Last Updated on November 20, 2025 by Ugurkan Demir
Precursor B Cell Acute Lymphoblastic Leukemia (ALL) is a serious cancer. It affects the bone marrow and blood. It’s the most common leukemia in kids, making up 75-80 percent of cases.
We will look at the different types, symptoms, and treatments for this condition.
Understanding Precursor B Cell ALL is key for those affected. Places like Liv Hospital offer advanced care and hope for better survival rates.
Key Takeaways
- Precursor B Cell ALL is the most common type of leukemia in children.
- It accounts for 75-80 percent of childhood ALL cases.
- Advanced protocols and compassionate care are improving survival rates.
- Understanding the subtypes, symptoms, and treatment options is critical.
- Trusted institutions like Liv Hospital are leading the way in care.
What Is Precursor B Cell ALL?
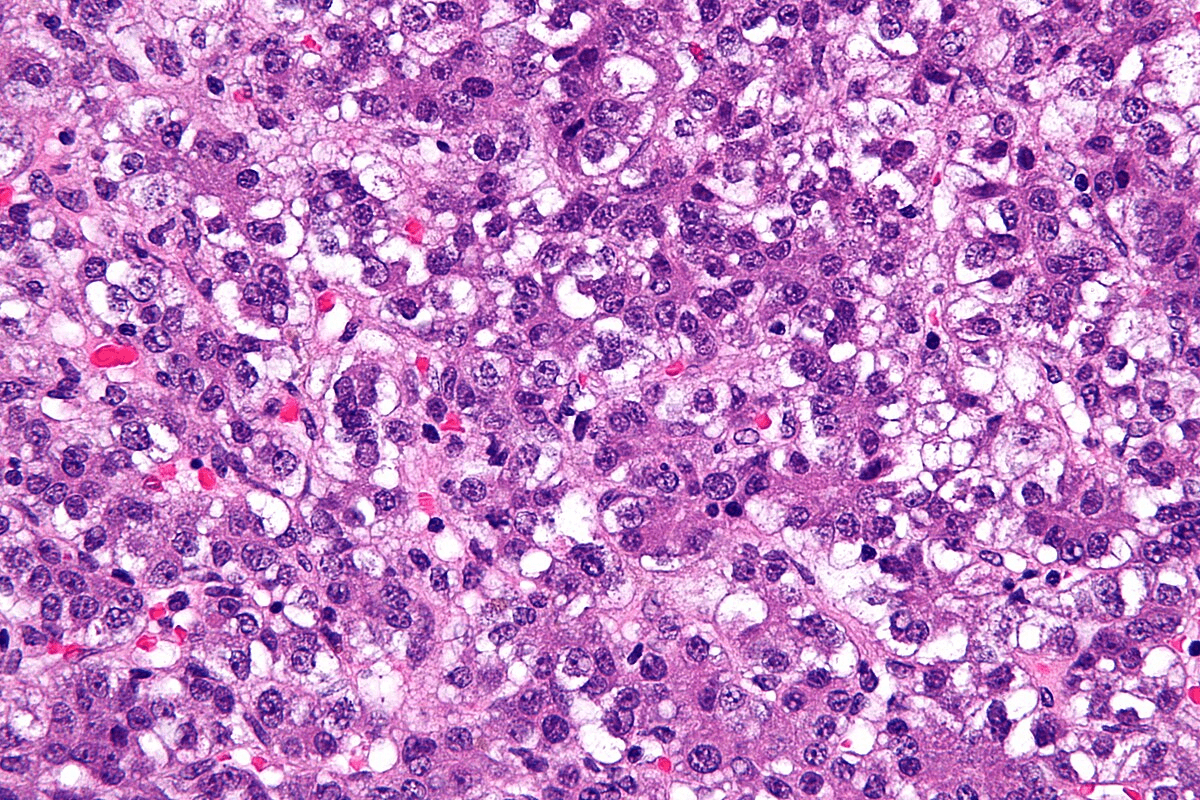
We will look into Precursor B Cell ALL, a complex condition. It involves the abnormal growth of immature B cells. This cancer affects the blood and bone marrow, causing an abnormal buildup of cells.
Definition and Classification
Precursor B Cell ALL, also known as Precursor B Cell Acute Lymphoblastic Leukemia, starts in the bone marrow. It’s classified by specific genetic changes and the stage of B cell development. The World Health Organization (WHO) system is used to categorize it based on genetic and morphological features.
Classifying Precursor B Cell ALL means finding certain genetic changes. For example, the Philadelphia chromosome, from a chromosome 9 and 22 swap, is a key factor in treatment choices.
Prevalence in Childhood Leukemia Cases
Precursor B Cell ALL is the most common leukemia in kids, making up 80-85% of pediatric ALL cases. It most often strikes between 2 and 5 years old. The types of genetic changes can differ by age and population.
| Age Group | Prevalence of Precursor B Cell ALL | Common Genetic Subtypes |
| 0-5 years | High | ETV6-RUNX1 translocation |
| 6-15 years | Moderate | Hyperdiploidy |
| 16+ years | Low | Philadelphia chromosome-positive |
Knowing how Precursor B Cell ALL varies by age helps in creating better treatments. This knowledge is key to improving patient outcomes.
The Biology Behind Precursor B Cell ALL
To understand Precursor B Cell ALL, we must first learn about B-cell development. This cancer affects the blood and bone marrow. It’s known as Pre B Acute Lymphoblastic Leukemia.
Normal B-Cell Development
B-cell development happens in the bone marrow. It’s a complex process. B-cells mature from precursors into functional cells that help fight infections.
This development is controlled by checkpoints. These ensure the immune system works right. Any problem can lead to leukemia.
Malignant Transformation Process
The transformation of B-cell precursors into cancer is key in Precursor B Cell ALL. This involves genetic changes that let cancer cells grow and live too long.
Genetic changes, like chromosomal translocations, drive this transformation. These changes can turn on genes that cause cancer or turn off genes that stop it. This leads to leukemia.
How Leukemic Cells Disrupt Bone Marrow Function
Leukemic cells in Precursor B Cell ALL harm the bone marrow. They take over space meant for healthy cells. This causes problems like anemia and low blood counts.
These cells also change the bone marrow environment. This supports their growth. Knowing how they harm the bone marrow helps in finding better treatments.
Genetic Subtypes and Classifications of Precursor B Cell ALL
Precursor B Cell Acute Lymphoblastic Leukemia (ALL) has many genetic subtypes. These subtypes greatly affect how well the disease can be treated. Knowing the genetic makeup of the disease is key to finding the best treatment.
The t(9;22)-BCR-ABL Philadelphia Chromosome
The t(9;22) translocation creates the BCR-ABL fusion gene. This is a big deal in Precursor B Cell ALL. It’s more common in adults and makes the disease harder to treat. But, new drugs called tyrosine kinase inhibitors (TKIs) have helped a lot.
The t(12;21)-ETV6-RUNX1 Translocation
The t(12;21) translocation leads to the ETV6-RUNX1 fusion. This is the most common genetic change in kids with Precursor B Cell ALL. Kids with this subtype usually do well. The ETV6-RUNX1 fusion happens early in B-cell development and affects how well the disease responds to treatment.
Other Significant Genetic Alterations
Other genetic changes in Precursor B Cell ALL include MLL gene rearrangements, hyperdiploidy, and hypodiploidy. Each change has its own impact on how the disease will progress. For example, high hyperdiploidy is good for kids, while hypodiploidy is not.
It’s very important to understand these genetic subtypes for treatment planning. As research gets better, finding specific genetic changes will help make treatments more targeted for Precursor B Cell ALL.
Key Symptoms of Precursor B Cell ALL
It’s important to know the symptoms of Precursor B Cell ALL to get help quickly. This type of leukemia shows different signs, so it’s key for both patients and doctors to spot them early.
Early Warning Signs
In the early stages, Precursor B Cell ALL might seem like a viral infection. Look out for fatigue, pallor, and frequent infections. You might also notice unexplained weight loss or night sweats.
These signs can be easy to overlook. But if they keep happening or get worse, it’s time to see a doctor.
Physical Manifestations
As the disease gets worse, you might see more obvious signs. Look for enlarged lymph nodes, splenomegaly, and hepatomegaly. You could also feel bone pain or joint pain because of the disease in your bones.
You might see petechiae or ecchymoses too. These are small spots or bruises from low platelet counts.
Emergency Symptoms Requiring Immediate Care
Some symptoms need help right away. Watch for severe bleeding, high fever that won’t go away, and symptoms of anemia like shortness of breath. Also, severe headache, vomiting, or altered mental status are emergencies.
Spotting these signs fast can really help treatment. It’s vital for patients and their families to know these signs and get help right away.
Diagnostic Process for Precursor B Cell ALL
To diagnose Precursor B Cell ALL, doctors use several tests. These tests help find the disease’s specific traits. This information helps decide the best treatment.
Initial Blood Work Findings
The first step is blood tests to check overall health and look for blood cell issues. Complete Blood Count (CBC) is key. It checks white, red blood cells, and platelets. In Precursor B Cell ALL, CBC often shows abnormal white blood cell counts.
Blood tests also look for signs of leukemia, like anemia or low platelets. These signs aren’t specific but lead to more detailed tests.
Bone Marrow Analysis Techniques
Bone marrow analysis is key for Precursor B Cell ALL diagnosis. It looks at bone marrow cells for leukemic cells. The process starts with bone marrow aspiration from the hip bone.
Bone marrow biopsy might also be done. It removes a small bone piece with marrow. This gives more info on the bone marrow.
Advanced Genetic and Molecular Testing
Genetic and molecular tests are vital for Precursor B Cell ALL diagnosis. Fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) find genetic issues. These tests help find specific chromosomal changes.
These tests also help predict how the disease will progress. They help sort patients into risk groups. This helps doctors tailor treatments for each patient.
Age-Related Differences in Precursor B Cell ALL
Understanding the age-related differences in Precursor B Cell ALL is key for effective treatment. This disease shows different signs in people of all ages, from young children to older adults.
Pediatric Presentation and Characteristics
In kids, Precursor B Cell ALL is the most common leukemia. It usually starts between 2 and 5 years old. Kids often show signs like pale skin, tiredness, and easy bruising because their bone marrow fails.
Children with this disease usually respond well to treatment. This means they have a higher chance of being cured.
Pediatric Precursor B Cell ALL often has specific genetic changes. For example, the ETV6-RUNX1 fusion is common. This is linked to a better outlook.
Adult Manifestation Differences
In adults, Precursor B Cell ALL is different from what kids experience. Adults often have more complex genetic changes. They also have a higher chance of having the Philadelphia chromosome-positive subtype.
Adults may have more severe symptoms, like losing a lot of weight, sweating a lot at night, and swollen lymph nodes. Treatment is less effective for adults, leading to lower survival rates.
| Characteristics | Pediatric | Adult |
| Common Age Range | 2-5 years | Variable, often >20 years |
| Genetic Features | ETV6-RUNX1 fusion common | Philadelphia chromosome-positive is more common |
| Treatment Response | Generally favorable | Less favorable |
Geriatric Considerations
In older adults, Precursor B-cell ALL is less common. It often comes with other health issues and a lower ability to handle treatments. Older patients may need special treatment plans that are easier on them.
It’s important to think about other health problems and how medicines might interact when treating older adults with this disease.
Prognosis Factors in Precursor B Cell ALL
Several key factors affect the outcome of Precursor B Cell ALL. These include age, genetic markers, and how well the patient responds to treatment. Knowing these factors helps predict how a patient will do and guides doctors in making treatment plans.
Age as a Critical Prognostic Factor
Age is a big factor in how well a patient with Precursor B Cell ALL will do. Children between 1 and 9 years old usually have a better chance of recovery than younger or older patients. This is because their leukemia might be different, and they can handle chemotherapy better.
Infants often face a tougher road because their leukemia might have Mixed Lineage Leukemia (MLL) gene rearrangements. These make treatment harder. Older adults might also have health issues that make treatment more challenging, leading to a less hopeful outlook.
Genetic Markers and Their Prognostic Value
Genetic markers are very important in predicting how a patient with Precursor B Cell ALL will do. Some genetic changes, like the t(12;21)-ETV6-RUNX1 translocation, are good signs. But others, like the t(9;22)-BCR-ABL Philadelphia chromosome, are not as promising.
| Genetic Marker | Prognostic Value |
| t(12;21)-ETV6-RUNX1 | Favorable |
| t(9;22)-BCR-ABL | Poor |
| MLL gene rearrangements | Poor |
Response to Initial Treatment
How well a patient responds to the first treatment is also very important. Those who quickly go into complete remission after starting treatment usually do better than those who don’t. Doctors check this by looking at the bone marrow after the first round of chemotherapy.
We group patients based on these factors to decide on the best treatment. For example, those at higher risk might need stronger treatments or even a stem cell transplant.
In summary, knowing about the prognosis factors in Precursor B Cell ALL is key to improving treatment plans. By looking at age, genetic markers, and how well the patient responds to treatment, doctors can give more tailored and effective care.
Risk Factors for Developing Precursor B Cell ALL
Precursor B Cell ALL can be caused by several risk factors. Knowing these factors helps us find people at higher risk. This knowledge can help prevent the disease.
Genetic Syndromes and Predispositions
Some genetic syndromes raise the risk of getting Precursor B Cell ALL. For example, people with Down syndrome are more likely to get leukemia, including Precursor B Cell ALL. Other conditions like ataxia-telangiectasia and Li-Fraumeni syndrome also increase the risk. This is because they affect DNA repair and tumor suppression.
Genetic predispositions are key. Research has found specific genetic changes that lead to Precursor B Cell ALL. For instance, mutations in genes related to B-cell development can raise the risk of cancer.
Environmental Exposures
Environmental factors also play a big role in Precursor B Cell ALL. Young people exposed to ionizing radiation face a higher risk of leukemia. This includes radiation from medical treatments, nuclear accidents, or other sources.
Chemicals like benzene and certain pesticides also increase the risk. The effect of electromagnetic fields (EMFs) on leukemia risk is being studied, with mixed results.
Other Contributing Factors
Other factors can also contribute to the risk of Precursor B Cell ALL. Infections and immune system problems might play a role, but the exact mechanisms are not clear.
Some research suggests that not getting certain infections early in life might raise the risk of ALL. This idea is part of the hygiene hypothesis.
It’s important to understand these risk factors for prevention and early detection. While some risks can’t be changed, research and awareness help us manage Precursor B Cell ALL better.
Standard Treatment Protocols for Precursor B Cell ALL
Treating Precursor B Cell Acute Lymphoblastic Leukemia (ALL) is complex. It has changed a lot over time. We will look at the main treatments, aiming to fight the disease well while keeping side effects low.
Induction Chemotherapy
Induction chemotherapy is the first step. It tries to get rid of leukemia cells in the bone marrow. This part lasts weeks and uses many drugs. The goal is to make the leukemia cells disappear.
Key components of induction chemotherapy include:
- Corticosteroids to reduce inflammation and kill leukemia cells
- Vincristine to disrupt cell division and prevent leukemia cell growth
- Anthracyclines, such as daunorubicin, intercalate into DNA and inhibit cancer cell proliferation
- Asparaginase to deplete asparagine, an amino acid essential for leukemia cell survival
Consolidation and Maintenance Therapy
After getting rid of leukemia cells, consolidation and maintenance therapy are key. Consolidation uses strong chemotherapy to kill more cells. Maintenance keeps the disease away for a long time.
The main objectives of consolidation and maintenance therapy are:
- To intensify treatment and eliminate residual leukemia cells
- To maintain remission and prevent disease recurrence
- To monitor for and manage any long-term side effects of treatment
Central Nervous System Prophylaxis
CNS prophylaxis is vital for Precursor B Cell ALL. It stops leukemia cells from hiding in the brain. This involves putting chemotherapy directly into the spinal fluid or using drugs that can get into the brain.
Genetic markers are important in treating Precursor B Cell ALL. Some genetic changes, like the Philadelphia chromosome, need special treatments. This includes drugs that target specific genes.
Knowing the genetic makeup of the disease helps tailor treatments for each patient.
Advanced Treatment Options
New treatments are being developed for Precursor B Cell ALL. These include innovative therapies that can save lives for those with high-risk or relapsed cases.
We will look at stem cell transplantation, targeted therapies, and immunotherapy. These are key in managing this complex disease.
Stem Cell Transplantation Indications
Stem cell transplantation is a key treatment for some with Precursor B Cell ALL. It replaces the bone marrow with healthy stem cells, either from the patient or a donor.
It’s used for:
- High-risk disease at diagnosis
- Relapsed or refractory disease
- Presence of minimal residual disease (MRD) after initial treatment
| Indication | Description | Transplant Type |
| High-risk disease | Presence of high-risk genetic features or poor response to initial treatment | Allogeneic |
| Relapsed disease | Disease recurrence after initial remission | Allogeneic |
| MRD positive | Presence of minimal residual disease after initial treatment | Allogeneic or Autologous |
Targeted Therapies for Specific Genetic Subtypes
Targeted therapies have changed how we treat Precursor B Cell ALL. They focus on specific genetic issues that cause the disease.
For example, those with the Philadelphia chromosome-positive (Ph+) subtype can benefit from tyrosine kinase inhibitors (TKIs). Drugs like imatinib and dasatinib target the BCR-ABL fusion protein. This improves outcomes for this subgroup.
Immunotherapy Approaches
Immunotherapy is a promising area in treating Precursor B Cell ALL. It uses the immune system to fight leukemia cells.
One exciting area is CAR-T cell therapy. It involves modifying T cells to target leukemia cells. These modified T cells are then given back to the patient.
There are significant advancements in treating Precursor B Cell ALL. This brings new hope to patients and their families. As research continues, we can expect even more effective treatments.
Multidisciplinary Approach to Patient Care
Managing Precursor B Cell ALL needs a team effort. A group of healthcare experts work together. They focus on both the physical and emotional health of patients.
The Role of the Healthcare Team
The team is key in fighting Precursor B Cell ALL. It includes doctors, nurses, and others. They create a treatment plan that fits each patient’s needs.
Key members of the healthcare team and their roles:
- Hematologists and oncologists: They diagnose and treat Precursor B Cell ALL. They make plans that meet each patient’s needs.
- Nurses: They give ongoing care and support. They teach patients and their families about the condition.
- Supportive care specialists: They help with emotional, psychological, and social needs. This improves patients’ quality of life.
Supportive Care Measures
Supportive care is a big part of managing Precursor B Cell ALL. It helps with symptoms, side effects, and improving outcomes. Supportive care includes:
- Infection prophylaxis and management
- Blood component transfusions
- Nutritional support
- Psychological counseling
These steps are important. They help patients live better and handle tough treatments.
Latest Academic Protocols and Research Advances
The fight against Precursor B Cell ALL is always getting better. New research brings new treatments and strategies. Recent breakthroughs include:
- Targeted therapies for specific genetic types
- Immunotherapy, like CAR-T cell therapy
- New chemotherapy drugs and combinations
Healthcare providers need to know about these new findings. This way, they can give patients the best treatments available.
Conclusion
Precursor B Cell ALL is a complex disease that needs a deep understanding. We’ve looked at its biology, diagnosis, and treatment in this article. Knowing these details is key for doctors and patients to work together.
Managing Precursor B Cell ALL requires a team effort. This includes using new treatments like targeted therapies and immunotherapy. Keeping up with the latest research helps doctors give care that fits each patient’s needs.
In summary, knowing a lot about Precursor B Cell ALL is vital for good care. As research grows, we’ll see better treatments and outcomes for patients everywhere.
FAQ
What is Precursor B Cell ALL?
Precursor B Cell ALL is a type of leukemia. It happens when immature B lymphoblasts build up in the bone marrow and blood.
What are the symptoms of Precursor B Cell ALL?
Symptoms can vary. They might include feeling very tired, losing weight, and getting sick often.
How is Precursor B-cell ALL diagnosed?
Doctors use blood tests, bone marrow analysis, and genetic testing. These help confirm the diagnosis and find the disease’s subtype.
What are the genetic subtypes of Precursor B Cell ALL?
There are different genetic subtypes. Each has its own outlook, like the t(9;22)-BCR-ABL and t(12;21)-ETV6-RUNX1 translocations.
What is the prognosis for Precursor B Cell ALL?
The outlook depends on several factors. These include age, genetic markers, and how well the disease responds to treatment.
What are the treatment options for Precursor B Cell ALL?
Treatment is a multi-phase process. It includes induction chemotherapy, consolidation, maintenance therapy, and central nervous system prophylaxis. Some patients may also need stem cell transplantation or targeted therapies.
What is the role of stem cell transplantation in Precursor B Cell ALL?
Stem cell transplantation is considered for high-risk or relapsed cases. It offers a chance for a cure.
How does age affect the prognosis and treatment of Precursor B Cell ALL?
Age is a key factor. Older patients usually face a worse prognosis and may need more aggressive treatment.
What are the risk factors for developing Precursor B Cell ALL?
Some genetic syndromes and environmental factors can raise the risk. But the exact causes are not yet fully understood.
References:
- Ding, F., et al. (2025). Analysis of global trends in acute lymphoblastic leukemia in children. BMC Pediatrics, 25, Article 123. https://pmc.ncbi.nlm.nih.gov/articles/PMC11966407/
- Kroeze, E., et al. (2022). Pediatric Precursor B-Cell Lymphoblastic Malignancies. Frontiers in Pediatrics, 10, Article 900123. https://pmc.ncbi.nlm.nih.gov/articles/PMC9405801/