When you think about cervical spine fusion, knowing the details is key. At Liv Hospital, we offer top-notch healthcare. We also support international patients fully.
Cervical spine fusion is a surgery that connects two or more neck vertebrae. Studies show that single- or two-level cervical fusion surgeries work about 90 percent of the time.
Let’s dive into the important facts about cervical spine fusion surgery. We’ll talk about what happens during recovery. We focus on both medical skill and caring for the patient.
Key Takeaways
- Understanding the purpose and benefits of cervical spine fusion
- Success rates of traditional single- or two-level cervical fusion surgeries
- The importance of patient-centered care in spinal fusion cervical spine procedures
- What to expect during the recovery process
- The role of medical expertise in ensuring a successful surgery
What Cervical Spine Fusion Surgery Entails

Cervical spine fusion surgery is a way to treat chronic neck pain and instability. We’ll explain what it involves, its purpose, and the conditions it treats.
Definition and Purpose of the Procedure
Cervical spine fusion, or cervical neck fusion, fuses two or more vertebrae in the neck. It aims to ease pain, stabilize the spine, and improve function. This is done by stopping the motion between vertebrae that causes pain or nerve problems.
The surgery uses bone grafts or artificial materials to join the vertebrae. This creates a single, stable unit. It helps with conditions like degenerative disc disease, spinal instability, or cervical spine trauma.
Common Conditions Requiring Cervical Fusion
Cervical spine fusion is often needed for certain neck conditions. These include:
- Degenerative disc disease
- Herniated discs
- Spinal stenosis
- Spondylolisthesis
- Trauma or fractures
- Instability or excessive motion between vertebrae
These issues can cause chronic pain, nerve damage, or spinal instability. They can greatly affect a person’s quality of life.
Goals and Expected Outcomes
The main goals of cervical spine fusion surgery are to relieve pain, stabilize the spine, and improve nerve function. Achieving these goals can greatly improve a patient’s life quality.
| Condition | Goal of Surgery | Expected Outcome |
|---|---|---|
| Degenerative Disc Disease | Relieve pain and stabilize spine | Reduced pain, improved mobility |
| Spinal Stenosis | Decompress nerves and stabilize spine | Improved neurological function, reduced pain |
| Trauma or Fractures | Stabilize spine and promote healing | Improved spinal stability, reduced risk of further injury |
Understanding cervical spine fusion surgery helps patients make informed choices. They can know what to expect from the procedure.
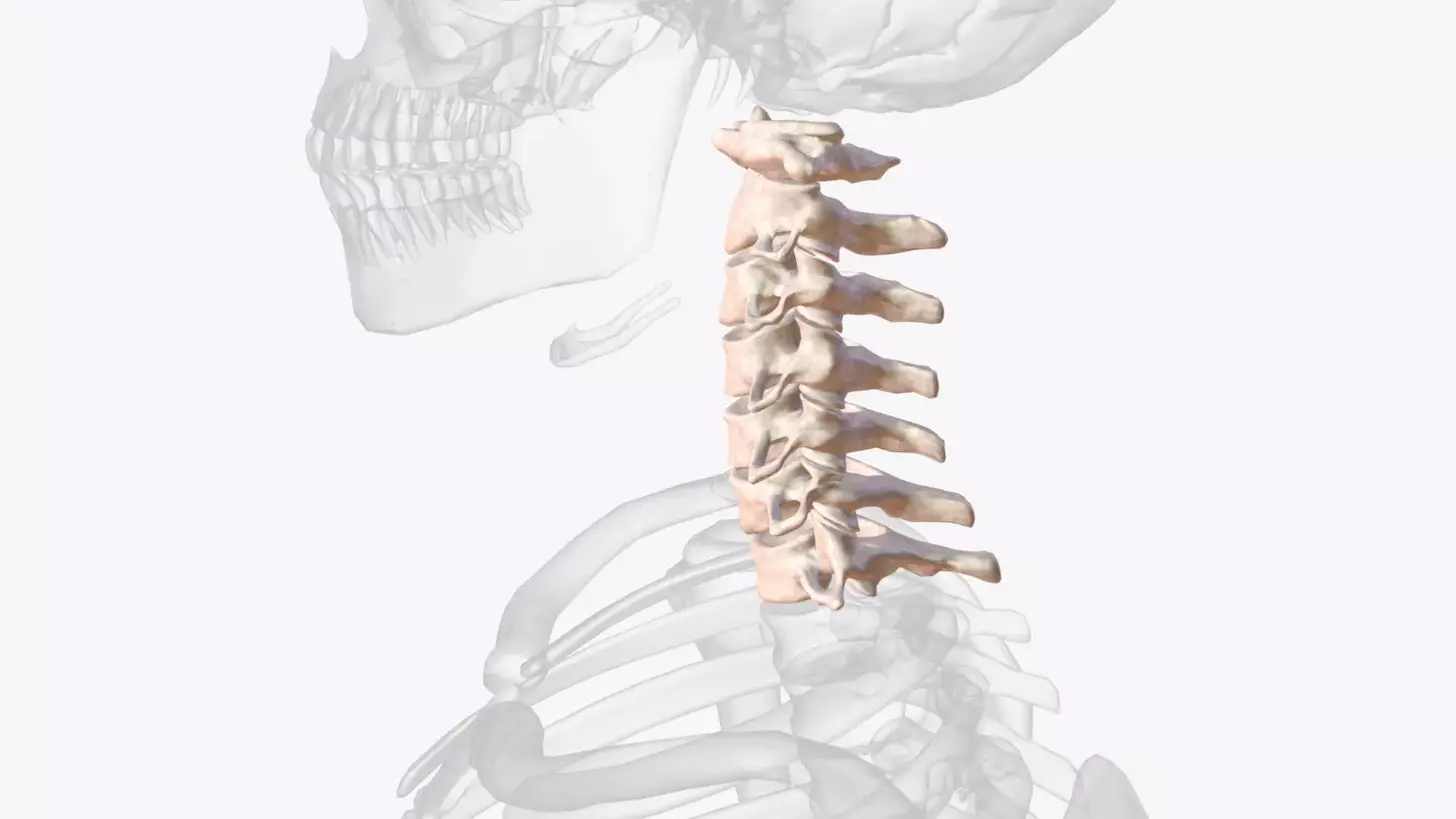
The Anatomy and Mechanics of Cervical Spine Fusion

It’s key to know the cervical spine’s anatomy to understand fusion mechanics. The cervical spine, with seven vertebrae, supports the head and allows for movement.
Understanding Cervical Spine Structure
The cervical spine has seven vertebrae (C1-C7). They support the head, offer flexibility, and protect the spinal cord. Intervertebral discs, between vertebrae, absorb shock and help with smooth movement.
The first two vertebrae (atlas and axis) allow head rotation. The rest of the vertebrae support and flex. The lower part (C5-C7) handles most mechanical stress.
How Fusion Creates Stability
Cervical spine fusion is a surgery that joins vertebrae for stability and pain relief. It stops vertebrae motion, which can cause pain.
The fusion uses bone grafts to join vertebrae. As the graft heals, it forms a strong bond, stabilizing the spine long-term.
There are different fusion techniques, like anterior and posterior approaches, each suited for specific needs.
Bone Graft Materials and Fusion Process
Bone grafts are vital for fusion. They can be from the patient (autograft), donated (allograft), or synthetic. The choice depends on the patient’s health, fusion extent, and surgeon’s choice.
The fusion stages start with placing bone graft between vertebrae. As it heals, a solid bond forms. This healing can take months, with the patient needing a brace or physical therapy.
A successful fusion can greatly improve a patient’s life by reducing pain and boosting mobility.
Types of Cervical Spine Fusion Procedures
The type of cervical spine fusion procedure depends on the patient’s condition and anatomy. This surgery is flexible and can treat many spinal problems. We’ll look at the different methods used in cervical spine fusion surgery.
Anterior Cervical Fusion Approaches
Anterior cervical fusion is done through the front of the neck. It’s often used for herniated discs, spinal stenosis, and fractures. Anterior cervical discectomy and fusion (ACDF) is a common procedure, where the damaged disc is removed and the vertebrae are fused.
This approach gives direct access to the front of the spine. It’s chosen for its benefits, like less risk of nerve damage.
Posterior Cervical Fusion Techniques
Posterior cervical fusion is done through the back of the neck. It’s used for conditions like facet joint arthritis or posterior ligament instability. Posterior cervical fusion uses rods, screws, and bone grafts.
This approach offers great exposure to the back of the spine. It’s best for complex spinal problems needing posterior stabilization.
C Spine Fusion Surgery Methods
C spine fusion surgery includes both anterior and posterior methods. The choice depends on the patient’s condition, the location of the problem, and the surgeon’s preference. Cervical spine fusion can be done with open surgery or minimally invasive techniques, each with its own benefits.
Disc Fusion Cervical Spine Interventions
Disc fusion cervical spine interventions target disc problems. Procedures like ACDF remove the damaged disc and fuse the vertebrae. Other methods, like cervical disc arthroplasty, replace the disc with an artificial one. These aim to stabilize the spine and relieve symptoms.
Knowing about the different cervical spine fusion procedures is key for patients and healthcare providers. By considering the patient’s anatomy, condition, and health, surgeons can pick the best technique for the best results.
Key Fact #1: Success Rates of Modern Cervical Fusion Surgery
Modern cervical fusion surgery has made big strides, leading to better success rates. Thanks to new surgical methods and better patient choices, outcomes have greatly improved.
Traditional Single and Two-Level Fusion Outcomes
Traditional single and two-level cervical fusion surgeries have a high success rate, around 90%. Most patients see a big relief from their symptoms and achieve successful fusion.
Multi-Level Fusion Success Rates
For complex cases needing multi-level fusions, success rates are encouraging at 61% or higher. These cases are more challenging due to the extensive surgery needed. Yet, modern techniques have made outcomes better even in these tough situations.
Reduction in Revision Surgery Needs
Modern cervical fusion surgery has also seen a drop in the need for revision surgeries. Thanks to better techniques and materials, complications needing more surgery have decreased. This not only helps patients but also eases the healthcare system’s load.
We keep seeing progress in cervical spine fusion, with ongoing research aiming to boost success rates and patient outcomes. Advances in imaging, better bone grafts, and advanced surgical tools have played a big role in these improvements.
Knowing the success rates of cervical fusion surgery helps patients make better choices. It’s key for patients to talk with their healthcare provider about their situation and what to expect. This way, they can understand their treatment options clearly.
Key Fact #2: Patient Selection and Factors Affecting Cervical Spine Fusion Outcomes
Knowing what affects cervical spine fusion outcomes is key. Choosing the right patient is vital for success.
Age Considerations
Age is a big factor in cervical spine fusion success. Older patients might see paradoxical benefits. This is because their bodies naturally fuse vertebrae and gain stability. This can lead to better fusion results for them.
Impact of Obesity on Surgical Success
Obesity can greatly affect cervical spine fusion surgery success. Studies show it may raise the risk of problems and impact the surgery’s outcome. Yet, with the right planning and care, obese patients can have successful fusions.
Disease Duration and Severity
The length and severity of the condition needing fusion also matter. Patients with longer or more severe conditions face unique recovery challenges. Knowing this helps set realistic hopes for the surgery.
Natural Autofusion and Vertebral Stability
Natural autofusion is the body’s way of fusing vertebrae. It can add to spine stability, improving fusion surgery outcomes. This is more common in older patients, helping them achieve more stable fusions.
Healthcare providers can improve patient selection for cervical spine fusion by considering these factors. It’s a detailed process that looks at how different patient traits and the surgery interact.
Key Fact #3: Pre-Surgical Preparation for Optimal Results
Pre-surgical preparation is key for a successful cervical spine fusion. It prepares you for surgery and recovery. We stress the need for thorough preparation for the best results.
Required Medical Evaluations and Testing
Before surgery, patients must go through detailed medical checks. These tests find any health risks and check if you’re right for the surgery. Tests include blood work, imaging like X-rays and MRI, and heart checks. Our team will use these results to plan your surgery.
Lifestyle Adjustments Before Surgery
Changing your lifestyle before surgery can greatly help. Quitting smoking is important because it helps healing and success. Also, staying healthy, managing chronic conditions, and avoiding certain meds are key. Our team will guide you on what changes to make.
Mental Preparation and Setting Realistic Expectations
Mental readiness is as important as physical. We urge patients to understand their surgery and recovery well. Having a support system and knowing what to expect can lower stress. Talking to our team about your concerns can make you feel more ready.
Key Fact #4: The Surgical Experience and Hospital Stay
As patients prepare for cervical spine fusion, knowing what to expect can ease anxiety. We know this knowledge is key for patients to feel in control of their treatment.
What to Expect During Surgery
During cervical spine fusion surgery, our skilled surgeons use the latest technology for precision and safety. They make an incision in the neck, remove the damaged disc, and fuse the vertebrae with bone graft material.
Advanced surgical techniques and careful planning help us minimize risks and improve outcomes. Patients are watched closely during the surgery to ensure their safety and comfort.
Anesthesia Considerations
Anesthesia is vital in cervical spine fusion surgery. Our anesthesiologists work with the surgical team to choose the right anesthesia. This keeps patients comfortable and pain-free during the surgery.
The type of anesthesia depends on the patient’s needs and the surgery specifics. We talk about these details with patients before surgery to address any concerns.
Typical Hospital Stay Duration
The hospital stay after cervical spine fusion surgery usually lasts 1 to 2 days. This lets our medical team closely watch the patient’s recovery and manage any pain.
Immediate Post-Operative Care
Immediate care after surgery is key for a smooth recovery. Our healthcare team provides detailed care, including pain management, wound care, and watching for complications.
Patients also get advice on posture, lifting, and activity levels for at-home care. We encourage patients to contact us with any questions or concerns during their recovery.
Key Fact #5: Recovery Timeline After Cervical Neck Fusion
The journey to recovery after cervical spine fusion surgery has many stages. Each stage has its own challenges and milestones. It’s important for patients to know these stages to manage their expectations and get the best results.
Short-Term Recovery Milestones (0-6 Weeks)
In the first weeks after surgery, patients often feel pain, numbness, and have limited mobility. We watch these symptoms closely and help with pain management and post-operative care.
It’s key to follow a structured rehabilitation program during this time. This helps ensure proper healing and avoids complications.
Medium-Term Healing Process (6 Weeks-6 Months)
As patients move into the medium-term recovery phase, they start to see big improvements. We suggest continuing with physical therapy to boost strength, flexibility, and range of motion.
Long-Term Fusion Completion (6 Months-1 Year+)
The long-term recovery phase is marked by continued bone fusion and strengthening of the cervical spine. We advise patients to keep a healthy lifestyle, including regular exercise and a balanced diet, to support the fusion process.
Physical Therapy and Rehabilitation Protocols
Physical therapy is vital in the recovery process. It helps patients regain strength, improve flexibility, and achieve the best outcomes. Our rehabilitation protocols are customized to meet each patient’s specific needs and goals.
| Recovery Stage | Timeline | Key Milestones |
|---|---|---|
| Short-Term | 0-6 Weeks | Pain management, initial healing |
| Medium-Term | 6 Weeks-6 Months | Improved mobility, strength gain |
| Long-Term | 6 Months-1 Year+ | Bone fusion, full recovery |
Key Fact #6: Understanding Complications and Risk Management
Knowing the risks of cervical spine fusion is key to a smooth recovery. This procedure is effective for many neck issues. Yet, it carries some risks.
Common Complications of Cervical Fusion
Cervical spine fusion surgery can have complications. Some common ones include:
- Infection at the surgical site
- Nerve damage or irritation
- Bone graft complications
- Hardware failure (e.g., loosening or breakage of implanted devices)
- Adjacent segment disease (degeneration of nearby spinal segments)
These issues can affect recovery differently. It’s vital for patients to know these risks to make informed choices.
Risk Factors for Complications
Some factors can raise the risk of complications. These include:
- Age: Older patients face higher risks due to bone density and health.
- Smoking: It hinders bone healing and increases risks.
- Obesity: Excess weight stresses the spine and implants.
- Pre-existing medical conditions: Conditions like diabetes or osteoporosis can affect healing and increase complication risks.
Knowing these risk factors helps us take steps to reduce them.
Strategies to Minimize Risks
We use several strategies to lower risks:
- Careful patient selection and pre-operative evaluation
- Advanced surgical techniques and technology
- Post-operative care protocols, including pain management and physical therapy
- Lifestyle modifications, such as smoking cessation and weight management
These strategies help reduce complications and improve outcomes.
When to Contact Your Surgeon Post-Operation
After surgery, watch your recovery closely. Seek help if you notice unusual symptoms. Contact your surgeon if you see:
- Increasing pain or swelling
- Signs of infection (fever, redness, drainage)
- Numbness, tingling, or weakness in the arms or legs
- Difficulty swallowing or breathing
Quick communication with your healthcare team is essential for early issue resolution and the best outcome.
Key Fact #7: Life After Cervical Spine Fusion
Life after cervical spine fusion requires big changes for the best results. We must understand the lifestyle changes, activity limits, and follow-up care needed for recovery.
Long-Term Lifestyle Adjustments
After surgery, patients must make big lifestyle changes. Maintaining a healthy weight is key to avoid putting extra strain on the spine. Eating a diet rich in calcium and vitamin D is also important for bone health.
It’s important to exercise, but it must fit the person’s needs and abilities. Gentle exercises like yoga or swimming help keep flexibility and strength without harming the spine.
Activity Restrictions and Modifications
Some activities may need to be avoided or changed after surgery. We advise against high-impact activities such as contact sports or heavy lifting to protect the fusion and avoid injury.
Small changes, like adjusting sleeping positions or using supportive devices, can help a lot. Using a supportive pillow at night can also keep the neck in the right position.
Adjacent Segment Disease Prevention
Adjacent segment disease is a risk after cervical spine fusion. To lower this risk, regular check-ups and watching for signs of the disease are key.
Keeping the spine healthy through good posture, exercise, and a balanced diet can also prevent this disease. Regular check-ups with your doctor are important for spinal health.
Follow-Up Care Schedule
A set follow-up care schedule is important for tracking healing and solving any problems quickly. Follow-up visits are usually at 6 weeks, 3 months, 6 months, and 1 year after surgery.
At these visits, your doctor will check the fusion site, watch for complications, and guide you on recovery and rehabilitation. Following the recommended schedule is key for the best results.
“The key to a successful recovery after cervical spine fusion lies in the patient’s ability to adhere to the recommended lifestyle adjustments and follow-up care schedule.” – Orthopedic Surgeon
Conclusion: Making an Informed Decision About Cervical Fusion
Understanding cervical spine fusion is key for those thinking about it. We’ve covered the basics, from what it is to recovery and risks. This helps patients know what to expect.
Choosing cervical fusion means looking at several things. These include the health issue, overall health, and lifestyle. Knowing these details helps patients make a better choice and understand what to hope for.
It’s vital to talk to a healthcare expert about your situation. They can help figure out the best treatment for you. This way, patients can make a smart choice about their care, leading to a better surgery and recovery.
FAQ
What is cervical spine fusion surgery?
Cervical spine fusion surgery joins two or more neck vertebrae together. This helps stabilize the spine and relieves pain.
What conditions are treated with cervical fusion?
This surgery treats many conditions. These include herniated discs, spinal stenosis, spondylolisthesis, and spinal fractures.
What are the different types of cervical spine fusion procedures?
There are several types. These include anterior cervical fusion, posterior cervical fusion, and disc fusion cervical spine interventions.
How long does it take to recover from cervical neck fusion?
Recovery time varies. But, most people recover in several months. Short-term recovery is 0-6 weeks. Medium-term is 6 weeks-6 months. Long-term fusion takes 6 months-1 year or more.
What are the possible complications of cervical fusion?
Complications include infection, nerve damage, and adjacent segment disease. These are among the risks.
How can I minimize the risks of cervical fusion complications?
To reduce risks, follow your surgeon’s advice. Attend all follow-up appointments. Also, make necessary lifestyle changes.
What lifestyle adjustments are necessary after cervical spine fusion?
Patients may need to limit activities. They also need to make changes to prevent disease in other segments.
How does obesity impact cervical spine fusion outcomes?
Obesity can affect surgery success. Patients with obesity may need to change their lifestyle before and after surgery for better results.
What is the success rate of modern cervical fusion surgery?
Success rates vary. Traditional single and two-level fusions have a 90% success rate. Multi-level fusions have a success rate of 61% or higher.
What are the alternatives to cervical fusion surgery?
Alternatives include conservative management and physical therapy. These depend on the condition and patient needs.
What is cervical spine fusion surgery?
Cervical spine fusion surgery joins two or more neck vertebrae together. This helps stabilize the spine and relieves pain.
What conditions are treated with cervical fusion?
This surgery treats many conditions. These include herniated discs, spinal stenosis, spondylolisthesis, and spinal fractures.
What are the different types of cervical spine fusion procedures?
There are several types. These include anterior cervical fusion, posterior cervical fusion, and disc fusion cervical spine interventions.
How long does it take to recover from cervical neck fusion?
Recovery time varies. But, most people recover in several months. Short-term recovery is 0-6 weeks. Medium-term is 6 weeks-6 months. Long-term fusion takes 6 months-1 year or more.
What are the possible complications of cervical fusion?
Complications include infection, nerve damage, and adjacent segment disease. These are among the risks.
How can I minimize the risks of cervical fusion complications?
To reduce risks, follow your surgeon’s advice. Attend all follow-up appointments. Also, make necessary lifestyle changes.
What lifestyle adjustments are necessary after cervical spine fusion?
Patients may need to limit activities. They also need to make changes to prevent disease in other segments.
How does obesity impact cervical spine fusion outcomes?
Obesity can affect surgery success. Patients with obesity may need to change their lifestyle before and after surgery for better results.
What is the success rate of modern cervical fusion surgery?
Success rates vary. Traditional single and two-level fusions have a 90% success rate. Multi-level fusions have a success rate of 61% or higher.
What are the alternatives to cervical fusion surgery?
Alternatives include conservative management and physical therapy. These depend on the condition and patient needs.


































