
If you’re dealing with neck pain, cervical fusion surgery might change your life. We get how complex and worrying this treatment can be. We’re here to help clear things up and offer support.
Cervical spine fusion is a surgery that makes the neck stable. It treats issues like degenerative disc disease and spinal instability. By joining two or more vertebrae, it can ease pain and improve function.
At our place, we focus on top-notch healthcare and support for patients from abroad. Our team is ready to help you at every step, from the first meeting to after the surgery.
Key Takeaways
- Cervical fusion surgery is used to treat various neck conditions.
- The procedure involves fusing two or more vertebrae to stabilize the neck.
- Our institution provides extensive support for international patients.
- We prioritize clear communication and personalized care.
- Our team is dedicated to guiding you through every step of the process.
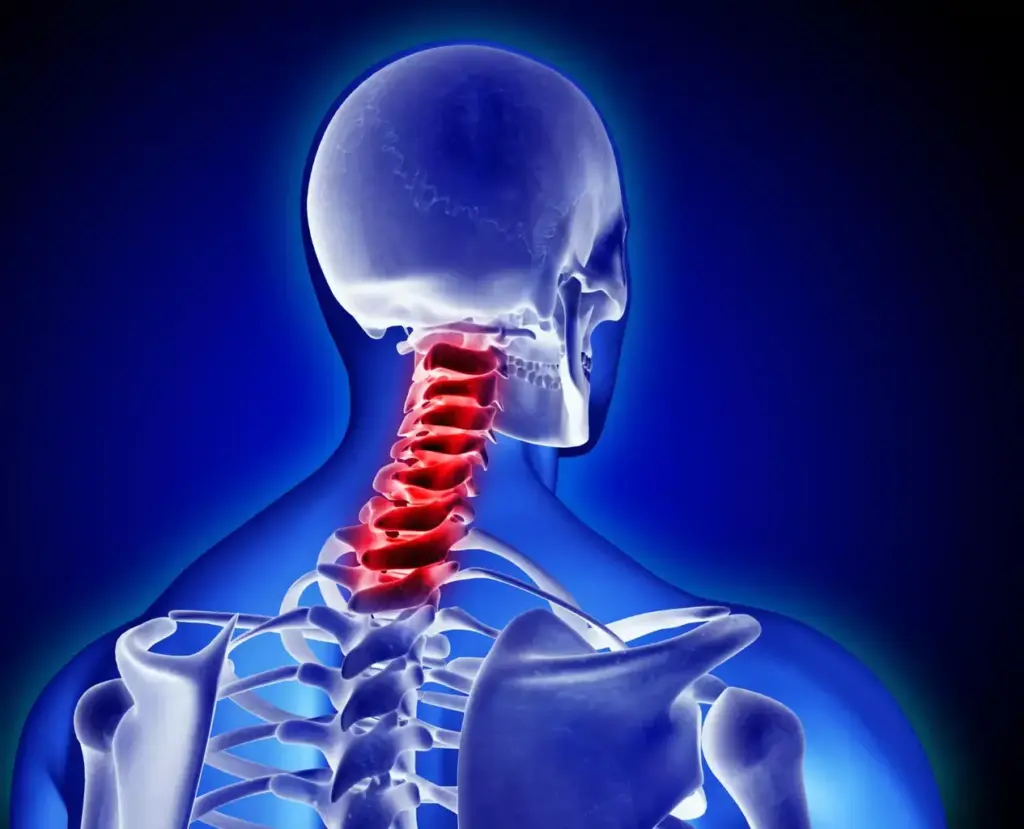
Understanding Cervical Spine Anatomy and Function

Knowing how the cervical spine works is key to fixing neck problems. The cervical spine is in the neck and helps hold the head up. It also lets us move our head in different ways.
The Structure of the Cervical Spine
The cervical spine has seven vertebrae, named C1 to C7. These vertebrae are linked by discs, ligaments, and muscles. They help keep the neck stable but also let it move.
The top two vertebrae, C1 and C2, have a special joint. This joint lets us rotate and nod our head.
Normal Function and Movement
The cervical spine is important for supporting the head and letting it move. It can bend forward and backward, rotate, and move side to side. The discs absorb shock, and the facet joints help the vertebrae move smoothly.
For the cervical spine to work right, everything must be in balance. If not, we might feel pain, stiffness, or have trouble moving.
Common Issues Affecting the Cervical Spine
Many problems can happen to the cervical spine, including:
- Degenerative Disc Disease: This is when the discs wear out, causing pain and stiffness.
- Cervical Spondylosis: It’s when the vertebrae and discs wear down with age.
- Herniated Discs: When the discs bulge or tear, they can press on nerves.
- Spinal Stenosis: This is when the spinal canal gets too narrow, putting pressure on the spinal cord.
- Traumatic Injuries: These can be from accidents or falls, causing fractures, dislocations, or sprains.
These issues can be very uncomfortable and might need a doctor’s help. Knowing about the cervical spine’s anatomy and function is important for finding and treating these problems.
What is Spinal Fusion Cervical Spine Surgery?
Spinal fusion cervical spine surgery is a surgery that joins vertebrae in the neck. It treats many neck problems by making the vertebrae stable. This helps to reduce symptoms of spinal disorders.
Definition and Basic Concept
Spinal fusion cervical spine surgery, or cervical fusion surgery, is a special operation. It aims to make the neck stable again. Bone grafts or synthetic materials are used to join the vertebrae, stopping painful motion and helping them heal.
The surgery can be done in different ways. For example, anterior cervical fusion is done from the front of the neck. Or, posterior cervical fusion is done from the back.
Historical Development of the Procedure
Cervical fusion surgery has changed a lot over time. The first attempts were in the early 20th century. But, it wasn’t until the 1950s and 1960s that modern methods started to develop.
The introduction of anterior cervical discectomy and fusion (ACDF) was a big step forward. It made it easier to fix cervical spine problems.
Now, thanks to new technologies and techniques, the surgery is even better. This has improved how well the surgery works.
Modern Approaches to Cervical Fusion
Today’s spinal fusion cervical spine surgery uses advanced technologies and methods. Surgeons use tools like intraoperative CT scans for better accuracy and to see the anatomy clearly.
Also, minimally invasive surgical techniques have made recovery faster and caused less damage. Using biologics and synthetic materials has also improved the fusion process. These options are better than traditional bone grafting.
7 Key Facts About Cervical Fusion Surgery
Learning about cervical fusion surgery can help patients make better choices. This surgery stabilizes the cervical spine. It’s important for patients to know several key things about it.
Fact 1: Most Common Age Group (55-74 Years)
Most people getting cervical fusion surgery are between 55 and 74 years old. This age group often deals with degenerative disc disease. Studies show that about 60% of cervical fusion surgeries are for people in this age range.
Fact 2: ACDF is the Most Common Technique
Anterior Cervical Discectomy and Fusion (ACDF) is the top cervical fusion method. It removes a bad disc and fuses the next vertebrae together. ACDF is favored because it works well and has fewer complications.
Fact 3: Market Value and Growth Projections
The global cervical fusion market is growing fast. This is because more people are getting older and getting spine problems. The market is expected to hit $2.5 by 2025, with a 4.5% annual growth. This growth is thanks to better surgery methods and materials.
Fact 4: Materials Used in Fusion
Different materials are used in cervical fusion, like autografts, allografts, and synthetic ones. The right material depends on the patient’s needs and the surgeon’s choice. New materials are being made that work better and are safer for the body.
Common Conditions Requiring Cervical Fusion
Many conditions need cervical fusion to ease pain and improve stability. This surgery is a top choice for treating cervical spine issues. Let’s look at the main reasons people need this surgery.
Degenerative Disc Disease
Degenerative disc disease happens when cervical spine discs wear out. This causes pain and makes it hard to move. The discs lose their cushioning, leading to stiffness and discomfort.
Symptoms of degenerative disc disease include:
- Neck pain
- Radiating pain to the arms
- Numbness or tingling sensations
- Weakness in the arms or hands
If other treatments don’t work, cervical fusion might be suggested. It helps stabilize the area and reduce pain.
Cervical Instability
Cervical instability means too much movement between vertebrae. This can harm nerves or press on the spinal cord. It might come from injury, wear and tear, or other issues.
Signs of cervical instability may include:
- Excessive neck motion
- Pain during movement
- Neck stiffness
- Neurological symptoms like numbness or weakness
Cervical fusion is used to keep the spine stable. It helps prevent further damage or worsening of symptoms.
Traumatic Injuries
Severe injuries to the cervical spine, like fractures or dislocations, might need cervical fusion. This surgery helps restore stability and prevent long-term damage.
Common traumatic injuries include:
- Fractures of the cervical vertebrae
- Dislocations or subluxations
- Spinal cord injuries
Cervical fusion helps align and stabilize the spine. It aids in recovery and lowers the chance of complications.
Other Indications for Surgery
Other reasons for cervical fusion include:
- Spondylolisthesis
- Spinal deformities
- Infections or tumors affecting the cervical spine
- Revision surgery for previous fusion failures
Each condition presents its own challenges. Cervical fusion is customized to meet the specific needs of each patient.
In summary, cervical fusion is a key surgical option for many cervical spine problems. Understanding these conditions helps patients see why this surgery is often necessary and its benefits.
Types of Cervical Fusion Procedures
Surgeons have many options for cervical spine fusion. Each procedure has its own benefits and is chosen based on the patient’s needs. The decision depends on the patient’s condition, anatomy, and the surgeon’s experience.
Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is a common cervical fusion procedure. It’s done through the front of the neck. The damaged disc is removed, and a bone graft or synthetic material is used to help the spine fuse.
ACDF is often chosen for issues in the front part of the cervical spine. It gives direct access to the disc space. It’s used for degenerative disc disease and herniated discs.
Posterior Cervical Fusion
Posterior cervical fusion is done through the back of the neck. It’s used for conditions affecting the back of the spine or when back stabilization is needed.
This procedure can be used alone or with other treatments. It’s great for stabilizing the back of the spine.
Lateral Approaches
Lateral approaches access the spine from the side. These methods are less common but useful in some cases.
They require special training and tools. They can be safer in certain situations than other approaches.
Choosing the Right Approach
Choosing the right cervical fusion procedure is complex. It depends on the patient’s anatomy, the location and type of spinal problem, and the surgeon’s skills.
A detailed evaluation and diagnosis are key to picking the best surgery. Surgeons look at imaging and the patient’s symptoms to decide.
Surgical Techniques and Materials Used
Surgical techniques and materials are key to cervical fusion surgery’s success. The right choice can greatly affect the outcome and recovery.
Bone Grafts: Autografts vs. Allografts
Bone grafts are essential for fusing vertebrae in cervical fusion surgery. There are two main types: autografts and allografts.
Autografts come from the patient’s own body, often the iliac crest. They have advantages like lower rejection risk and living cells for fusion. But, they need another surgery site, which can increase recovery time.
Allografts, from donors, are processed and sterilized to reduce disease risk. They avoid the need for a second surgery, but might have a lower fusion rate than autografts.
| Characteristics | Autografts | Allografts |
|---|---|---|
| Source | Patient’s own body | Donor |
| Risk of Rejection | Lower | Higher |
| Additional Surgery | Yes | No |
| Fusion Rate | Higher | Lower |
Hardware: Plates, Screws, and Cages
Hardware like plates, screws, and cages also plays a role. They stabilize the spine and aid in fusion. These devices ensure the spine stays aligned during healing.
In ACDF procedures, plates and screws secure vertebrae. Cages hold the bone graft and keep disc space, aiding fusion.
Synthetic Materials and Biologics
Synthetic materials and biologics enhance cervical fusion surgery. Materials like titanium and PEEK are used in implants. Biologics, like BMPs, stimulate bone growth for fusion.
These advancements offer more treatment options. But, the right material or biologic depends on the patient’s needs and condition.
Minimally Invasive Cervical Fusion Techniques
Minimally invasive cervical fusion techniques have changed spinal surgery a lot. They cause less damage to tissues, less pain after surgery, and shorter hospital stays. It’s important to look at their benefits, possible problems, and who should get them.
Advantages of Minimally Invasive Approaches
These techniques have many benefits. Less tissue damage means less pain and faster recovery. They also leave smaller scars, which many patients like. Plus, they often have lower infection rates than traditional surgery.
Reduced Complications and Hospital Stays
Minimally invasive cervical fusion also means fewer problems and shorter hospital stays. Patients have fewer issues like infections and nerve damage. Shorter stays also save money and reduce infection risks.
| Benefits | Traditional Open Surgery | Minimally Invasive Surgery |
|---|---|---|
| Tissue Damage | Significant | Minimal |
| Postoperative Pain | Higher | Lower |
| Hospital Stay | Longer | Shorter |
| Infection Rate | Higher | Lower |
Patient Selection Criteria
Not every patient is right for minimally invasive cervical fusion. We check things like how bad the condition is, the patient’s health, and past surgeries. Patients with complex spinal anatomy or severe degenerative disc disease might not be good candidates. We need to carefully decide the best option for each patient.
Preparing for Cervical Fusion Surgery
Getting ready for cervical fusion surgery is a big step. It involves medical checks and getting your life in order. We’re here to help you feel ready and confident.
Medical Evaluation and Testing
First, you’ll need a detailed medical check. This includes tests and assessments to see if you’re a good fit for the surgery. These might include blood tests, MRI or CT scans, and a physical check-up. Your medical team will look at your health history, talk about your meds, and explain the surgery’s risks and benefits.
Tell your doctor about your health history, past surgeries, allergies, and chronic conditions. This helps make the surgery plan just right for you and lowers the risk of problems.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before surgery can help your recovery. Quitting smoking is key because it helps your body heal faster and lowers risks. Eating well is also important for your body’s recovery.
Make your home safe and comfy for when you’re recovering. This might mean setting up a recovery area and getting help with daily tasks.
What to Expect on Surgery Day
On surgery day, you’ll get clear instructions on what to eat, drink, and take. It’s important to follow these to stay safe during the surgery. Arrive at the hospital or surgical center early to get settled before your surgery.
During surgery, a skilled team will watch over you. They’ll keep an eye on your health and make sure you’re comfortable. After, you’ll go to a recovery area where you’ll be watched closely as you wake up from the anesthesia.
Knowing what to expect can help you feel less anxious and more in control. Our team is here to support you from start to finish.
Recovery Timeline After Cervical Spine Fusion
Knowing what to expect after cervical spine fusion surgery is key. It helps patients manage their recovery smoothly. The time it takes to heal can vary based on several factors, like the patient’s health and the surgery’s complexity.
Immediate Post-Operative Period
The first few days to a week after surgery are critical. Patients are watched closely for any issues, and managing pain is a top priority. Effective pain management is key for comfort and early movement.
Resting and avoiding hard activities are advised. Patients might feel pain, swelling, or bruising in their neck. These symptoms can be managed with medication and rest. Having a support system during this time is also important.
Short-Term Recovery (First 6 Weeks)
In the first six weeks, patients start to get back to normal. A structured rehabilitation program helps regain neck strength and flexibility. Physical therapy might be suggested to aid in this process.
Heavy lifting, bending, or twisting should be avoided. Sleeping arrangements might need to be changed to keep the neck aligned properly. Following these guidelines helps prevent complications.
Long-Term Recovery and Rehabilitation
Recovery can take months beyond the first six weeks. Patients keep working on strengthening the muscles around the cervical spine. Sticking to the rehabilitation program is essential for the best results.
Regular check-ups with the healthcare provider are important to track the fusion’s progress and address any issues. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, supports recovery.
Return to Normal Activities
When patients can go back to their usual activities varies. Most people can get back to their daily lives in a few weeks to months. But, high-impact activities or heavy lifting should be avoided for longer.
It’s wise to talk to the healthcare provider before starting any strenuous activities. This ensures the recovery and fusion success are not compromised.
Potential Risks and Complications
It’s important to know the risks and complications of cervical fusion surgery. This surgery is usually safe and works well. But, there are some risks.
Common Side Effects
Patients might feel some common side effects after surgery. These can include:
- Neck pain or stiffness
- Swallowing difficulties
- Numbness or tingling in the arms or hands
- Fatigue
These side effects are usually short-term and go away in a few weeks.
Serious Complications
Though rare, serious complications can happen. These might include:
- Infection
- Nerve damage
- Bone graft complications
- Hardware failure
Talking to your surgeon about these risks is key. This helps you understand the surgery’s benefits and risks.
Adjacent Segment Disease
Adjacent segment disease (ASD) is a long-term risk. It happens when the spinal segments next to the fusion site wear out over time. Studies show ASD can affect up to 25% of patients within 10 years after surgery.
“The risk of adjacent segment disease is a significant consideration in the long-term management of patients who have undergone cervical fusion surgery.” –
Risk Factors for Complications
Some factors can raise the risk of complications. These include:
| Risk Factor | Description |
|---|---|
| Age | Older patients may have a higher risk of complications |
| Smoking | Smoking can impair bone healing and increase the risk of complications |
| Pre-existing conditions | Conditions like diabetes or osteoporosis can affect recovery |
Knowing these risk factors helps patients take steps to lower their risk of complications.
Benefits and Success Rates of Cervical Fusion
Cervical fusion surgery offers many benefits. It helps patients feel less pain and move better. This surgery can greatly improve a person’s life quality.
Pain Relief Outcomes
Cervical fusion surgery is very good at reducing pain. Most patients see a big drop in their pain levels after surgery. Effective pain management is key to getting back to normal.
The surgery stabilizes the spine and removes the source of pain. Our patients say they can do more things easily again.
Functional Improvement Statistics
Another big plus of cervical fusion surgery is better mobility. Patients can move more freely and easily after the surgery. We’ve gathered data to show how well this works.
| Functional Improvement Metrics | Pre-Surgery | Post-Surgery (6 months) |
|---|---|---|
| Neck Disability Index (NDI) | 40% | 15% |
| Range of Motion (ROM) | 30° | 50° |
| Muscle Strength | 60% | 85% |
Quality of Life Changes
Cervical fusion surgery can make a big difference in a person’s life. It helps them do things they love again. Enhanced quality of life is a main benefit of this surgery.
Patient Satisfaction Metrics
Patient happiness is a key sign of success with cervical fusion surgery. We see very high satisfaction rates. Patients are happy with the pain relief and how they can move better.
More than 85% of patients are glad they had the surgery. They say it greatly improved their symptoms and overall health.
Conclusion: The Future of Cervical Spine Fusion
The field of cervical spine fusion is changing fast, thanks to new research and ideas. We’re looking forward to big improvements in how we treat this condition. These changes will make patients’ lives better and their recovery times shorter.
New trends include less invasive surgeries and new materials for implants. Technology like robotics and navigation systems will also play a big role. These tools will help doctors do complex surgeries more accurately and safely.
We expect to see better fusion rates and faster recoveries in the future. Biologics and synthetic materials will help bones heal faster and stronger. This will lead to more successful surgeries.
We’re excited for the future of cervical spine fusion. We’re committed to giving our patients the newest treatments and technologies. This way, they get the best care for their spine problems.

































