be almost always fatal. Now, thanks to medical science, it has a much better outlook. The journey from old treatments to today’s care has seen big steps forward.
Historical Perspective: From Rare Survivors to Common Cures
In the 1970s, only about 10% of kids with leukemia lived five years after being diagnosed. This was because we didn’t know much about the disease, and treatments were not effective. But, over the years, hard work by many has greatly improved survival rates.
A big step forward was the use of combination chemotherapy. It was more effective than single treatments. Also, better care for infections and blood issues has helped kids live longer.
Current Five-Year Survival Statistics Exceeding 86%
Now, more than 86% of kids with leukemia in North America and Europe live five years after diagnosis. This shows how far we’ve come in understanding and treating the disease. The latest data shows survival rates keep getting better.
| Region | Five-Year Survival Rate |
| North America | 87% |
| Europe | 86% |
The Medical Advances Behind This Progress
Several medical advances have led to better survival rates for kids with leukemia. These include:
- More effective and less harmful chemotherapy
- Advances in stem cell transplants
- Understanding leukemia’s genetics and molecules for targeted treatments
- Better care for infections and nutrition
A leading pediatric oncologist says, “The progress in treating childhood leukemia is thanks to global teamwork. Clinicians, researchers, and families are working together to make new treatments possible.”
“The cure of childhood leukemia is one of the most significant achievements in modern medicine, reflecting a journey of relentless pursuit of better treatments and outcomes.”
-As noted by a pediatric oncologist
As we keep improving treatments and adding new therapies, we hope to make survival rates even better. This will also improve the quality of life for kids with leukemia.
Understanding Acute Lymphoblastic Leukemia (ALL) Success Rates
Acute Lymphoblastic Leukemia (ALL) is now one of the most curable childhood cancers. This is thanks to big steps in medical research and treatment. Pediatric oncologists, researchers, and healthcare teams have worked hard to improve how we diagnose and treat it.
Why ALL Has the Highest Cure Rate Among Childhood Cancers
ALL’s high cure rate is due to early detection, better treatments, and understanding the disease. Early detection is key because it lets us start treatment early. This helps stop the disease from getting worse.
Refined treatment protocols also play a big role. These are made from lots of research and trials. They ensure kids get the best treatment possible.
Current 90-94% Five-Year Survival Statistics
Today, the five-year survival rate for ALL in kids is 90-94%. This is a big jump from before. It shows how far we’ve come in fighting this disease.
| Year | Five-Year Survival Rate |
| 1990s | 80% |
| 2000s | 85% |
| 2020s | 90-94% |
B-Cell ALL: Specific Outcomes and Treatment Approaches
B-cell ALL has seen big improvements in treatment. The current methods include intensive chemotherapy regimens and sometimes targeted therapy. These have been shown to be very effective, with cure rates over 85% in many cases.
The success in treating B-cell ALL also comes from precision medicine. It lets us create treatment plans that fit each patient’s unique genetic makeup.
Acute Myeloid Leukemia (AML): Challenging But Improving Prognosis
Acute Myeloid Leukemia (AML) has seen a big change in its outlook. What was once a tough condition to treat has now seen better survival rates for kids. This is thanks to new discoveries in medicine.
The Journey from 14% to 65-70% Survival Rates
Survival rates for kids with AML have jumped from 14% in the 1970s to about 65-70% today. This big leap is thanks to better treatments. These include strong chemotherapy and stem cell transplants.
Many things have helped improve survival rates. Better understanding of the disease, new diagnostic tools, and more effective treatments are key. Clinical trials have also been vital in finding the best ways to treat AML.
Why AML Remains More Difficult to Treat Than ALL
Even with progress, AML is harder to treat than Acute Lymphoblastic Leukemia (ALL). AML’s complexity and aggressiveness make it tough. Genetic and molecular heterogeneity among AML patients also makes finding targeted treatments hard.
AML also has a higher chance of coming back. This means kids need even stronger treatments. Finding the right treatment for each child is a big challenge in managing AML.
Recent Breakthroughs Improving AML Outcomes
Recently, there have been big steps forward in treating AML. New targeted therapies focus on specific genetic mutations, like FLT3 inhibitors. Also, better hematopoietic stem cell transplantation has made this treatment safer and more effective.
Immunotherapy is also showing great promise. Many clinical trials are looking into its use in AML. Adding new treatments to existing ones is expected to keep improving survival rates and reduce side effects.
Critical Factors That Influence Pediatric Leukemia Survival Rate
Several key factors significantly impact the survival rates of children diagnosed with leukemia. Understanding these factors is essential for parents, healthcare providers, and researchers. It helps improve treatment outcomes and quality of life for young patients.
Age at Diagnosis: Why It Matters
The age of a child at the time of diagnosis plays a critical role. Infants under one year and children over 10 years face different challenges. Age influences not only the type of leukemia but also the likelihood of response to treatment.
Children diagnosed with Acute Lymphoblastic Leukemia (ALL) between 1 and 9 years have the most favorable prognosis. They have higher cure rates in this age group.
White Blood Cell Count as a Prognostic Indicator
The white blood cell (WBC) count at diagnosis is another critical factor. A high WBC count often indicates a more aggressive disease. Monitoring WBC count helps healthcare providers adjust treatment plans.
Genetic and Chromosomal Markers
Genetic and chromosomal abnormalities within leukemia cells provide valuable information. They help understand the disease’s aggressiveness and treatment response. Certain genetic markers are associated with a better or worse prognosis, guiding treatment decisions.
Early Response to Treatment: A Key Predictor
The initial response to treatment is a significant predictor of long-term outcomes in pediatric leukemia. Children who respond well to early treatment generally have better survival rates. Monitoring early response helps in tailoring treatment strategies for optimal results.
By understanding and closely monitoring these critical factors, healthcare providers can develop more effective treatment plans. This ultimately improves pediatric leukemia survival rates.
Age-Specific Outcomes: Infant vs. Older Child Leukemia
Pediatric leukemia outcomes change with age, with infants under one facing unique challenges. The disease affects infants differently from older children. This requires a closer look at age-specific outcomes.
Why Babies Under One Year Face Greater Challenges
Infants under one year have a harder time with leukemia. Their disease often has high-risk features, like Mixed Lineage Leukemia (MLL) gene rearrangements. These are linked to a poorer prognosis. Their young immune system and fast disease progression also make treatment harder.
Leukemia in infants is often aggressive and hard to treat. This is because of the disease’s biology in this age group. It often involves genetic mutations that make the leukemia resistant to treatment.
Current Survival Statistics for Infant Leukemia
Survival rates for infant leukemia have improved but are lower than for older children. The five-year survival rate for infants with Acute Lymphoblastic Leukemia (ALL) is about 60-70%. This is much lower than the 90%+ rates for older children.
| Age Group | Five-Year Survival Rate for ALL |
| Infants (<1 year) | 60-70% |
| Children (1-9 years) | 90% |
| Adolescents (10-19 years) | 80-85% |
How Age Affects Treatment Approaches and Outcomes
Age greatly influences leukemia treatment in children. Infants need special treatment plans. These plans consider their disease biology and aim to avoid long-term harm. Treatment for infants often includes more intense chemotherapy and sometimes stem cell transplantation.
The outcome for infants with leukemia depends on how well they respond to treatment. Those who quickly go into remission tend to have better survival rates. Researchers are working to improve treatments for this age group. They aim to use targeted therapies that are less toxic but more effective.
Long-Term Survival Beyond the Five-Year Milestone
After beating leukemia, kids face new challenges. They need ongoing care to stay healthy and happy.
What Happens After the Critical Five-Year Mark
After five years, kids are watched for treatment side effects. These can include learning problems, growth issues, or hormonal imbalances. Regular check-ups are key to catching these issues early.
Late effects of treatment can differ for each survivor. Some might struggle with:
- Cognitive difficulties
- Emotional challenges
- Physical health issues
Late Effects and Quality of Life Considerations
Survivors’ quality of life is a big concern. They might deal with long-term health problems that impact their daily life. It’s important to think about these when looking at the childhood leukemia survival rate.
As one survivor noted, “The journey doesn’t end at five years; it’s just the beginning of a new chapter in life.”
Lifelong Monitoring and Follow-Up Care
Long-term monitoring is key to managing side effects and keeping survivors healthy. Regular check-ups and screenings help catch problems early, allowing for quick action.
A good follow-up care plan includes:
- Regular health check-ups
- Screenings for possible late effects
- Support for emotional and psychological well-being
By focusing on long-term care, we can boost the leukemia survival rate in children. This improves survivors’ quality of life.
Relapse Scenarios: Understanding Secondary Treatment Outcomes
Relapse in pediatric leukemia is a tough challenge. It requires a deep understanding of secondary treatment outcomes. Families face a daunting experience when leukemia comes back after the first diagnosis and treatment.
Risk Factors for Leukemia Recurrence
Several factors increase the risk of leukemia coming back in children. These include:
- The initial white blood cell count at diagnosis
- Specific genetic abnormalities, such as the Philadelphia chromosome
- The presence of minimal residual disease (MRD) after initial treatment
- The child’s response to the initial treatment regimen
Knowing these risk factors is key to creating effective treatment plans for relapse. TheNational Cancer Institute says assessing relapse risk helps tailor therapies.
Survival Rates After Relapse
Survival rates after relapse depend on many factors. These include the timing, location, and overall health of the child. Generally, children with relapse face a poorer prognosis. But treatment advances have improved some outcomes.
For example, kids with Acute Lymphoblastic Leukemia (ALL) who relapse might achieve a second remission. This can happen with intensive chemotherapy and sometimes a hematopoietic stem cell transplant. The survival rates after relapse are getting better, giving families hope.
Innovative Therapies for Resistant Disease
Creating innovative therapies is vital for better outcomes in resistant or relapsed leukemia. These include:
- Targeted therapies that target specific genetic weaknesses in leukemia cells
- Immunotherapies, like CAR-T cell therapy, which show great promise in treating relapsed or refractory ALL
- New chemotherapeutic agents and combinations are being tested in clinical trials
These new approaches are being studied in clinical trials. They offer hope for children with leukemia that doesn’t respond to usual treatments.
Regional and Demographic Variations in Treatment Outcomes
The survival rate for childhood leukemia changes a lot depending on where you live and who you are. This is a big problem that affects how well kids with leukemia do. It changes the pediatric leukemia survival rate and childhood leukemia survival numbers.
Access to Specialized Pediatric Cancer Centers
Getting treatment at a specialized pediatric cancer center is key. Kids with leukemia do better when they get care at these places. A study showed that kids treated at these centers live longer than those at regular hospitals.
Specialized centers offer many benefits. They have:
- Teams of experts in pediatric oncology
- Access to the latest treatments and clinical trials
- Support services for patients and their families
Socioeconomic Factors Affecting Survival
Socioeconomic status also affects how well kids with leukemia do. Families with more money can usually get better healthcare. But, families with less money face big challenges. These include:
- Harder time getting health insurance
- Higher costs for traveling to specialized centers
- Longer times to get a diagnosis because of less access to doctors
These issues lead to differences in childhood leukemia survival rates.
Closing the Gap: Initiatives to Equalize Outcomes
To fix these problems, many efforts are being made. These aim to make healthcare more accessible and reduce money issues. Some of these efforts are:
- Telemedicine to let patients talk to specialists from home
- Programs to help families pay for treatment
- Outreach and education to help find leukemia early
Healthcare providers are working hard to make sure all kids have a fair chance. They want to close the gap in pediatric leukemia survival rate. This will help more kids survive leukemia.
Conclusion: Navigating the Journey Through Childhood Leukemia
The journey through childhood leukemia is complex. It involves many factors that affect the survival rate. Recent data show a big improvement in survival rates, with over 86% of kids surviving five years.
But, some groups and ages face bigger challenges. This shows the need for more work in treating leukemia in kids.
Thanks to medical research, treating pediatric leukemia has gotten better. Acute Lymphoblastic Leukemia (ALL) now has a five-year survival rate of 90-94%. Acute Myeloid Leukemia (AML) is harder to treat, but new discoveries are helping.
Knowing the prognosis for leukemia in kids is key. It depends on age, white blood cell count, and genetic markers. These factors help doctors choose the best treatment and predict survival chances.
Doctors are working hard to improve treatments and address unfair differences in care. This makes the future look brighter for kids with leukemia. By understanding the latest research and treatments, families can face the journey with hope.
FAQ
What is the current five-year survival rate for pediatric leukemia?
The five-year survival rate for pediatric leukemia is now over 86%. This is a big improvement from recent years.
How has the survival rate for Acute Lymphoblastic Leukemia (ALL) improved?
The survival rate for ALL has jumped to 90-94%. This makes it one of the most treatable childhood cancers.
What are the challenges in treating Acute Myeloid Leukemia (AML) in children?
AML is harder to treat than ALL. It’s aggressive and has complex treatment plans.
How does age at diagnosis affect pediatric leukemia survival rates?
Age at diagnosis is very important. Infants under one year face bigger challenges and often have worse outcomes than older kids.
What factors influence the prognosis of pediatric leukemia?
Several factors affect prognosis. These include white blood cell count, genetic markers, and how well the treatment works early on.
What happens after the five-year survival milestone in pediatric leukemia?
After five years, patients need ongoing care. This is to manage late effects of treatment and keep their quality of life good.
What are the survival rates after relapse in pediatric leukemia?
Survival after relapse depends on several things. These include the type of leukemia, when the relapse happens, and how well the second treatment works.
How do socioeconomic factors affect pediatric leukemia survival rates?
Socioeconomic factors, like access to care, greatly impact survival rates. Efforts are being made to close these gaps.
Is childhood leukemia curable?
Yes, many childhood leukemias are curable today. ALL, in particular, has a high cure rate among childhood cancers.
What is the survival rate for infant leukemia?
Infant leukemia survival rates are lower than for older kids. But treatment advances are helping improve these rates.
How does the type of leukemia affect survival rates in children?
The type of leukemia matters a lot. ALL has a higher cure rate than AML, which is harder to treat.
References
- Buechner, J., Zwaan, C. M., Pabst, T., & Creutzig, U. (2023). Pediatric Acute Myeloid Leukemia — Past, Present, and Future. Frontiers in Pediatrics, 11, Article 8837075. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8837075/
- National Cancer Institute. (2025, January). Childhood Acute Myeloid Leukemia Treatment (PDQ®). https://www.cancer.gov/types/leukemia/hp/child-aml-treatment-pdq