
Acute myeloid leukemia (AML) is a serious blood cancer that hits children hard. It makes up about 20 percent of leukemia cases in kids. At Liv Hospital, we know how tough it is for families with this disease. We’re here to give top-notch care and support to patients from around the world.
Spotting symptoms early is key to beating AML. We’re all about quick diagnosis and the newest treatments to boost survival chances. Our team of pediatric oncology experts is known worldwide. They make sure our young patients get the best care possible.
Key Takeaways
- AML is an aggressive blood cancer that requires prompt treatment.
- Liv Hospital offers complete support for international patients.
- Early symptom recognition is vital for effective treatment.
- Our pediatric oncology team is internationally recognized.
- We provide timely diagnosis and the latest treatment protocols.
Understanding AML in Children: An Overview
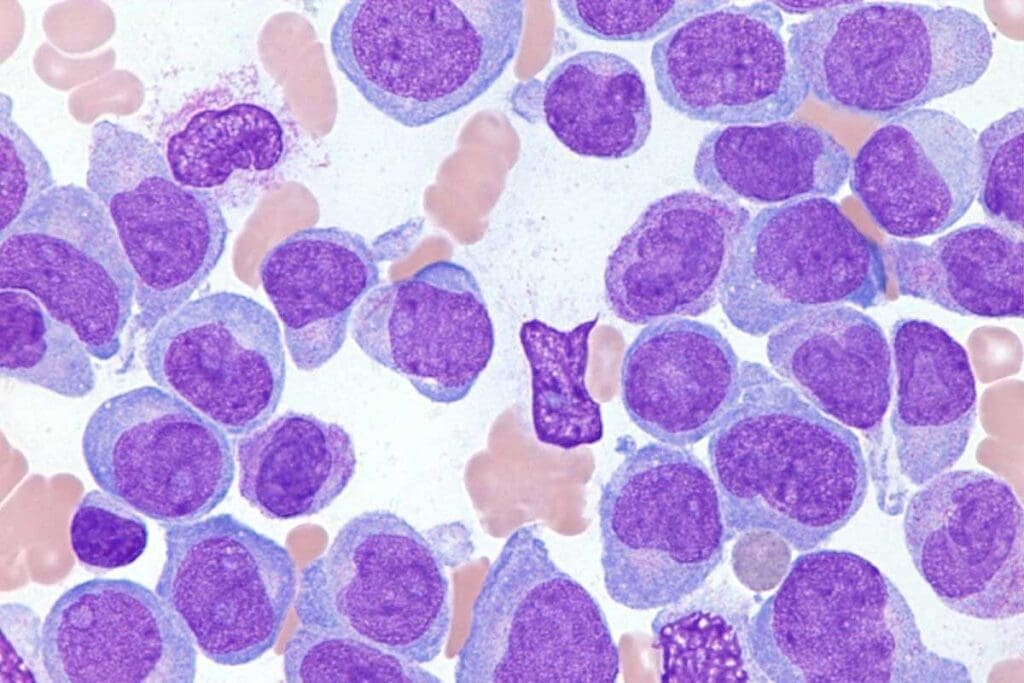
It’s important to know about Acute Myeloid Leukemia (AML) in kids to catch it early and treat it well. AML happens when a bone marrow cell turns cancerous. This leads to too many immature cells that don’t work right.
What is Acute Myeloid Leukemia?
AML is a blood and bone marrow cancer. It makes the bone marrow make bad white blood cells. These bad cells stop normal blood cells from being made.
This can cause infections, anemia, and bleeding problems. AML makes bad cells grow fast. If not treated fast, it can get worse.
Prevalence and Incidence Rates
AML is rare in kids, making up 5-10% of childhood leukemias. It happens in about 5-7 kids per million each year under 20.
The chance of getting AML changes with age. It’s more common in babies under 2 and in late teens. Knowing this helps find and treat it early.
Key statistics on AML incidence in children:
- 5-7 cases per million per year in children under 20
- Higher incidence in infants under 2 years old
- Smaller peak in late adolescence
How AML Differs from Other Childhood Leukemias
AML is different from Acute Lymphoblastic Leukemia (ALL), which is more common. AML affects myeloid cells, while ALL affects lymphoid cells.
Treatment and outlook for AML and ALL also vary. AML needs stronger chemotherapy and responds differently than ALL.
Main differences between AML and ALL:
- Cell lineage: AML affects myeloid cells, while ALL affects lymphoid cells
- Treatment approach: AML requires more intensive chemotherapy
- Prognosis: AML generally has a poorer prognosis than ALL in children
Common Signs and Symptoms of Childhood AML

It’s important to know the signs of Acute Myeloid Leukemia (AML) in kids. This knowledge helps get them the right care early. Early treatment is key to better chances of beating pediatric AML.
Physical Symptoms: Fatigue, Pallor, and Bruising
Kids with AML might show signs that are not always easy to spot. Look out for:
- Fatigue: Feeling very tired that doesn’t get better with rest.
- Pallor: Skin that looks pale because of fewer red blood cells.
- Bruising: Easy bleeding or bruising, like frequent nosebleeds or gum bleeding.
AML messes with blood cell making, leading to a lack of healthy ones. This means less red blood cells for energy and less platelets for stopping bleeding.
Recurrent Infections and Fever
Kids with AML often get sick more often and have fevers. Their immune system is weak because AML affects white blood cells. This can cause:
- Frequent infections: Like pneumonia, urinary tract infections, or skin infections.
- Fever: Unexplained fevers that keep coming back.
These signs are scary for kids because their immune systems are growing. Watch your child’s health closely and get help if symptoms don’t go away.
Bone Pain and Other Musculoskeletal Symptoms
Kids with AML might also have bone and joint pain. Leukemia cells in bones and joints can hurt. Some symptoms include:
- Bone pain: Severe pain in bones or joints.
- Joint pain: Swelling or pain in the joints.
These symptoms can really affect a child’s life. If they keep happening, it’s important to see a doctor.
When to Seek Medical Attention
If your child shows any of these signs, get them to a doctor fast. Early treatment is very important for kids with AML.
| Symptom | Description | Action |
| Fatigue and Pallor | Persistent tiredness and pale skin | Consult a pediatrician if symptoms persist |
| Bruising and Bleeding | Easy bruising or frequent bleeding | Seek immediate medical attention if severe |
| Recurrent Infections and Fever | Frequent infections or unexplained fevers | Consult a pediatrician for evaluation |
| Bone and Joint Pain | Severe pain in bones or joints | Seek medical evaluation to rule out AML |
Diagnostic Process for AML in Children
When a child might have Acute Myeloid Leukemia (AML), doctors use many tools to check. They do tests to find out what kind of leukemia it is. This is key to picking the right treatment.
Initial Blood Tests and Examinations
The first step is initial blood tests. These look for odd levels of white and red blood cells, and platelets. They hint at leukemia, but more tests are needed to be sure.
A complete blood count (CBC) is often the first test. It checks the levels of different blood cells. It can show signs of leukemia.
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy and aspiration are key for AML diagnosis. They take a bone marrow sample for a closer look. The sample shows if leukemia cells are there, what they look like, and how widespread the disease is.
Genetic and Molecular Testing
Genetic and molecular testing are very important for AML diagnosis. They find specific genetic changes in leukemia cells. These changes help decide treatment and how likely the child is to recover.
Classification and Staging of Pediatric AML
After diagnosing, the next step is to classify and stage the AML. This means figuring out the exact type of AML and how far it has spread. Knowing this helps doctors create a treatment plan that fits the child’s needs.
Age-Related Differences: From Infants to Adolescents
It’s key to know how Acute Myeloid Leukemia (AML) shows up in kids of different ages. AML is complex, and how it looks can change a lot from infancy to being a teenager.
Unique Characteristics of Infant AML
Infant AML is when kids under 1 get this disease. It often has high white blood cell counts and special genetic changes, like MLL gene rearrangements. These changes help decide how to treat the disease.
Studies show infant AML reacts differently to treatment than older kids. So, doctors have made special treatment plans for this age group.
AML in School-Age Children
School-age kids with AML might feel tired, look pale, and bruise easily. Their disease can be like adults’, with certain genetic changes more common.
Thanks to better treatments and care, kids in school age have better chances of beating AML. But, it’s a tough disease, and doctors keep looking for the best ways to fight it.
Adolescent AML Presentations
Teenagers with AML often have symptoms and disease traits like young adults. Their disease can be aggressive, so treatment plans consider their health and future risks.
Research shows teens with AML can do well with strong treatments, like chemotherapy and sometimes stem cell transplants. The aim is to cure them while avoiding lasting harm.
Age as a Prognostic Factor
Age is a big factor in AML, affecting how well treatment works and survival chances. Infants and teens often face different outcomes than school-age kids. This shows the need for treatments tailored to each age group.
The table below shows the main differences in AML by age:
| Age Group | Common Characteristics | Prognosis |
| Infants (<1 year) | High WBC count, MLL gene rearrangements | Variable, often challenging to treat |
| School-age Children | Symptoms like fatigue, pallor, bruising | Generally better than infants, with improving survival rates |
| Adolescents | Aggressive disease, similar to young adults | Can benefit from intensive treatment, with a focus on minimizing long-term toxicity |
Knowing these age differences helps doctors give the best care for each child with AML. This can lead to better results for kids with this disease.
Treatment Approaches for Pediatric Acute Myeloid Leukemia
Treating pediatric Acute Myeloid Leukemia (AML) is complex. It uses many strategies to help kids get better. We’ll look at intensive chemotherapy, stem cell transplants, targeted treatments, and supportive care.
Intensive Chemotherapy Protocols
Intensive chemotherapy is key in treating pediatric AML. It uses strong drugs to kill cancer cells. The treatment goes through many cycles, lasting days to weeks. The aim is to clear leukemia from the bone marrow and blood.
A study in a top medical journal shows intensive chemotherapy boosts survival rates for kids with AML.
“Intensive chemotherapy regimens have become the standard of care for pediatric AML, improving outcomes and survival rates.”
– Journal of Pediatric Hematology/Oncology
Stem Cell Transplantation Indications and Process
Stem cell transplants are for kids with high-risk AML or those who’ve relapsed. It replaces bad bone marrow with healthy stem cells from a donor. This can get rid of leftover leukemia cells and lead to long-term remission.
| Indication | Description |
| High-risk AML | Children with high-risk genetic features or those who have not responded to initial chemotherapy |
| Relapsed AML | Children who have experienced a relapse after initial treatment |
Targeted Therapies and Emerging Treatments
Targeted therapies are being tested to improve AML treatment for kids. They target specific genetic changes in leukemia cells. New treatments like immunotherapy are also being looked into for better results.
Supportive Care During Treatment
Supportive care is vital during AML treatment. It helps manage side effects and improves the child’s life quality. This includes nutrition, infection prevention, and counseling.
With full supportive care, we can help kids face AML treatment challenges and achieve better results.
Survival Rates and Prognosis Factors
Medical treatments have improved a lot for kids with AML. This gives hope to families. We’ll look at how well kids with AML are doing now. We’ll also talk about what affects their chances of getting better.
Current Five-Year Survival Statistics
The five-year survival rate for kids with AML has gone up. It’s now between 65 and 75 percent. This better rate comes from new treatments like strong chemotherapy and stem cell transplants.
We’ve learned a lot about AML. This knowledge helps us treat it more effectively.
Differences in Survival Rates by Age Group
Age is very important for kids with AML. Babies under one and teens have different chances of getting better. Kids between 1 and 9 years old usually have a better outlook.
We need to think about age when we plan treatment. This helps us predict how well a child might do.
Impact of AML Subtype on Prognosis
The type of AML also affects how well a child will do. Some types, like acute promyelocytic leukemia (APL), are easier to treat. Others might need stronger treatments.
Knowing the exact type of AML is key. It helps us choose the best treatment for each child.
Recent Improvements in Survival Outcomes
In the last few decades, survival rates for kids with AML have gotten better. New tests help us understand AML better. This means we can treat it more precisely.
New medicines and better care have also helped. We keep working to make care even better for kids with AML.
| Age Group | Five-Year Survival Rate |
| Infants (<1 year) | 50-60% |
| Children (1-9 years) | 70-80% |
| Adolescents (10+ years) | 60-70% |
These numbers show why we need to keep researching and treating each child as an individual. This way, we can help all kids with AML, no matter their age or type of AML.
Long-Term Effects and Follow-Up Care
Survivors of pediatric Acute Myeloid Leukemia (AML) often face long-term effects. These effects need careful management. Treatment for AML has improved, focusing now on better quality of life for survivors.
We will talk about the late effects of AML treatment. We’ll also cover the importance of monitoring and follow-up care. Plus, the need for psychosocial support will be highlighted.
Potential Late Effects of AML Treatment
Pediatric AML survivors may face various late effects. These can come from intensive chemotherapy and other treatments. Some of these effects include:
- Organ Damage: Chemotherapy and radiation can harm organs like the heart, lungs, and kidneys.
- Secondary Cancers: There’s a higher risk of getting secondary cancers, which means long-term surveillance is needed.
- Growth and Development Issues: Children might experience growth delays or developmental problems.
- Fertility Concerns: Treatment can affect fertility, making it key to discuss fertility preservation options.
Monitoring and Follow-Up Protocols
Regular follow-up care is key for early detection and management of late effects. This includes:
- Regular Check-Ups: Survivors should see their healthcare provider regularly to monitor for late effects.
- Screening Tests: Tests like echocardiograms and blood tests help detect issues early.
- Risk-Based Care: Care plans are tailored based on treatments received and individual risk factors.
Psychosocial Support for Survivors
Survivors of pediatric AML and their families often need psychosocial support. This support helps them cope with emotional and psychological challenges. It includes:
- Counseling: Individual or family counseling helps with anxiety, depression, and other emotional issues.
- Support Groups: Joining support groups connects survivors with others facing similar challenges.
Quality of Life Considerations
Improving the quality of life for pediatric AML survivors is a complex effort. It involves managing late effects, providing psychosocial support, and ensuring access to resources. By focusing on these areas, we can enhance survivors’ overall well-being.
The Importance of Early Recognition of Child Leukemia Symptoms
Spotting leukemia symptoms early is key for better treatment and survival chances. Knowing the signs of leukemia in kids is vital. Early detection can greatly improve treatment success.
Impact of Early Diagnosis on Treatment Outcomes
Diagnosing Acute Myeloid Leukemia (AML) early means better treatment plans. Early detection means higher chances of successful treatment. This might also mean less harsh treatments.
Early diagnosis brings many benefits:
- It leads to better treatment results because of timely action
- It lowers the risk of serious problems from advanced leukemia
- It improves life quality during treatment
Educating Parents and Caregivers
Teaching parents and caregivers about leukemia symptoms is essential. They need to know when to seek medical help. This includes signs like persistent tiredness, unexplained bruises, and frequent infections.
Knowing these symptoms helps parents get medical help fast. This can lead to an earlier diagnosis. Key symptoms to watch for are:
- Persistent tiredness or weakness
- Unexplained bruising or bleeding
- Recurring infections or fever
The Role of Primary Care Providers
Primary care providers are vital in catching leukemia early. We count on them to spot early signs during check-ups. They also refer kids to specialists when needed.
Being alert and knowing leukemia symptoms helps primary care providers. This can greatly reduce delays in diagnosis.
Reducing Diagnostic Delays
Shortening diagnostic times is essential for better leukemia treatment in kids. We need to work together to ensure kids get diagnosed quickly. This allows them to start treatment without delay.
Ways to cut down diagnostic delays include:
- Boosting awareness of leukemia symptoms among healthcare providers and parents
- Making the diagnostic process faster to ensure quick referrals to specialists
- Improving communication between healthcare teams and families
By using these strategies, we aim for earlier diagnosis and better treatment of childhood leukemia.
Conclusion: Advances in Childhood AML Care
Advances in AML care have greatly improved survival rates for kids with Acute Myeloid Leukemia. At Liv Hospital, we aim to give top-notch healthcare. We also support international patients fully.
We talked about AML in kids, including symptoms, treatments, and survival chances. We stressed the need to spot symptoms early. We also highlighted our support services.
Treatment for kids with AML has grown, with new methods like intensive chemotherapy and stem cell transplants. We keep working to improve care and outcomes for these children.
We’re committed to top-notch treatment for kids with AML. Our goal is to better the lives of our young patients and their families. Our dedication to AML care in kids is strong, and we aim to make a difference globally.
FAQ
What are the common symptoms of Acute Myeloid Leukemia (AML) in children?
Symptoms of AML in kids include feeling very tired, looking pale, and bruising easily. They might also get sick a lot, have fever, or pain in their bones. If your child shows any of these signs, get them to a doctor right away.
How is AML diagnosed in children?
Doctors use blood tests, bone marrow biopsies, and genetic tests to find AML in kids. These tests help figure out if your child has AML and what type it is.
What are the treatment approaches for pediatric AML?
Kids with AML might get chemotherapy, a stem cell transplant, or special medicines. The treatment plan depends on the child’s age, the type of AML, and other factors.
What are the survival rates for children with AML?
Survival rates for kids with AML vary based on age and type of AML. Thanks to better treatments, more kids are living longer. But, some types of AML are harder to treat.
How does age affect the prognosis of AML in children?
Age is very important when it comes to AML in kids. Babies and teens have different types of AML and outcomes. Knowing this helps doctors plan better treatments.
What are the possible late effects of AML treatment in children?
AML treatment can cause damage to organs, increase the risk of other cancers, and affect a child’s mental health. It’s important to keep an eye on these effects over time.
How can parents and caregivers reduce diagnostic delays for child leukemia symptoms?
Parents and caregivers can help by knowing the signs of leukemia and acting fast. They should also push for their child to get the care they need. Doctors play a big role in spotting symptoms and sending kids to specialists.
What is the role of supportive care during AML treatment?
Supportive care helps manage side effects, prevent infections, and keep kids feeling good. This includes helping with nutrition, pain, and mental health.
Are there any new and emerging treatments for pediatric AML?
Yes, new treatments like targeted therapies and immunotherapies are being developed for AML in kids. These aim to improve results and reduce harm.
How can families access complete support services for children with AML?
Families can find help by talking to their doctor or contacting a place like Liv Hospital. They offer support with nutrition, mental health, and ongoing care.
Reference
- National Cancer Institute. (2024). Childhood Acute Myeloid Leukemia Treatment (PDQ®) – Health Professional Version.https://www.cancer.gov/types/leukemia/patient/child-aml-treatment-pdq



































