Last Updated on November 18, 2025 by Ugurkan Demir

Preparing for cervical neck fusion surgery can be a daunting task, but with expert guidance, you can navigate both the preparation and recovery phases with confidence.
At Liv Hospital, we understand the importance of proper preparation and rehabilitation to achieve optimal outcomes. Cervical fusion is a frequently performed procedure for patients with severe pain, degenerative disc disease, or spinal instability.
With a success rate exceeding 80 percent, cervical fusion surgery is a viable option for patients seeking relief from pain and improved function. We will guide you through the surgical techniques, recovery process, and potential complications to ensure a smooth and successful experience.
Key Takeaways
- Understand the importance of proper preparation for cervical neck fusion surgery
- Learn about the surgical techniques and recovery process
- Discover how to manage potential complications
- Find out what to expect during the rehabilitation phase
- Achieve optimal outcomes with expert guidance
Understanding Cervical Neck Fusion Surgery

Cervical neck fusion surgery, also known as cervical spine fusion, is a procedure that involves joining two or more bones in the neck. This surgical technique is used to stabilize the cervical spine, alleviate pain, and improve functionality. We will explore the details of this procedure, including its definition, reasons for undergoing it, and the expected outcomes.
What is Cervical Fusion?
Cervical fusion is a surgical procedure where two or more vertebrae in the cervical spine are fused together using bone grafts, rods, or other stabilizing devices. This fusion can help to:
- Reduce or eliminate pain caused by movement between vertebrae.
- Stabilize the spine and prevent further injury.
- Improve neurological function if nerves are being compressed.
The goal of cervical fusion is to create a stable and pain-free neck. By understanding the process and benefits, patients can make informed decisions about their treatment.
Common Reasons for Cervical Spine Fusion
Cervical spine fusion is typically recommended for patients with specific spinal conditions. Some of the common reasons include:
- Degenerative disc disease that causes significant pain or nerve damage.
- Spinal instability due to trauma or infection.
- Severe arthritis that affects the joints between vertebrae.
- Spondylolisthesis, where a vertebra slips out of place.
According to a study published in the Journal of Neurosurgery: Spine, “Cervical spine fusion is a highly effective treatment for various cervical spine disorders, offering significant pain relief and functional improvement.”
“Cervical spine fusion is a highly effective treatment for various cervical spine disorders, offering significant pain relief and functional improvement.”
Success Rates and Expected Outcomes
Recent studies have shown that the success rates for cervical fusions exceed 80 percent, with most patients experiencing significant pain relief and functional improvement. The expected outcomes can vary based on the individual condition and overall health of the patient.
| Outcome | Percentage |
|---|---|
| Pain Relief | 85% |
| Functional Improvement | 80% |
| Return to Normal Activities | 75% |
We understand that every patient’s journey is unique, and outcomes can depend on various factors, including the underlying condition and the patient’s overall health.
When Neck Infusion Surgery Becomes Necessary

Neck infusion surgery, also known as cervical fusion, becomes a necessary consideration for patients suffering from specific spinal conditions that significantly impair their quality of life. Understanding when this surgical intervention is required involves examining several critical spinal health issues. We will explore the conditions that make neck infusion surgery necessary, including degenerative disc disease, spinal instability, and severe neck pain, and discuss when conservative treatments are deemed ineffective.
Degenerative Disc Disease
Degenerative disc disease is a condition where the intervertebral discs in the neck deteriorate, leading to pain and reduced mobility. As the discs degenerate, they can no longer effectively cushion the vertebrae, resulting in discomfort and potentially leading to nerve compression. When conservative treatments fail to alleviate the symptoms, surgical options like neck infusion surgery may be considered.
Spinal Instability Conditions
Spinal instability occurs when the vertebrae are abnormally moved or are unable to maintain their normal position, often due to trauma, degenerative changes, or congenital conditions. This instability can cause significant pain and may lead to neurological symptoms if not addressed. Neck infusion surgery can help stabilize the spine, alleviate pain, and prevent further neurological deterioration.
Severe Neck Pain Indicators
Severe neck pain that is persistent and debilitating can be an indicator that surgical intervention is necessary. When neck pain is accompanied by other symptoms such as numbness, tingling, or weakness in the arms, it may signify nerve compression or damage. We evaluate these symptoms comprehensively to determine if neck infusion surgery is an appropriate treatment option.
When Conservative Treatments Fail
Conservative treatments, including physical therapy, medication, and lifestyle modifications, are typically the first line of treatment for neck pain and related conditions. However, when these treatments fail to provide adequate relief, surgical options are considered. The decision to proceed with neck infusion surgery is made after a thorough evaluation of the patient’s condition and a detailed discussion with the patient about the potential benefits and risks.
Types of Cervical Fusion Procedures
There are multiple approaches to cervical fusion surgery, each with its own benefits and risks. The choice of procedure depends on the patient’s specific condition, the location of the affected vertebrae, and the surgeon’s professional judgment.
Anterior Cervical Fusion Technique
Anterior cervical fusion involves accessing the spine through the front of the neck. This approach is commonly used for treating conditions affecting the discs and vertebrae in the neck. The benefits include less risk of nerve damage and generally less postoperative pain compared to posterior approaches.
During an anterior cervical fusion, the surgeon makes an incision in the neck, retracts the muscles and tissues, and removes the damaged disc or vertebra. A bone graft or implant is then inserted to stabilize the spine and facilitate fusion.
Posterior Cervical Fusion Approach
Posterior cervical fusion involves accessing the spine through the back of the neck. This method is often used for conditions that affect the posterior elements of the spine or when more extensive stabilization is required.
The posterior approach allows for greater access to the posterior spine, enabling surgeons to address complex issues such as spinal instability or deformity. However, it may involve more tissue disruption and potentially higher risks of nerve irritation.
Bone Grafts and Implant Options
Bone grafts are critical in cervical fusion surgery as they provide the biological material necessary for bone fusion to occur. There are several types of bone grafts, including autografts (from the patient), allografts (from a donor), and synthetic grafts.
Implant options, such as plates, rods, and cages, are used to stabilize the spine and support the bone graft during the fusion process. The choice of implant depends on the specific requirements of the patient’s anatomy and the surgeon’s preference.
| Procedure Type | Approach | Common Uses | Benefits |
|---|---|---|---|
| Anterior Cervical Fusion | Front of the neck | Disc herniation, vertebral fractures | Less risk of nerve damage, less postoperative pain |
| Posterior Cervical Fusion | Back of the neck | Spinal instability, deformity | Greater access to posterior spine, effective for complex issues |
Medical Preparation Before Surgery
Medical preparation is a critical phase before cervical neck fusion surgery, setting the stage for a successful outcome. We understand that this period can be both anticipatory and anxiety-provoking, so we aim to guide you through each necessary step.
Required Pre-operative Tests
Before your surgery, we require a series of tests to ensure you’re adequately prepared for the procedure. These tests may include:
- Blood work to check for any underlying conditions that could affect surgery or recovery
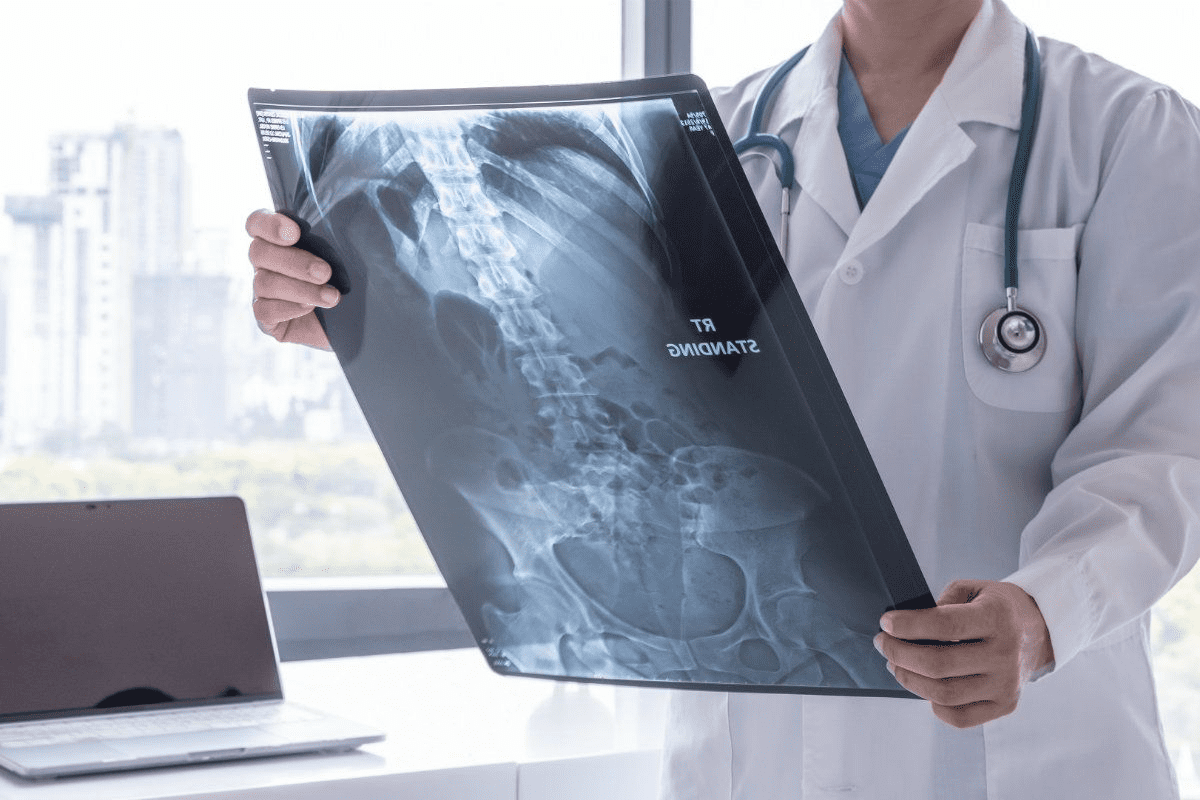
- Imaging studies such as X-rays, MRI, or CT scans to provide detailed views of your cervical spine
- Cardiac evaluations if you have a history of heart conditions
These tests help us assess your overall health and identify any potential risks.
Medication Adjustments and Restrictions
Certain medications can interfere with surgery or the healing process. We will review your current medications and supplements to determine if any need to be adjusted or stopped before surgery. This includes:
- Blood thinners that may need to be paused to reduce bleeding risks
- Anti-inflammatory medications that could affect bone healing
- Certain herbal supplements that may interact with anesthesia or other medications
It’s crucial to follow our guidance on medication adjustments to ensure your safety during and after surgery.
Nutritional Considerations
A well-balanced diet rich in essential nutrients can significantly impact your recovery. We recommend:
- Increasing your protein intake to support tissue repair
- Ensuring adequate calcium and vitamin D for bone health
- Staying hydrated to promote overall bodily functions
Nutritional optimization before surgery can enhance your body’s ability to heal and recover.
Final Consultation with Your Surgical Team
Before your surgery, we will have a final consultation to address any last-minute questions or concerns. This is an opportunity for you to:
- Review the surgical plan and what to expect
- Discuss post-operative care and recovery instructions
- Clarify any doubts about the procedure or recovery process
This consultation is a crucial step in preparing you mentally and physically for the surgery ahead.
Practical Preparation for Recovery
A successful recovery starts with practical preparation, including your home environment and support system. Ensuring that you have a comfortable and safe space to recover, along with the necessary support, can significantly impact your healing process.
Home Modifications for Post-Surgery Comfort
Modifying your home to facilitate a smooth recovery is essential. This includes:
- Creating a recovery zone on the ground floor to avoid stairs
- Ensuring that your home is free from tripping hazards
- Installing handrails in strategic locations
- Using a shower chair or bench for bathing safety
These modifications can help prevent accidents and make your recovery period more manageable.
Arranging Caregiver Support
Having a caregiver or support system in place is crucial for your recovery. This could be a family member, friend, or professional caregiver. They can assist with daily tasks, medication management, and providing emotional support.
It’s advisable to discuss your needs with your potential caregiver and create a schedule that works for both of you.
What to Pack for Your Hospital Stay
Packing the right items for your hospital stay can make your experience more comfortable. Essentials include:
| Item Category | Specific Items |
|---|---|
| Clothing | Comfortable clothes, slippers |
| Personal Care | Toothbrush, toothpaste, hairbrush |
| Medications | List of current medications, dosages |
| Entertainment | Books, tablet, or laptop |
Planning for Time Off Work
Planning for time off work is a critical aspect of your preparation. The amount of time you’ll need off depends on your job requirements and the nature of your surgery.
It’s recommended to discuss your recovery timeline with your surgeon and employer to ensure a smooth transition.
By focusing on these practical aspects of preparation, you can ensure a more comfortable and less stressful recovery period after your cervical neck fusion surgery.
The Day of Surgery: What to Expect
As you prepare for your cervical neck fusion surgery, understanding what to expect on the day of the operation can help alleviate anxiety. We want to ensure that you’re fully informed and comfortable throughout the process.
Pre-Operative Procedures
Before your surgery begins, you’ll undergo several pre-operative procedures. These typically include:
- Reviewing your medical history and current medications
- Changing into a surgical gown
- Receiving an intravenous (IV) line for administering medications and fluids
- Being positioned on the operating table to optimize surgical access
“The preparation is key to a successful surgery,” says a renowned spinal surgeon. “We take every precaution to ensure our patients are comfortable and ready for the procedure.”
Anesthesia Process
The anesthesia process is a critical component of your surgical experience. Our anesthesiologist will:
- Administer general anesthesia to ensure you’re asleep and pain-free during the surgery
- Monitor your vital signs throughout the procedure
- Adjust the anesthesia as needed to maintain your comfort and safety
It’s essential to follow the pre-operative instructions provided by your surgical team regarding eating, drinking, and medications to ensure the anesthesia works effectively.
The Surgical Procedure Step-by-Step
During the cervical neck fusion surgery, our surgical team will:
- Make an incision in the front or back of your neck, depending on the surgical approach
- Carefully move aside muscles and tissues to access the spine
- Remove any damaged discs or bone spurs
- Insert a bone graft or implant to stabilize the spine
- Close the incision with sutures or staples
The surgery typically takes a few hours, during which time our team will be with you every step of the way.
Immediate Post-Operative Recovery
After the surgery, you’ll be taken to the recovery room where our team will closely monitor your:
- Pain levels and manage any discomfort
- Vital signs, such as heart rate and blood pressure
- Neurological status, checking for any numbness or weakness
We’ll also provide you with instructions on how to care for yourself after discharge, including pain management, wound care, and follow-up appointments.
As you recover, it’s normal to feel a mix of relief and fatigue. Rest assured, our team is committed to supporting you through every stage of your recovery.
Hospital Recovery and Discharge
Understanding what to expect during hospital recovery can significantly ease the process after cervical fusion surgery. As you prepare for your hospital stay, it’s essential to know what to anticipate in terms of care and recovery.
Typical Hospital Stay Duration
The length of your hospital stay after cervical neck fusion surgery can vary depending on several factors, including the complexity of your procedure and your overall health. Typically, patients stay in the hospital for 1 to 3 days. During this time, our medical team closely monitors your condition, manages pain, and ensures that you’re recovering as expected.
Pain Management Protocols
Effective pain management is a critical aspect of your hospital recovery. We use a combination of medications and other techniques to minimize discomfort. Our pain management protocols are tailored to your individual needs, ensuring that you’re as comfortable as possible during your recovery.
Pain Management Strategies:
- Medications: We use a range of pain relief medications, from mild to stronger opioids, depending on your needs.
- Regional anesthesia: Techniques like nerve blocks can help manage pain in specific areas.
- Non-pharmacological methods: Techniques such as deep breathing, relaxation, and positional changes can also help manage discomfort.
Learning to Use a Cervical Collar
After cervical fusion surgery, wearing a cervical collar is often necessary to provide support and stability to your neck as it heals. Our healthcare team will guide you on how to properly use and care for your cervical collar.
| Aspect | Guideline |
|---|---|
| Wearing Schedule | Wear the collar as directed by your surgeon, typically at all times except when bathing or as otherwise instructed. |
| Adjustment | Ensure the collar is snug but not too tight. Adjust as necessary to maintain comfort and support. |
| Care | Clean the collar regularly with mild soap and water. Dry thoroughly to prevent skin irritation. |
Discharge Instructions and Restrictions
Before you’re discharged, our team will provide you with detailed instructions on how to continue your recovery at home. This includes information on medication, activity levels, and follow-up appointments.
Key Discharge Instructions:
- Follow your medication regimen as prescribed.
- Avoid heavy lifting, bending, or strenuous activities.
- Attend follow-up appointments as scheduled.
- Monitor for signs of complications, such as infection or neurological changes.
By understanding these aspects of hospital recovery and discharge, you’ll be better prepared for a successful recovery from cervical neck fusion surgery.
The Recovery Timeline After Cervical Fusion
Cervical fusion surgery marks the beginning of a significant recovery journey that typically spans several months. Understanding the different phases of recovery can help patients prepare for what to expect and how to optimize their healing process.
First Two Weeks: Initial Recovery Phase
The initial recovery phase is characterized by rest and gradual mobilization. During the first two weeks, patients are advised to avoid heavy lifting, bending, or strenuous activities. Pain management is crucial during this period, and patients are typically prescribed medication to manage discomfort.
As part of the recovery process, patients are encouraged to gradually increase their mobility with short walks and gentle stretches, as approved by their healthcare provider.
Weeks 2-6: Increasing Mobility
As patients progress into weeks 2-6, they can start to increase their mobility. This phase involves a gradual return to more normal activities, including light household chores and short drives. Physical therapy may be recommended to help improve range of motion and strengthen the neck muscles.
It’s essential during this phase to listen to your body and not push beyond what feels comfortable. Gradual progression is key to avoiding setbacks.
Months 2-3: Progressive Activity Reintroduction
By months 2-3, many patients can start reintroducing more strenuous activities into their routine. This may include more vigorous physical therapy exercises, heavier lifting (within specified limits), and a return to more demanding physical activities.
However, it’s crucial to follow the specific guidelines provided by the healthcare team to ensure that the fusion is healing correctly and to minimize the risk of complications.
Months 3-12: Complete Bone Fusion Process
The complete bone fusion process typically takes up to 12 months. During this time, regular follow-up appointments with the surgical team are vital to monitor the healing progress. Imaging tests such as X-rays or CT scans may be used to assess the fusion’s integrity.
Patients are advised to continue following the post-operative instructions and to report any unusual symptoms or concerns to their healthcare provider promptly.
As highlighted by a study published in the Journal of Neurosurgery: Spine, “The success of cervical fusion surgery is highly dependent on the patient’s adherence to the post-operative rehabilitation protocol.”
“Adherence to post-operative instructions and rehabilitation protocols significantly influences the outcome of cervical fusion surgery.”
| Recovery Phase | Timeline | Key Activities |
|---|---|---|
| Initial Recovery | First 2 weeks | Rest, pain management, gradual mobilization |
| Increasing Mobility | Weeks 2-6 | Light activities, physical therapy |
| Progressive Activity | Months 2-3 | More strenuous activities, vigorous physical therapy |
| Complete Bone Fusion | Months 3-12 | Regular follow-ups, imaging tests |
Physical Therapy and Rehabilitation Program
Physical therapy plays a vital role in helping patients regain strength and mobility after cervical fusion surgery. We understand that a comprehensive rehabilitation program is essential for achieving optimal outcomes and returning to daily activities with minimal discomfort.
Initiating Physical Therapy
Typically, physical therapy begins a few weeks after surgery, once the initial healing process has progressed. We recommend that patients start with gentle exercises to improve flexibility and gradually increase the intensity as guided by their physical therapist.
Key Therapeutic Exercises
The rehabilitation program includes a variety of exercises tailored to the patient’s specific needs. Some of the key therapeutic exercises focus on:
- Strengthening: Exercises to strengthen the muscles in the neck and upper back.
- Flexibility: Gentle stretches to improve range of motion.
- Posture Correction: Techniques to maintain proper posture and reduce strain on the cervical spine.
Gradually Returning to Daily Activities
As patients progress through their rehabilitation program, they can gradually return to their daily activities. We advise patients to:
- Start with low-impact activities such as walking or light housekeeping.
- Avoid heavy lifting, bending, or twisting.
- Monitor their body’s response and adjust activities accordingly.
Long-term Maintenance Exercises
To maintain the benefits of physical therapy and prevent future issues, we recommend continuing with a maintenance exercise program. This may include:
- Regular stretching to maintain flexibility.
- Strengthening exercises to support the cervical spine.
- Periodic check-ins with a physical therapist to adjust the program as needed.
By following a well-structured physical therapy and rehabilitation program, patients can achieve a successful recovery and enjoy improved quality of life after cervical neck fusion surgery.
Monitoring for Complications and Long-Term Care
Long-term care and vigilance for complications are essential components of the recovery process after cervical neck fusion surgery. As we navigate the post-operative period, it’s crucial to be aware of the potential issues that may arise and take proactive steps to mitigate them.
Warning Signs to Watch For
After cervical neck fusion surgery, patients must be vigilant for warning signs of complications. These may include:
- Increasing pain or discomfort
- Numbness, tingling, or weakness in the arms or legs
- Fever or chills
- Redness, swelling, or drainage from the surgical site
- Difficulty swallowing or breathing
If any of these symptoms occur, it’s essential to contact your healthcare provider immediately.
Preventing Adjacent Segment Disease
Adjacent segment disease (ASD) is a potential long-term complication of cervical neck fusion surgery. It occurs when the spinal segments adjacent to the fusion site become stressed, leading to degeneration. While some risk of ASD is inherent, certain lifestyle adjustments can help minimize this risk.
“The key to preventing adjacent segment disease lies in maintaining a healthy spine through proper posture, regular exercise, and avoiding excessive strain on the neck.” – Orthopedic Surgeon
Follow-up Appointments and Imaging
Regular follow-up appointments with your surgical team are critical for monitoring the healing process and detecting any potential complications early. These appointments may include imaging studies such as X-rays or MRIs to assess the fusion site and overall spinal health.
| Follow-up Timeline | Typical Activities |
|---|---|
| 2-4 weeks post-op | Initial follow-up, wound check |
| 6-12 weeks post-op | X-rays, assessment of fusion progress |
| 6-12 months post-op | Final assessment, long-term plan |
Lifestyle Adjustments for Spinal Health
Making certain lifestyle adjustments can significantly contribute to long-term spinal health after cervical neck fusion surgery. These may include:
- Maintaining a healthy weight
- Engaging in regular, low-impact exercise
- Practicing good posture
- Avoiding smoking and excessive alcohol consumption
By being proactive about your spinal health and following your healthcare provider’s guidance, you can maximize the success of your cervical neck fusion surgery and enjoy improved quality of life.
Conclusion: Life After Cervical Neck Fusion
After undergoing cervical neck fusion surgery, patients can expect a significant improvement in their quality of life. With proper care and rehabilitation, individuals can achieve substantial pain relief and improved function. The recovery process is crucial in determining the long-term outcomes of the surgery.
As we have discussed throughout this article, cervical neck fusion surgery is a complex procedure that requires careful preparation, precise execution, and thorough post-operative care. The long-term outcomes of this surgery are generally positive, with most patients experiencing a reduction in pain and an improvement in their overall spinal health.
Life after cervical neck fusion surgery involves continued care and maintenance to ensure optimal results. This includes following a rehabilitation program, attending follow-up appointments, and making lifestyle adjustments to promote spinal health. By doing so, patients can enjoy the benefits of their surgery for years to come.
FAQ
What is cervical neck fusion surgery?
Cervical neck fusion surgery, also known as cervical spine fusion, is a surgical procedure that involves fusing two or more vertebrae in the neck to stabilize the spine, relieve pain, and improve function.
What conditions can be treated with cervical fusion surgery?
Cervical fusion surgery can be used to treat various conditions, including degenerative disc disease, spinal instability, severe neck pain, and herniated discs.
What are the different types of cervical fusion procedures?
There are two main types of cervical fusion procedures: anterior cervical fusion and posterior cervical fusion. The choice of procedure depends on the location and severity of the condition being treated.
How long does it take to recover from cervical neck fusion surgery?
The recovery time for cervical neck fusion surgery varies, but most patients can expect to take several months to fully recover. The initial recovery phase typically lasts 2-6 weeks, followed by a gradual return to normal activities.
What are the benefits of physical therapy after cervical fusion surgery?
Physical therapy after cervical fusion surgery can help improve range of motion, strength, and flexibility, as well as reduce pain and stiffness. It can also help patients return to their normal activities and maintain long-term spinal health.
What are the potential complications of cervical neck fusion surgery?
Potential complications of cervical neck fusion surgery include infection, bleeding, nerve damage, and adjacent segment disease. It’s essential to follow post-operative instructions and attend follow-up appointments to minimize the risk of complications.
How can I prevent adjacent segment disease after cervical fusion surgery?
To prevent adjacent segment disease, it’s crucial to maintain a healthy lifestyle, including regular exercise, a balanced diet, and good posture. Regular follow-up appointments and imaging can also help detect any potential issues early.
What are the long-term outcomes of cervical neck fusion surgery?
The long-term outcomes of cervical neck fusion surgery are generally positive, with most patients experiencing significant pain relief and improved function. However, it’s essential to continue maintaining a healthy lifestyle and attending follow-up appointments to ensure optimal results.
How soon can I return to work after cervical fusion surgery?
The time it takes to return to work after cervical fusion surgery varies depending on the type of work and the individual’s recovery progress. Most patients can expect to take 4-12 weeks off work, but this can be longer or shorter depending on the specific circumstances.
What kind of pain management can I expect after cervical fusion surgery?
Pain management after cervical fusion surgery typically involves a combination of medication, rest, and physical therapy. Your surgical team will provide guidance on managing pain and discomfort during the recovery process.
Will I need to wear a cervical collar after surgery?
Yes, most patients will need to wear a cervical collar after cervical fusion surgery to provide support and stability to the neck. The duration of wearing the collar varies depending on the individual’s condition and the surgeon’s instructions.
What is cervical neck fusion surgery?
Cervical neck fusion surgery, also known as cervical spine fusion, is a surgical procedure that involves fusing two or more vertebrae in the neck to stabilize the spine, relieve pain, and improve function.
What conditions can be treated with cervical fusion surgery?
Cervical fusion surgery can be used to treat various conditions, including degenerative disc disease, spinal instability, severe neck pain, and herniated discs.
What are the different types of cervical fusion procedures?
There are two main types of cervical fusion procedures: anterior cervical fusion and posterior cervical fusion. The choice of procedure depends on the location and severity of the condition being treated.
How long does it take to recover from cervical neck fusion surgery?
The recovery time for cervical neck fusion surgery varies, but most patients can expect to take several months to fully recover. The initial recovery phase typically lasts 2-6 weeks, followed by a gradual return to normal activities.
What are the benefits of physical therapy after cervical fusion surgery?
Physical therapy after cervical fusion surgery can help improve range of motion, strength, and flexibility, as well as reduce pain and stiffness. It can also help patients return to their normal activities and maintain long-term spinal health.
What are the potential complications of cervical neck fusion surgery?
Potential complications of cervical neck fusion surgery include infection, bleeding, nerve damage, and adjacent segment disease. It’s essential to follow post-operative instructions and attend follow-up appointments to minimize the risk of complications.
How can I prevent adjacent segment disease after cervical fusion surgery?
To prevent adjacent segment disease, it’s crucial to maintain a healthy lifestyle, including regular exercise, a balanced diet, and good posture. Regular follow-up appointments and imaging can also help detect any potential issues early.
What are the long-term outcomes of cervical neck fusion surgery?
The long-term outcomes of cervical neck fusion surgery are generally positive, with most patients experiencing significant pain relief and improved function. However, it’s essential to continue maintaining a healthy lifestyle and attending follow-up appointments to ensure optimal results.
How soon can I return to work after cervical fusion surgery?
The time it takes to return to work after cervical fusion surgery varies depending on the type of work and the individual’s recovery progress. Most patients can expect to take 4-12 weeks off work, but this can be longer or shorter depending on the specific circumstances.
What kind of pain management can I expect after cervical fusion surgery?
Pain management after cervical fusion surgery typically involves a combination of medication, rest, and physical therapy. Your surgical team will provide guidance on managing pain and discomfort during the recovery process.
Will I need to wear a cervical collar after surgery?
Yes, most patients will need to wear a cervical collar after cervical fusion surgery to provide support and stability to the neck. The duration of wearing the collar varies depending on the individual’s condition and the surgeon’s instructions.