Last Updated on November 20, 2025 by Ugurkan Demir

Bone Marrow Transplant (BMT) is a medical procedure that saves lives. It replaces damaged bone marrow with healthy stem cells. This is key for those with certain cancers and blood disorders. Discover what bmt meaning medical and how it’s used in treating blood and bone marrow disorders.
At Liv Hospital, we understand the complex nature of BMT. We’re dedicated to patient-focused care. Our team helps patients and families navigate the treatment process, ensuring they get the best care.
A BMT involves putting healthy stem cells into the body to make blood cells again. This can be done using the patient’s own stem cells (autologous) or donor stem cells (allogeneic).
Key Takeaways
- BMT is a medical procedure that replaces unhealthy bone marrow with healthy stem cells.
- It’s used to treat life-threatening diseases, including certain cancers and blood disorders.
- The procedure can be autologous or allogeneic, depending on the source of the stem cells.
- Liv Hospital provides complete care and support for patients undergoing BMT.
- Understanding BMT is vital for patients and families facing serious blood disorders.
BMT Meaning Medical: Definition and Basics
Bone Marrow Transplant, or BMT, has changed how we treat blood-related diseases. It’s important to understand BMT basics to see its role in medicine.
Full Form and Definition of BMT
BMT means Bone Marrow Transplant. It’s a way to replace bad bone marrow with healthy stem cells. It helps with leukemia, lymphoma, aplastic anemia, and some immune problems. The term BMT is key in hematology and oncology.
Historical Development of Bone Marrow Transplantation
The first BMT was done in the 1970s by E. Donnall Thomas, MD, and his team. Their work led to the use of transplants in medicine and won them a Nobel Prize. Over time, BMT has grown, thanks to new tech and an understanding of the immune system.
| Year | Milestone |
| 1970s | First bone marrow transplant performed by E. Donnall Thomas, MD |
| 1980s | Advancements in HLA typing and matching |
| 1990s | Increased use of peripheral blood stem cells for transplants |
| 2000s | Development of reduced-intensity conditioning regimens |
BMT has become a key treatment for many diseases. It gives hope to patients all over the world.
The Science Behind Bone Marrow and Its Function
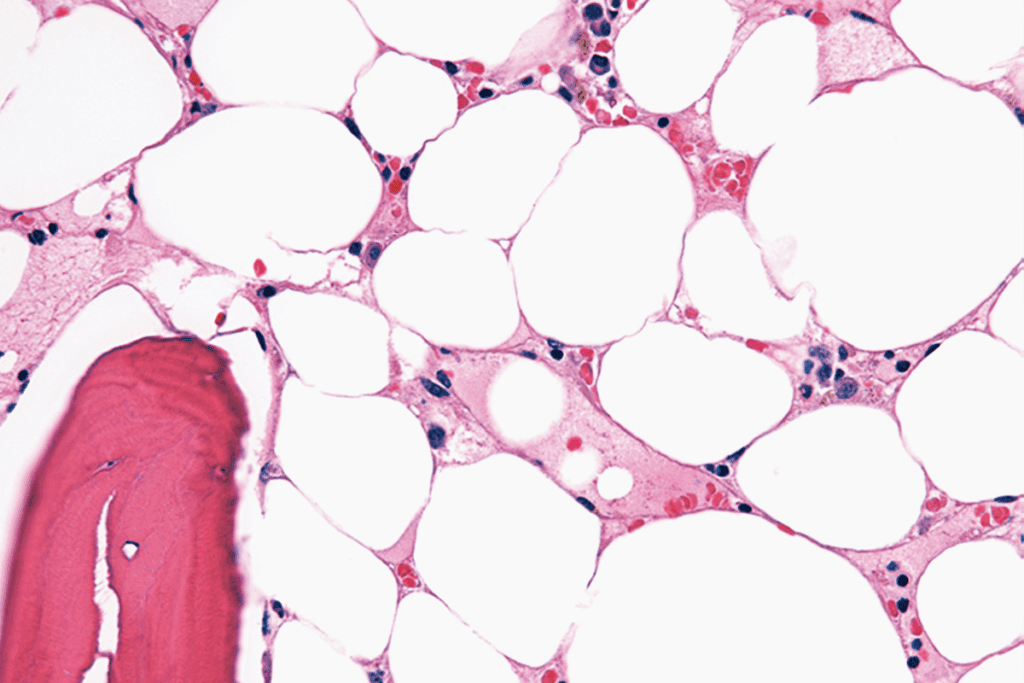
Bone marrow is a spongy tissue in our bones that makes blood cells. It’s where most of our blood cells grow and are kept. It’s key for making red blood cells, white blood cells, and platelets.
What is Bone Marrow?
Bone marrow is soft tissue inside bones, like the hips and thighbones. It makes blood cells. It’s a big part of our body’s blood-making system. The marrow has hematopoietic stem cells that can turn into different blood cells.
Role of Bone Marrow in Blood Cell Production
Bone marrow’s main job is to make blood cells. It creates:
- Red blood cells, which carry oxygen
- White blood cells, part of our immune system
- Platelets, important for blood clotting
It’s vital for keeping our blood cell counts healthy. This ensures our body gets the cells it needs.
Hematopoietic Stem Cells Explained
Hematopoietic stem cells are special in bone marrow. They can turn into any blood cell type. These cells are key to making blood cells and helping our body fight off diseases and injuries.
Knowing how bone marrow works is key to understanding bone marrow transplantation (BMT). BMT replaces a patient’s bad bone marrow with healthy stem cells. It’s used to treat serious diseases like some cancers and blood disorders.
Medical Conditions Treated with BMT
BMT is key in treating many diseases, like some cancers and immune disorders. Doctors choose BMT based on the patient’s health and disease type. We’ll look at the conditions BMT can treat and what decides its use.
Blood Cancers: Leukemia and Lymphoma
BMT is a main treatment for blood cancers like leukemia and lymphoma. These cancers harm blood cells and bone marrow. BMT can cure these by replacing bad cells with good ones. Leukemia makes too many white blood cells. Lymphoma hurts the immune system. BMT has greatly improved survival rates for these patients.
A leading oncologist said,
“BMT has changed the game for blood cancers, giving many patients a second chance.”
Many studies show BMT’s success in fighting leukemia and lymphoma.
Bone Marrow Failure Syndromes
Bone marrow failure, like aplastic anemia, means the marrow can’t make enough blood cells. BMT is a key treatment, replacing the failing marrow with healthy cells. Aplastic anemia is rare, but BMT can save lives.
- Aplastic anemia
- Myelodysplastic syndromes
- Other bone marrow failure conditions
Immune Disorders Responsive to BMT
Some immune disorders can be treated with BMT. These include cases where the immune system is weak or not working properly. BMT replaces the patient’s immune cells with healthy ones from a donor.
Severe Combined Immunodeficiency (SCID) is a condition where kids are born without an immune system. BMT has saved many SCID patients, giving them a working immune system.
Other Conditions Benefiting from BMT
BMT is also used for diseases like multiple myeloma and some genetic disorders. Its versatility makes it a powerful tool against many deadly conditions.
As research grows, more conditions will be treatable with BMT. This brings hope to patients all over the world.
Types of Bone Marrow Transplants
It’s important for patients and their families to know about the different Bone Marrow Transplants. This knowledge helps them choose the best treatment.
Bone Marrow Transplantation (BMT) is a flexible treatment. It can be adjusted to fit each patient’s needs. The choice of BMT depends on the patient’s disease, the availability of a donor, and their health.
Autologous Transplants: Using the Patient’s Own Cells
Autologous transplants use the patient’s own stem cells. This method is often used for certain cancers like multiple myeloma or lymphoma. It helps restore the bone marrow when it’s damaged by disease.
Allogeneic Transplants: Donor-Derived Cells
Allogeneic transplants use stem cells from a donor. This donor can be a family member or someone unrelated. It’s used for patients with leukemia or blood disorders. The donor’s stem cells replace the patient’s diseased bone marrow.
Haploidentical Transplants
Haploidentical transplants use stem cells from a half-matched relative. This is usually a parent, child, or sibling. It’s a good option when a fully matched donor is not available.
Umbilical Cord Blood Transplants
Umbilical cord blood transplants use stem cells from a newborn’s umbilical cord. This is an alternative for patients without a suitable adult donor.
The following table summarizes the key characteristics of the different types of BMT:
| Type of BMT | Donor Source | Typical Use |
| Autologous | Patient’s own cells | Cancers like multiple myeloma or lymphoma |
| Allogeneic | Family member or unrelated donor | Leukemia, other blood disorders |
| Haploidentical | Half-matched relative | When a fully matched donor is not available |
| Umbilical Cord Blood | Umbilical cord of a newborn | Alternatively, when an adult donor is not available |
Each type of BMT has its own benefits. It’s important to understand these differences to make the best treatment choice.
Donor Selection and Matching Process
Finding a compatible donor is the first step towards a successful BMT. This process is key because how well the donor and recipient match affects the transplant’s success.
HLA Typing and Compatibility Factors
HLA typing is a key step in matching donors and recipients. HLA genes help our immune system fight off infections. Matching these genes is important to lower the risk of graft-versus-host disease (GVHD), a serious transplant complication. HLA typing tests for specific genetic markers on white blood cells.
The HLA system is complex, with many genes to match. Important genes for BMT include HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQB1. A good match at these genes is key to avoiding GVHD and ensuring the transplant works.
Finding a Match: Family Members vs. Donor Registries
After finding out the patient’s HLA type, the search for a donor starts. Donors can be family members or unrelated donors from registries. Siblings have the best chance of being a match, with a 25% chance of being HLA-identical. If no sibling match is found, other family members or unrelated donors are considered.
Donor registries, like the National Marrow Donor Program (NMDP), have a database of donors. These registries are vital for patients without a matched family member. They search the registry for a donor with the right HLA type.
| Donor Type | Chance of Match | Advantages | Disadvantages |
| Sibling | 25% | High chance of match, potentially lower risk of GVHD | Limited availability, emotional involvement |
| Unrelated Donor | Varies | Large pool of donors, diverse HLA types | Higher risk of GVHD, longer search |
The Importance of Diverse Donor Pools
Having a diverse donor pool is key for patients from different ethnic backgrounds. Patients from ethnic minorities often struggle to find a match because their HLA types are underrepresented. Increasing diversity in donor registries is vital to help these patients.
There are efforts to recruit donors from diverse backgrounds. This includes campaigns and outreach to encourage people from different ethnic groups to register as donors.
The BMT Procedure: Step-by-Step Process
The Bone Marrow Transplant (BMT) procedure is complex. It involves several key steps for success. We’ll walk you through from the start to the stem cell transplant.
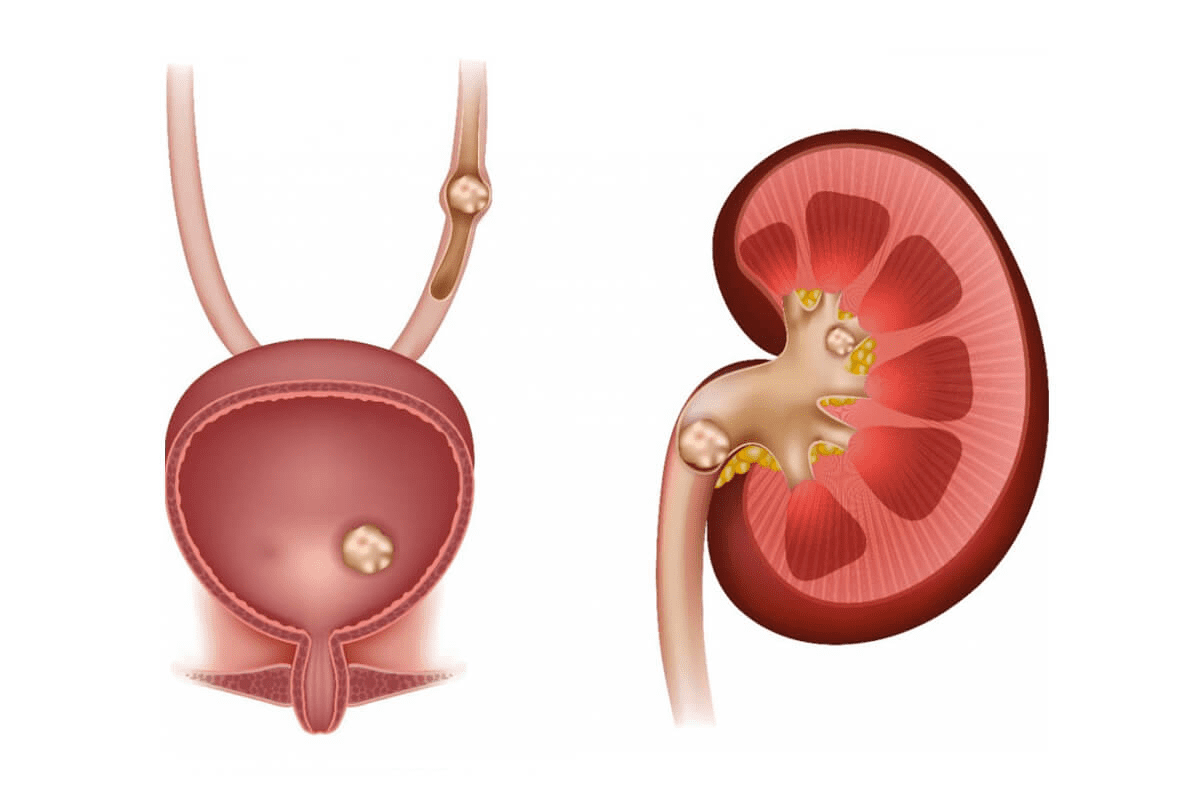
Pre-Transplant Evaluation and Testing
Before a BMT, patients get a detailed check-up. This is to see if they’re healthy enough for the transplant. Tests like blood work and imaging studies are done to find any risks.
Key tests include:
- Blood typing and cross-matching
- Infectious disease screening
- Organ function tests (liver, kidney, heart, and lung function)
- Disease status evaluation
Conditioning Regimen: Preparing the Body
The conditioning regimen is a key part of BMT. It uses high-dose chemotherapy and/or radiation to clear out old bone marrow. This makes room for new stem cells and stops the body from rejecting them.
The conditioning regimen has two main goals:
- Eradicate malignant cells or diseased bone marrow
- Suppress the immune system to prevent graft rejection
| Conditioning Regimen Component | Purpose |
| Chemotherapy | Eradicate diseased cells and suppress the immune system |
| Radiation Therapy | Kill malignant cells and further suppress the immune system |
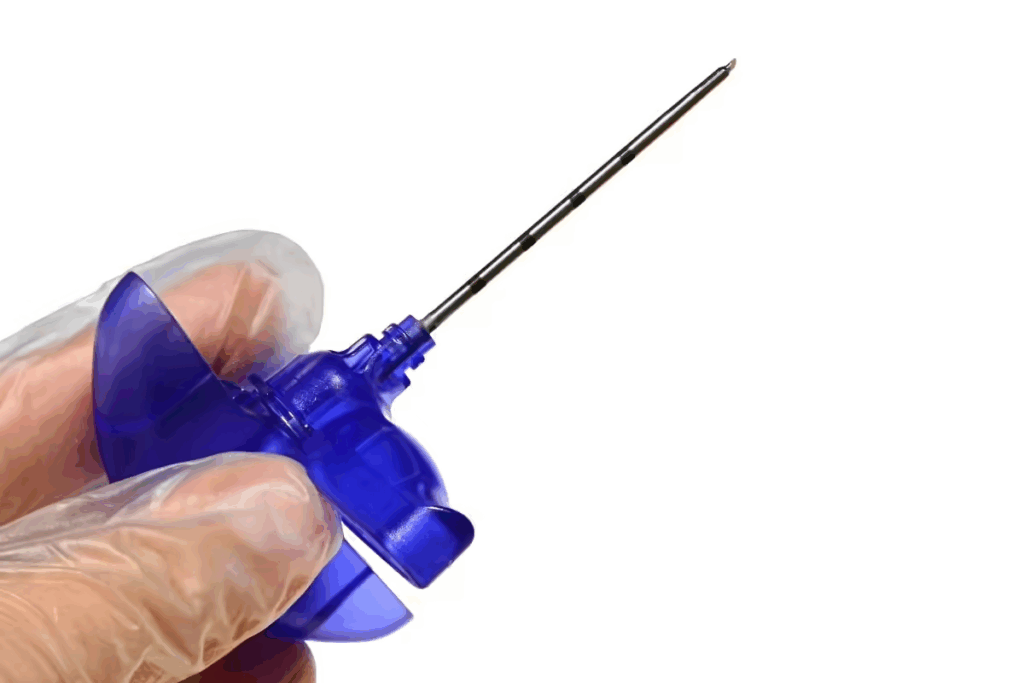
Stem Cell Collection Methods
Stem cells can be collected in different ways. For autologous transplants, they’re taken from the patient before treatment. For allogeneic transplants, they come from a donor.
Common stem cell collection methods include:
- Peripheral blood stem cell collection (most common method)
- Bone marrow harvest
- Umbilical cord blood collection
The Transplantation Process
The transplant process involves putting stem cells into the patient’s bloodstream. This is done through an intravenous line and takes a few hours.
After infusion, the stem cells go to the bone marrow. There, they start making new blood cells. Recovery signs usually appear in a few weeks.
Bone Marrow Collection: Methods and Experience
Collecting bone marrow for transplant uses different methods. Each method has its own benefits. Bone marrow is often taken through a simple blood draw after stem cells are moved into the blood. We’ll look at the various ways to collect bone marrow and what donors and patients go through.
Traditional Bone Marrow Harvest
Traditional bone marrow harvest takes stem cells directly from the bone marrow, usually from the hip. This is done under general or local anesthesia to reduce pain. The bone marrow is then processed to get the stem cells ready for transplant.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is more common. It uses apheresis to separate stem cells from blood. The donor’s stem cells are first moved into the blood with medicine. Then, a special device collects the stem cells while returning the rest of the blood.
Is BMT Painful? Patient and Donor Experiences
While most find the process okay, some might feel pain or discomfort. Doctors use pain management to help. For peripheral blood stem cell collection, some donors might feel bone pain or tiredness from the mobilization medicine.
Here’s a comparison of the two main bone marrow collection methods:
| Collection Method | Description | Potential Side Effects |
| Traditional Bone Marrow Harvest | Surgical extraction of stem cells from bone marrow | Pain at the harvest site, fatigue |
| Peripheral Blood Stem Cell Collection | Apheresis after stem cell mobilization | Bone pain, fatigue, and possible side effects from mobilization medicine |
Knowing about bone marrow collection methods and experiences can ease worries. Whether it’s a traditional bone marrow harvest or a peripheral blood stem cell collection, the aim is the same: to give healthy stem cells for a successful transplant.
How BMT Works as a Cure
BMT can cure life-threatening diseases by rebuilding the immune system and making healthy blood cells. This complex process involves several key steps. These steps work together to cure diseases.
Reconstituting the Immune System
After a BMT, stem cells move to the bone marrow. There, they start making new blood cells. This rebuilds the immune system, helping it fight infections and cancer cells.
Replacing Diseased Cells with Healthy Ones
BMT can cure diseases by replacing bad bone marrow with healthy stem cells. This is key for patients with blood cancers or bone marrow failure. It lets the body make healthy blood cells and can help get rid of the disease.
The table below shows how BMT replaces diseased cells:
| Disease Category | Benefits of BMT | Outcome |
| Blood Cancers | Replaces cancerous cells with healthy stem cells | Potential cure |
| Bone Marrow Failure | Restores healthy blood cell production | Improved survival rates |
| Immune Disorders | Reconstitutes the immune system | Enhanced immune function |
The “Graft-versus-Tumor” Effect
The “graft-versus-tumor” effect is a big plus of allogeneic BMT. It happens when the donor’s immune cells attack cancer cells left behind. This is very helpful in treating blood cancers, as it can kill off any cancer cells left and lower the chance of the disease coming back.
The graft-versus-tumor effect is a key factor in the curative power of BMT. It makes BMT a valuable treatment for patients with certain cancers.
Potential Complications and Risks of BMT
BMT offers hope for many patients, but it comes with risks. It’s important to know these risks and how to prevent them. BMT care focuses on watching for complications and preventing infections.
Graft-Versus-Host Disease (GVHD)
Graft-Versus-Host Disease is a big risk with allogeneic BMT. It happens when the donor’s immune cells attack the recipient’s body. GVHD can affect the skin, liver, and gut.
Symptoms of GVHD can range from mild to severe. They include skin rashes, diarrhea, and liver problems. To manage GVHD, doctors use special medicines and keep a close eye on patients.
Infection Risks During Recovery
After BMT, patients face a high risk of infections. Their immune systems are weak, making them more susceptible to infections.
- Infection prevention strategies are key.
- Doctors use antibiotics and antivirals to prevent infections
- Patients are often kept isolated to reduce exposure to germs
Organ Damage and Other Side Effects
BMT can harm organs. The treatment before the transplant can be toxic to the heart, lungs, and liver.
| Organ | Potential Side Effects |
| Heart | Cardiac dysfunction, heart failure |
| Lungs | Pneumonitis, pulmonary fibrosis |
| Liver | Veno-occlusive disease, liver failure |
Long-Term Health Considerations
Survivors of BMT may face long-term health problems. These include infertility, secondary cancers, and chronic conditions. It’s important to have ongoing care to manage these risks.
“Long-term survivors of BMT require careful monitoring for late effects, including secondary malignancies and organ dysfunction.”
Understanding these risks helps patients and doctors work together. This way, they can reduce complications and ensure the best outcomes.
BMT Care and Recovery Process
After BMT, patients start a key recovery phase. They need full care and support. This phase is vital for handling complications and aiding recovery.
Hospital Stay Duration and Protocols
The time a patient stays in the hospital after BMT changes based on their health and transplant type. Usually, patients stay 2-4 weeks for close watch and early recovery. We stick to strict rules to cut down infection risks and manage any issues.
Infection Prevention Strategies
Stopping infections is a major focus during BMT recovery. We use strict hygiene, isolation, and antibiotics to lower infection risks. Patients learn how to avoid infections, too.
Nutritional Support During Recovery
Nutrition is key in BMT recovery. Patients need a balanced diet full of nutrients to heal. We guide on what to eat and might suggest supplements.
Physical and Emotional Rehabilitation
Recovering physically and emotionally is important after BMT. We offer physical therapy and counseling to help patients get strong and deal with emotional challenges. This support helps patients get the best results and live better lives.
Conclusion: The Life-Changing Impact of BMT
Bone Marrow Transplantation (BMT) has changed the game for treating serious diseases. It gives patients a second chance at life, replacing sick bone marrow with healthy stem cells. This can cure or greatly improve life for many.
The effects of BMT are truly life-changing. Many patients live longer and healthier lives after it. As medical science grows, so will BMT’s benefits, bringing hope to more families.
BMT can cure some diseases and put others into remission. This greatly improves life for many patients. With ongoing progress in BMT, patients now have a brighter future ahead, free from their past health issues.
FAQ
What is BMT in medical terms?
BMT stands for Bone Marrow Transplant. It’s a procedure that saves lives. It treats serious diseases like some cancers and blood disorders.
What is the difference between autologous and allogeneic BMT?
Autologous BMT uses the patient’s own stem cells. Allogeneic BMT uses stem cells from a donor.
What medical conditions are treated with BMT?
BMT treats blood cancers like leukemia and lymphoma. It also helps with bone marrow failure, immune disorders, and other conditions.
How is a BMT donor selected and matched?
Donors are chosen through HLA typing and compatibility tests. This can be a family member or an unrelated donor from a registry.
Is BMT painful for the donor?
Pain levels vary. Traditional bone marrow harvest can be painful. But, peripheral blood stem cell collection might only cause mild side effects.
What is the BMT procedure like?
The BMT process starts with an evaluation. Then, there’s a conditioning regimen and stem cell collection. The transplant follows.
What are the possible complications of BMT?
Complications include graft-versus-host disease (GVHD) and infection risks. There’s also a chance of organ damage and other side effects.
How does BMT work as a cure for certain diseases?
BMT replaces diseased cells with healthy ones. It reconstitutes the immune system. It also uses the “graft-versus-tumor” effect to fight cancer.
What is involved in BMT care and recovery?
Care and recovery include a hospital stay and infection prevention. Nutritional support and physical and emotional rehabilitation are also part of it.
Can BMT be used to treat non-cancerous conditions?
Yes, BMT can treat non-cancerous conditions. This includes bone marrow failure syndromes and immune disorders.
References
- Thomas, E. D., & Blume, K. G. (2023). Bone marrow transplantation: a review. PubMed Central. https://pubmed.ncbi.nlm.nih.gov/10595758/