Last Updated on November 20, 2025 by Ugurkan Demir
Pediatric acute myeloid leukemia is a serious cancer in kids. It’s a big part of childhood cancers. Knowing about survival rates is key for families and doctors to get the best care.
The National Cancer Institute says treatment for this cancer includes strong chemotherapy. Sometimes, a stem cell transplant is needed. At Liv Hospital, we focus on you, using the newest research and treatments.
Key Takeaways
- Understanding survival rates helps families and healthcare providers make informed decisions.
- Pediatric acute myeloid leukemia treatment involves intensive chemotherapy.
- Stem cell transplantation is sometimes necessary for treatment.
- Liv Hospital provides a patient-centered approach to care.
- The latest research and innovative therapies are key for better survival rates.
What is Pediatric Acute Myeloid Leukemia?
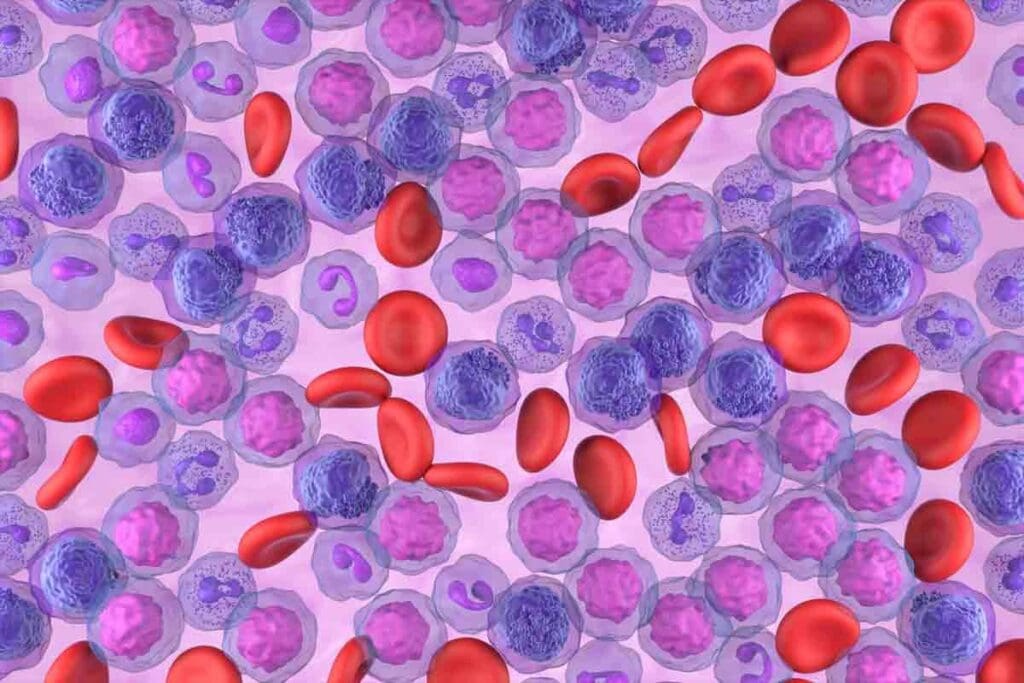
Childhood AML is a cancer that starts in the bone marrow and spreads quickly to the blood. It happens when abnormal white blood cells grow fast. These cells fill the bone marrow and stop normal blood cells from being made.
Definition and Classification
Pediatric AML is sorted by the type of cells it affects and its genetic traits. This sorting helps doctors know how likely it is to get better and what treatment to use. AML is different from Acute Lymphoblastic Leukemia (ALL), which is more common in kids. While ALL makes up about 80% of childhood leukemia, AML is around 15-20%.
Prevalence as the Fifth Most Common Childhood Cancer
The American Cancer Society says AML is the fifth most common cancer in kids. About 500 kids in the U.S. get AML every year. The exact cause of AML is not known, but some genetic conditions and past chemotherapy or radiation are risk factors. Symptoms include tiredness, fever, bruising, and infections, which make parents seek medical help.
Knowing about Pediatric AML’s prevalence and what it is helps with early detection and treatment. By spotting symptoms and risk factors early, doctors can start the right treatment quickly.
Key Fact #1: Current AML Leukemia Pediatric Survival Rates
Pediatric AML survival rates have improved a lot. New medical treatments are helping young patients live longer. Thanks to research and better healthcare, the outlook for kids with AML is getting brighter.
Overall 5-Year Survival Statistics
The 5-year survival rate for kids with AML has gone up. Now, about 65-75 percent of kids in high-income countries survive. This shows how far treatment has come and how well kids are being cared for.
Historical Improvements in Outcomes
Studies show AML survival rates for kids have been getting better over time. Aplenc et al.’s research points to the progress in treating pediatric AML. This progress is thanks to better chemotherapy, stem cell transplants, and care.
Factors Affecting Survival Statistics
Several things can change a child’s AML survival chances. These include:
- Age at diagnosis
- Genetic characteristics of the leukemia
- Response to initial treatment
- Presence of minimal residual disease
Knowing these factors helps doctors create treatment plans that work best for each child.
| Factor | Impact on Survival |
| Age at Diagnosis | Children under 1 year and those over 10 years often have different prognoses. |
| Genetic Characteristics | Favorable genetic markers can significantly improve survival rates. |
| Response to Initial Treatment | Rapid response to induction therapy is associated with better outcomes. |
Key Fact #2: Recognizing Early Warning Signs and Symptoms
It’s important to know the early signs of pediatric AML. Parents and caregivers need to watch for common symptoms.
Common Physical Symptoms
AML symptoms in kids can look like common illnesses. Look out for fatigue, fever, bruising, and frequent infections. These happen because AML messes with blood cell making.
Kids with AML might have bone or joint pain. This is because leukemia cells build up in the bone marrow. They might also have big lymph nodes, spleen, or liver, but this is more common in other leukemias.
When to Seek Medical Attention
If a child keeps getting sick or tired, get them to a doctor. These signs can mean many things, but a doctor can figure out what’s wrong.
Be worried if your child loses weight, has night sweats, or keeps getting sick. These signs, with others, might mean they need a serious check-up.
Importance of Early Diagnosis
Finding AML early is key to better treatment. Early treatment means kids have a better shot at beating the disease.
The National Cancer Institute says spotting AML signs early is key. They offer detailed info on AML symptoms in kids. They stress the need for quick doctor visits if symptoms show up.
Key Fact #3: Standard Treatment Approaches and Success Rates
Children with AML usually get intensive chemotherapy. This treatment has improved a lot. Now, we aim to increase survival rates and lessen long-term side effects.
Intensive Chemotherapy Protocols
Intensive chemotherapy is key for treating pediatric AML. Research shows it works well, helping most kids get into remission after treatment (Source: Tarlock K, Cooper TM. Acute myeloid leukemia: Children and adolescents. UpToDate. 2024). This treatment involves several rounds of strong chemotherapy.
The treatment plan is made just for each child. It depends on their risk level and how they react to treatment. We mix different drugs to kill the leukemia cells.
Stem Cell Transplantation Indications
Stem cell transplantation is for high-risk AML or those not responding to first treatment. It replaces the bone marrow with healthy stem cells, from a donor or the patient’s own cells after treatment.
Choosing stem cell transplantation depends on many things. These include the patient’s health, AML’s genetic makeup, and how they did with first treatment.
70-80% Cure Rate for Low-Risk Patients with Chemotherapy Alone
Low-risk pediatric AML patients can be cured with just chemotherapy. This has a success rate of 70-80%. It shows how effective modern chemotherapy is.
| Treatment Approach | Success Rate | Patient Group |
| Chemotherapy Alone | 70-80% | Low-Risk Patients |
| Stem Cell Transplantation | Variable | High-Risk Patients |
We keep watching and changing treatment plans to help all pediatric AML patients. Thanks to better chemotherapy and stem cell transplantation, kids with AML have a better chance of recovery.
Key Fact #4: AML Prognosis by Age in Pediatric Patients
The outlook for kids with Acute Myeloid Leukemia (AML) changes with age. This affects how we treat them and their chances of getting better. Knowing how age impacts AML is key to better care and survival rates.
Infant AML (Under 1 Year)
AML in babies under 1 year is tough. They often have special genes that make treatment harder. Babies with AML usually face a tougher road than older kids, mainly because of these high-risk genes.
Key challenges in infant AML include:
- Higher incidence of MLL gene rearrangements
- Increased risk of treatment-related toxicity
- Difficulty in administering appropriate chemotherapy doses
Children Aged 1-10 Years (Best Prognosis Group)
Kids aged 1 to 10 have the best chance of beating AML. They often have genes that help them fight the disease better. Standard treatments work well for them.
Factors contributing to better outcomes in this age group:
- Lower incidence of high-risk genetic mutations
- Better tolerance to intensive chemotherapy
- More effective treatment protocols tailored for this age group
Adolescent AML (11-18 Years)
Teens with AML have their own set of challenges. Their outlook is better than infants but not as good as younger kids. Teens might face different genetic risks and treatment responses.
Considerations for adolescent AML patients:
- Increased risk of therapy-related long-term effects
- Potential differences in drug metabolism affecting treatment efficacy
- Psychosocial factors impacting treatment adherence and overall well-being
Age-Specific Treatment Considerations
Treatment for AML in kids depends a lot on their age. We adjust our plans to fit each age group’s needs. This includes how they handle drugs, long-term effects, and their ability to handle tough treatments.
Age-specific treatment considerations include:
| Age Group | Treatment Considerations |
| Infants (<1 year) | Modified chemotherapy doses, careful management of toxicity |
| Children (1-10 years) | Standard intensive chemotherapy protocols |
| Adolescents (11-18 years) | Consideration of late effects, inclusion in clinical trials |
By focusing on how age affects AML and tailoring treatments, we aim to boost survival rates for kids with AML.
Key Fact #5: Genetic Factors Determining Survival Outcomes
Understanding the genetics of pediatric AML is key to predicting survival. Genetic factors greatly influence how children with AML react to treatment and their prognosis.
Favorable Genetic Markers
Certain genetic markers in pediatric AML patients are more favorable. For example, AML with t(8;21) or inv(16) genetic abnormalities tends to respond better to therapy. These genetic traits help guide treatment, leading to more effective care.
High-Risk Genetic Features
On the other hand, some genetic features are high-risk and linked to poor outcomes in pediatric AML. For instance, FLT3 gene abnormalities, like internal tandem duplications (ITD), increase the risk of relapse. Early detection of these high-risk features allows for more aggressive treatment plans.
How Genetic Testing Guides Treatment Decisions
Genetic testing is vital in managing pediatric AML. It helps doctors tailor treatments based on each patient’s genetic profile. This personalized approach has greatly boosted the childhood leukemia survival rate in recent years.
The National Cancer Institute notes that genetic testing helps identify markers in pediatric AML patients. It guides treatment decisions and improves outcomes. As we learn more about AML’s genetics, we can expect even better leukemia survival rates for children.
Key Fact #6: AML Subtypes and Their Distinct Survival Rates
It’s important to know the different types of Acute Myeloid Leukemia (AML) to understand survival rates in kids. AML is a complex disease with many subtypes. Each subtype has its own unique traits and how well it does in treatment.
Some subtypes have better survival rates than others. For example, Acute Promyelocytic Leukemia (APL) has a high cure rate with the right treatment.
Acute Promyelocytic Leukemia (APL)
APL, marked by the PML-RARA gene, has seen big improvements in survival thanks to new treatments. Studies show that APL patients can live over 90% of the time with today’s treatments.
Targeted therapies have greatly improved APL patient outcomes. ATRA and arsenic trioxide are key in treating this subtype.
Core Binding Factor AML
Core Binding Factor AML, with specific genetic changes, has a better outlook than other AML types. These genetic changes help patients achieve complete remission and live longer.
Patients with Core Binding Factor AML often do well with intensive chemotherapy. Their genetic makeup is key to how they respond to treatment.
High-Risk AML Subtypes with Less Favorable Outcomes
On the other hand, some AML subtypes have worse outcomes. These include subtypes with complex genetics, FLT3-ITD mutations, or other high-risk features. These patients often need more aggressive treatments, like stem cell transplants.
The survival rates for these high-risk subtypes are lower than for subtypes like APL or Core Binding Factor AML. We need more research into new treatments to help these patients.
| AML Subtype | Characteristic Genetic Feature | Survival Rate |
| Acute Promyelocytic Leukemia (APL) | PML-RARA fusion | >90% |
| Core Binding Factor AML | t(8;21) or inv(16) | 70-80% |
| High-Risk AML | Complex cytogenetics or FLT3-ITD | 40-50% |
Key Fact #7: Measuring Treatment Response and Remission
It’s important to know how treatment response is measured in pediatric AML. We look at several key indicators to see if treatment is working. This helps us adjust the treatment plan as needed.
Initial Response to Induction Therapy
The first response to treatment is key for kids with AML. Most children get better after the first treatment. This is a big step forward in their fight against cancer. Studies show that how well they do at first is a good sign for their future.
Minimal Residual Disease Monitoring
Checking for minimal residual disease (MRD) is vital in AML. MRD are tiny cancer cells left after treatment. Finding MRD helps us spot who might need extra help. Research shows that watching for MRD can make a big difference in treatment success (Meyran D, Arfeuille C, Chevret S, et al. Haematologica. 2024;109(9):2908-2919).
Relapse Patterns and Post-Relapse Survival
How AML comes back can change, and knowing this helps us plan better. The table below shows important facts about relapse and survival after it happens.
| Relapse Timing | Post-Relapse Survival Rate | Factors Influencing Survival |
| Early Relapse (<1 year) | Lower survival rate | Intensity of initial treatment, genetic factors |
| Late Relapse (>1 year) | Higher survival rate | Duration of first remission, response to second-line treatment |
Long-Term Remission Statistics
Good news: more kids with AML are staying in remission for a long time. Thanks to better treatments, many can live a long, healthy life. We keep tracking these numbers to keep making treatments better.
Advances in Pediatric AML Treatment
New treatments like targeted therapies and immunotherapy are changing how we fight AML in kids. We’ve made big strides in understanding AML in children. This has led to treatments that are more effective and safer.
Targeted Therapies
Targeted therapies are showing great promise in treating AML in kids. They work by focusing on specific genetic changes in leukemia cells. This helps protect healthy cells. For example, drugs targeting the FLT3 mutation have shown good results in trials.
Examples of Targeted Therapies:
- FLT3 inhibitors for patients with FLT3 mutations
- CD33-directed therapies for AML cells expressing CD33
Immunotherapy Approaches
Immunotherapy is another exciting area in AML treatment for kids. It uses the body’s immune system to fight cancer. There are a few ways it works:
- CAR-T cell therapy, which modifies T cells to attack AML cells
- Antibody-based therapies that target specific proteins on AML cells
Promising Clinical Trials
Many clinical trials are testing new treatments for AML in kids. These trials combine targeted therapies and immunotherapies. They’re key to finding the best treatments and improving survival rates.
| Trial Name | Treatment Approach | Target Population |
| Trial ABC | FLT3 inhibitor + chemotherapy | Newly diagnosed AML patients with FLT3 mutation |
| Trial XYZ | CAR-T cell therapy | Relapsed or refractory AML patients |
Impact on Future Survival Rates
New therapies are expected to greatly improve survival rates for kids with AML. These treatments are more effective and less harmful. This means better lives for survivors and higher survival rates.
As research keeps moving forward, we’re hopeful for better outcomes for kids with AML.
Long-Term Effects After Successful Treatment
The journey doesn’t end with treatment completion. Survivors of childhood AML may face long-lasting health issues. These need careful management and monitoring.
Physical Late Effects
Survivors of pediatric AML can face physical late effects from treatment. These may include:
- Cardiac issues, such as heart failure or coronary artery disease, from certain chemotherapy drugs or radiation therapy.
- Endocrine problems, like thyroid dysfunction or growth hormone deficiency.
- Increased risk of secondary cancers due to previous treatments.
Table: Common Physical Late Effects in Pediatric AML Survivors
| Late Effect | Potential Causes | Monitoring Recommendations |
| Cardiac Issues | Anthracycline chemotherapy, radiation to the chest | Regular echocardiograms, cardiovascular risk assessment |
| Endocrine Problems | Radiation to the head or neck, certain chemotherapy agents | Annual thyroid function tests, growth monitoring |
| Secondary Cancers | Previous chemotherapy or radiation therapy | Lifelong surveillance for new cancers |
Cognitive and Psychological Impacts
Pediatric AML survivors may face cognitive and psychological challenges. These include learning, memory, and emotional well-being issues. These can stem from the disease, treatment, or the stress of the experience.
Long-Term Monitoring Requirements
Survivors of pediatric AML need ongoing monitoring. This includes regular follow-up appointments and screenings for late effects. It also involves support for managing any challenges.
Understanding these long-term effects and implementing monitoring and support strategies can improve survivors’ quality of life.
Disparities in Pediatric AML Outcomes
Despite progress in treatment, some groups face worse outcomes in pediatric AML. Factors like income, race, and access to care play big roles. These differences affect how well kids do after being diagnosed.
Socioeconomic Factors
Income level greatly impacts AML outcomes in kids. Families with less money often struggle to get the right care on time. This can hurt their child’s chances of beating the disease.
“Differences in treatment outcomes for children with AML have been observed, with socioeconomic status being a contributing factor.”
Puumala SE, Ross JA, Aplenc R, Spector LG. Pediatr Blood Cancer. 2013;60(5):728-733.
Economic barriers can block access to top treatments and support services. This can make outcomes worse. We need to think about these issues when trying to improve survival rates.
Racial and Ethnic Differences
There are also racial and ethnic differences in AML outcomes. Some groups face lower survival rates. This is due to genetics, environment, and healthcare access.
Cultural factors affect how families seek and stick to treatment. It’s key to understand these differences to help more kids.
Access to Specialized Care
Getting care from experienced teams is vital for better outcomes. But not all families can get to these centers. This is a big problem, mainly in rural or poor areas.
Telemedicine and new ways to deliver care are being tried. They aim to make sure every child gets top-notch care, no matter where they live.
Initiatives to Address Disparities
Many efforts are underway to fix these disparities. These include better access to care, more culturally aware doctors, and support for families. These steps aim to make outcomes fairer for all kids with AML.
By tackling these disparities, we can strive for fairer outcomes for all kids with AML. As we learn more about treating AML, we must make sure everyone benefits equally.
Support Resources for Families Facing Childhood AML
When a child is diagnosed with AML, it can feel overwhelming. Finding support is key for families. Dealing with pediatric AML means facing medical, emotional, financial, and educational challenges.
Financial Assistance Programs
Handling the costs of AML treatment can be tough. Luckily, many groups offer financial help. This includes covering medical bills, travel, and staying costs. For example, the Children’s Cancer and Blood Foundation helps families with childhood cancer, including AML.
Emotional Support Networks
Emotional support is essential for families with AML. There are support groups, counseling, and online forums. These connect families with others facing similar challenges. The CureSearch for Children’s Cancer offers resources and support for families with childhood cancer.
Educational Resources
Knowing about pediatric AML helps families make better treatment choices. There are many educational resources available. These include brochures, websites, and workshops. The American Cancer Society is a great source of information and support for families with cancer.
Clinical Trial Information
Clinical trials are important for finding new treatments for AML. Families can find out about trials on ClinicalTrials.gov. These trials offer new treatments that could help children with AML.
By using these support resources, families can better handle the challenges of AML. We suggest families look into these options to find the right support for them.
Conclusion: The Evolving Landscape of Pediatric AML Survival
Looking back, we see big steps forward in treating pediatric acute myeloid leukemia. New ways to care for kids with this disease have raised survival hopes. This shows that we’re getting better at fighting this tough illness.
New studies and treatments are on the horizon. The National Cancer Institute says we’re close to making things even better for kids. They’re looking into special medicines and ways to boost the immune system.
Dealing with pediatric AML is tough, but there’s always hope. We’re all working together to make treatments better. We want to make sure every family gets the support they need during this hard time.
Our goal is to keep improving how we treat acute myeloid leukemia in kids. We want every child to have a good chance of beating this disease and living a full life.
FAQ
What is pediatric Acute Myeloid Leukemia (AML)?
Pediatric AML is a cancer that affects kids’ blood and bone marrow. It’s when abnormal white blood cells grow too fast. These cells fill the bone marrow and stop normal blood cells from being made.
What are the common symptoms of pediatric AML?
Kids with AML might feel tired, look pale, and get sick often. They might bruise easily or have pain in their bones or joints. They could also lose weight, have a fever, or not want to eat.
How is pediatric AML diagnosed?
Doctors use a few ways to find AML in kids. They do a physical check, blood tests, a bone marrow biopsy, and imaging studies. They look for abnormal cells in the bone marrow or blood to confirm the diagnosis.
What are the current survival rates for pediatric AML?
The 5-year survival rate for kids with AML is about 60-70%. But, survival can change based on age, genetics, and how well the treatment works.
How does age affect the prognosis of pediatric AML?
Age plays a big role in AML’s outlook. Babies under 1 year face a tough time, but kids 1-10 years old have a better chance. Teens 11-18 years old usually fall in between.
What are the genetic factors that influence survival outcomes in pediatric AML?
Some genetic traits can help kids with AML live longer. But, other traits can make it harder. Genetic tests help doctors choose the best treatment.
What are the standard treatment approaches for pediatric AML?
Kids with AML usually get strong chemotherapy. Sometimes, they also get a stem cell transplant. The goal is to get rid of the cancer and keep it from coming back.
What are the long-term effects of successful treatment for pediatric AML?
Kids who beat AML might face long-term issues. They could have physical problems, trouble with thinking or feeling, or a higher risk of getting cancer again. It’s important to keep an eye on them over time.
Are there any disparities in pediatric AML outcomes?
Yes, some kids face different challenges because of where they live, their race, or how much money their family has. There are efforts to make sure all kids get the best care.
What support resources are available for families facing childhood AML?
Families dealing with AML can find help. There are programs for money, emotional support, learning, and clinical trials. These resources help with the tough parts of diagnosis, treatment, and living after cancer.
What advances are being made in pediatric AML treatment?
New treatments for AML are being worked on. Doctors are looking at targeted therapies and immunotherapy. Clinical trials are testing these new ways to help kids live longer.
Reference
- National Cancer Institute: Childhood Acute Myeloid Leukemia Treatment (PDQ)
https://www.cancer.gov/types/leukemia/patient/child-aml-treatment-pdq