At Liv Hospital, we know that persistent discomfort after spine surgery can really hurt. It can make a big difference in how well a patient lives. We aim to give top-notch healthcare and support to patients from all over.
Studies have found many reasons for postoperative back pain. For example, a study in the Niagara Gazette looks into using music to help manage pain.
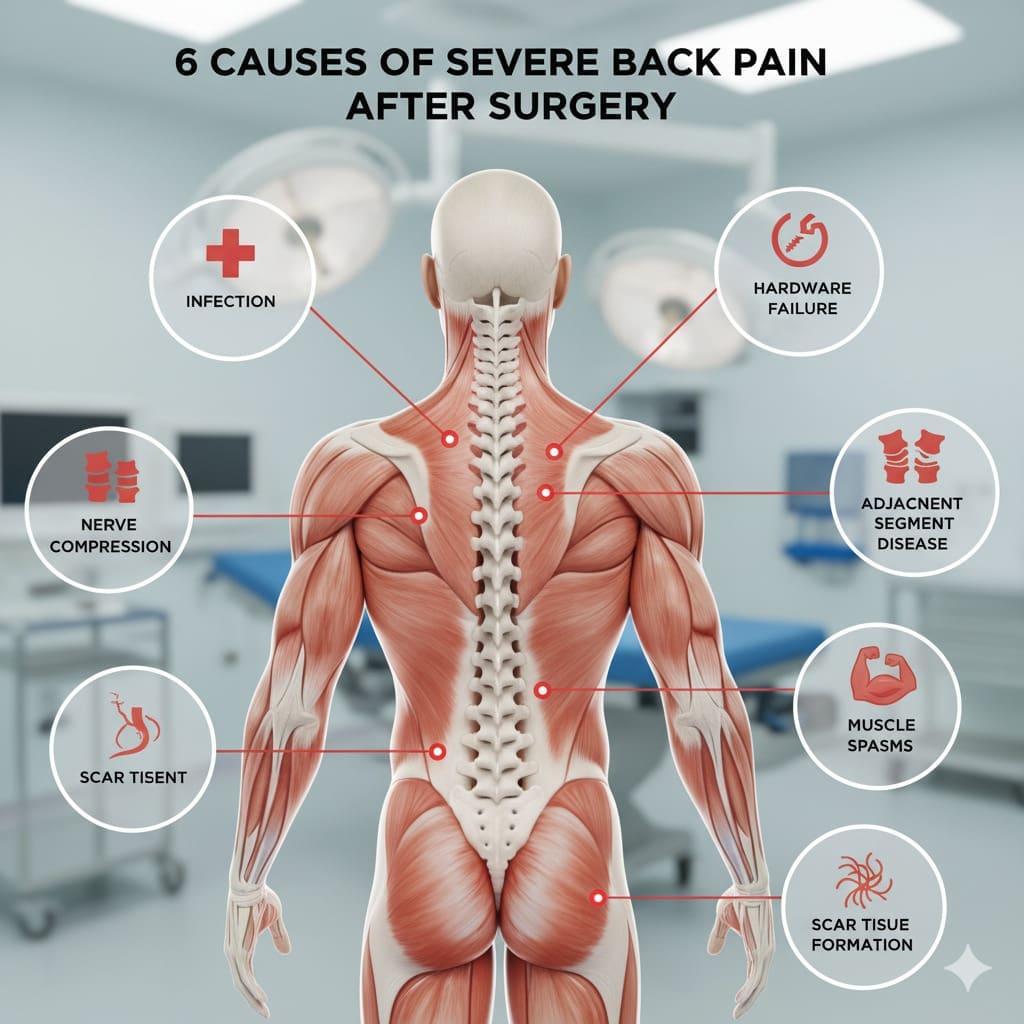
In this article, we’ll look at the six main reasons for severe back pain after surgery. We’ll also talk about how to deal with them. Our team is here to help patients get better and feel strong again.
Key Takeaways
- Understanding the causes of postoperative back pain is key to managing it well.
- Liv Hospital offers full care for patients from abroad.
- Methods like music therapy can help with pain.
- Our team is here to support patients on their recovery path.
- Good management can really help patients get better.
The Reality of Post-Surgical Back Pain

Many patients face back pain after surgery, which can greatly affect their recovery. This pain can make a big difference in their life and well-being.
Looking at the numbers, a lot of patients deal with back pain after surgery. For example, up to 40% of those who have lumbar spine surgery may have ongoing lower back pain.
Statistics on Post-Operative Pain Prevalence
Post-operative pain is common among many patients. The amount of back pain after surgery can vary. It depends on the surgery type and the patient’s health.
| Surgery Type | Prevalence of Post-Operative Back Pain |
|---|---|
| Lumbar Spine Surgery | Up to 40% |
| Discectomy | 20-30% |
| Spinal Fusion | 30-40% |
Normal vs. Abnormal Recovery Patterns
It’s important to know the difference between normal and abnormal recovery patterns. Normally, pain should lessen as you get better. But, some may have pain that gets worse or doesn’t go away, which could mean there’s a problem.
Abnormal recovery patterns include pain that gets worse, new symptoms, or not getting better. It’s key for patients to stay in touch with their doctors to watch their recovery and fix any issues fast.
For those with severe back pain after surgery, there are treatment options for postoperative back pain. These include physical therapy, medicine, and sometimes more surgery. The aim is to help with severe back pain relief and improve their life quality.
In summary, postoperative back pain is a big problem for many patients. By knowing the stats and understanding normal versus abnormal recovery, we can help those with back pain after surgery better.
Understanding Severe Back Pain After Surgery

It’s important to know why back pain happens after surgery. Back pain after surgery can show up in different ways. Understanding the reasons helps in treating it properly.
Defining Post-Surgical Pain Complications
Post-surgical pain complications are problems that can happen after surgery. These can include surgical technique, patient health, and post-operative care. Finding these issues early is key to fixing them.
“Pain is not just a simple feeling,” say pain experts. “It’s a complex mix of physical and emotional feelings.” Knowing this helps in tackling post-surgical pain.
The 40% Statistic: Why Lower Back Pain Persists
About 40% of patients keep feeling lower back pain after surgery. This shows how hard it is to manage back pain after surgery. Reasons include incomplete fusion, instability, or stress on adjacent vertebrae. Knowing these reasons helps in finding better treatments.
When to Seek Medical Attention
Patients should know when to see a doctor for back pain after surgery. Signs that mean you need to see a doctor include increasing pain intensity, neurological symptoms, or failure to improve with conservative management. Getting help quickly can stop more problems and help you get better.
Being aware of possible complications and knowing when to get help is important. Managing severe back pain after surgery needs a full approach. This includes physical, emotional, and psychological aspects of pain.
Failed Back Surgery Syndrome (FBSS)
Failed Back Surgery Syndrome, or FBSS, is a tough issue to handle. It happens when back surgery doesn’t fix the pain. Both patients and doctors face big challenges with this condition.
FBSS means persistent pain that doesn’t go away after surgery. This pain can feel the same as the pain before the surgery.
Diagnostic Criteria for FBSS
To diagnose FBSS, we look at the patient’s history, symptoms, and past surgeries. We check for pain that’s similar to or the same as before surgery.
Our diagnostic process includes a detailed physical exam and imaging like MRI or CT scans. We might also do more tests to find other pain causes.
Common Causes and Risk Factors
Several things can lead to FBSS. Poor surgery technique, not fully understanding the problem, and patient health are big factors. We focus on these to create better treatment plans.
Other risks include pre-existing conditions like degenerative disc disease or spinal stenosis. Knowing these helps us target our treatments better.
Management Strategies and Treatment Options
Handling FBSS needs a team effort. We use physical therapy, medicine, and sometimes more surgery. Our goal is to reduce pain and improve life quality for each patient.
Treatment might include pain management drugs, physical therapy, or more surgery in some cases.
Scar Tissue Formation and Fibrosis
After surgery, the body heals by forming scar tissue. This can sometimes lead to fibrosis. Scar tissue is made of collagen and other connective tissue. While it’s a normal part of healing, too much can cause problems.
The Mechanism of Post-Surgical Scarring
Surgery causes tissue trauma, starting the healing process. The body repairs the damage by forming scar tissue. Sometimes, this scar tissue grows too much, causing fibrosis.
Understanding how scar tissue forms is key to managing it. Knowing what causes excessive scarring helps healthcare providers prevent and treat it better.
How Scar Tissue Causes Pain
Scar tissue can cause pain in several ways. It can stick to nerves, causing tension and irritation. This can lead to chronic pain, which is hard to treat.
Patients with long-lasting pain after surgery might have fibrosis or nerve irritation. They should see a doctor to find out why and get the right treatment.
Therapeutic Approaches for Scar-Related Pain
There are many ways to manage pain from scar tissue. We use physical therapy, injections, minimally invasive procedures, and medicine to help.
- Physical therapy to improve mobility and reduce scar tissue adhesions
- Targeted injections to reduce inflammation and relieve pain
- Minimally invasive procedures to break up scar tissue
- Pharmacological interventions to manage pain and inflammation
The table below shows the different ways we treat scar-related pain:
| Therapeutic Approach | Description | Benefits |
|---|---|---|
| Physical Therapy | Improves mobility, reduces scar tissue adhesions | Non-invasive, promotes healing |
| Targeted Injections | Reduces inflammation, relieves pain | Quick relief, minimally invasive |
| Minimally Invasive Procedures | Breaks up scar tissue | Effective for severe scar tissue |
| Pharmacological Interventions | Manages pain and inflammation | Wide range of options, can be tailored to patient needs |
By understanding and treating scar tissue, we can help patients with severe back pain relief.
Inadequate or Failed Spinal Fusion
Spinal fusion surgery aims to stabilize the spine and ease pain. But, if it fails, patients may face ongoing pain and mobility issues. This can happen when the spine doesn’t fuse correctly.
Signs of Incomplete Fusion
Spotting signs of incomplete fusion early is key. Look out for:
- Persistent or worsening back pain
- Limited mobility or stiffness in the spine
- Instability or abnormal movement at the fusion site
- Hardware failure or loosening of surgical implants
Factors Contributing to Fusion Failure
Several things can cause spinal fusion to fail. These include:
| Factor | Description |
|---|---|
| Inadequate Surgical Technique | Poor surgery or not enough stabilization can cause failure. |
| Patient-Specific Factors | Smoking, diabetes, or osteoporosis can hinder bone healing. |
| Hardware Failure | Failed or loose hardware can ruin the fusion. |
Treatment Options for Fusion Complications
Dealing with fusion problems needs a detailed plan. Options might include:
- Revision surgery to fix hardware issues or instability
- Physical therapy to boost mobility and strength
- Pain management, like meds or procedures
- Changes in lifestyle, like quitting smoking and better nutrition
If you’re in pain or have symptoms after spinal fusion, talk to your doctor. They can help figure out the best steps to take.
Nerve Damage and Persistent Neuropathic Pain
Nerve damage during surgery is a big worry. It can cause long-lasting neuropathic pain. This pain can bother patients long after their surgery. It’s important to know about nerve injuries, how to spot neuropathic pain, and what treatments are available.
Types of Surgical Nerve Injuries
Surgical nerve injuries can be different in how severe they are. They are mainly split into three types: neuropraxia, axonotmesis, and neurotmesis. Neuropraxia is the least severe, where the nerve is okay but can’t send signals well. Axonotmesis damages the axon but keeps the nerve’s connective tissue safe. Neurotmesis is the worst, where the nerve is cut completely.
Knowing these types helps doctors figure out the best treatment. A study on Patient Care Online shows that treating pain right away is key to avoiding long-term problems.
Identifying Neuropathic Pain Symptoms
Neuropathic pain has its own set of symptoms. These include burning, shooting pain, and being extra sensitive to touch. Patients might also feel numbness or tingling. Spotting these symptoms early is key to starting the right treatment.
“Neuropathic pain is a complex condition that requires a complete treatment plan. This plan should include both medicines and other methods.”
Multimodal Approaches to Nerve Pain Management
Handling neuropathic pain well often means using many different treatments. This mix can include medicines like anticonvulsants and antidepressants, procedures like nerve blocks, and other methods like physical therapy and therapy for the mind.
| Treatment Modality | Description | Benefits |
|---|---|---|
| Pharmacological Treatments | Use of medicines like anticonvulsants and antidepressants | Helps manage pain symptoms well |
| Interventional Procedures | Nerve blocks and other injections to stop pain signals | Gives focused pain relief |
| Non-Pharmacological Interventions | Physical therapy, therapy for the mind | Boosts function and helps with coping |
We know that every person’s experience with neuropathic pain is different. So, we make treatment plans that fit each person’s needs. By using a wide range of treatments, we can help those with nerve damage and long-lasting neuropathic pain a lot.
Adjacent Segment Disease
After spinal fusion surgery, the spine’s segments next to the fusion can get affected. This is called adjacent segment disease. It happens because the fusion changes how the spine moves, putting more stress on the nearby segments.
Biomechanical Changes After Spinal Surgery
Spinal fusion surgery aims to stabilize the spine and ease pain. But it can also change how the spine works. The fusion of vertebrae changes the way the spine moves and handles stress. This can lead to more stress and pain in the segments next to the fusion site.
The main biomechanical changes include:
- Increased stress on adjacent discs and facet joints
- Altered motion patterns in the spine
- Potential for accelerated degeneration
Recognizing Adjacent Segment Problems
Finding out if you have adjacent segment disease can be tricky. The symptoms might seem like they did before surgery. Signs include:
- Pain or discomfort in the neck or back
- Radiating pain into the arms or legs
- Neurological symptoms such as numbness or weakness
Imaging tests like MRI or CT scans are key to confirming the disease and how bad it is.
Conservative and Surgical Management Options
How to manage adjacent segment disease depends on how bad the symptoms are. First, doctors might suggest trying non-surgical treatments. These include physical therapy, pain meds, and changes in lifestyle.
If these don’t work, surgery might be needed. Surgery options include:
- Extending the original fusion to include the affected segment
- Revision surgery to fix problems with the original fusion
- Minimally invasive procedures to manage symptoms
We help patients choose the best treatment plan for their situation.
Physical Rehabilitation for Post-Surgical Back Pain
A good physical rehabilitation plan is key to lessening post-surgical back pain and boosting mobility. We know that physical therapy is a big part of post-surgery care. It helps manage back pain and improves patient results.
Evidence-Based Physical Therapy Protocols
Physical therapy is a mainstay of post-surgery rehab. We use proven protocols that fit each patient’s needs. These plans mix manual therapy, exercises, and lessons on good posture and body mechanics.
Manual therapy methods, like massage and joint mobilization, can cut down pain and stiffness. Exercise programs aim to boost strength, flexibility, and movement. These are vital for spinal support and better mobility.
Strengthening Exercises for Spinal Support
Strengthening the muscles that back the spine is a big part of physical therapy. We suggest exercises that work the core muscles, like the abs and back. These muscles are key for spine support.
- Pelvic tilts
- Bridge exercises
- Planks
It’s important to do these exercises with a physical therapist. They make sure you’re doing them right and don’t make the pain worse.
Gradual Return to Activities
Going back to normal activities slowly is key for a good recovery. We tell patients to start with easy activities and slowly add more intensity and time. This should be based on how they feel and how much pain they’re in.
It’s important to avoid heavy lifting, bending, or twisting, at least in the beginning. Patients should also watch their posture and body mechanics to avoid putting extra strain on their back.
Medication and Interventional Pain Management
Managing pain after surgery includes using medicine and special treatments. It’s key to help patients feel better and live better lives.
Pharmacological Approaches to Post-Surgical Pain
Medicine is a big part of fighting post-surgical pain. We use different drugs, like:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain
- Opioids for severe pain, used carefully to avoid addiction
- Adjuvant medications like gabapentinoids for nerve pain
A study in the Journal of Pain Research shows that using many medicines at once can help. It can make pain less and cut down on opioid use.
“Multimodal analgesia has been shown to improve pain control and reduce opioid-related side effects.”
| Medication Type | Primary Use | Benefits |
|---|---|---|
| NSAIDs | Reducing inflammation and pain | Works well for mild to moderate pain, cuts down on opioid use |
| Opioids | Severe pain management | Very effective for bad pain, starts working fast |
| Gabapentinoids | Neuropathic pain | Good for nerve pain, not addictive |
Injection Therapies and Nerve Blocks
Some patients find relief with injection treatments and nerve blocks. These methods target pain sources, giving relief with fewer side effects.
Nerve blocks involve injecting local anesthetics or steroids near nerves to block pain signals. Epidural injections are often used for back pain.
Emerging Treatments for Chronic Pain
New treatments for chronic pain are being studied. Some promising ones include:
- Stem cell therapy, which might help fix damaged tissues
- Platelet-rich plasma (PRP) therapy, to help healing
- Advanced neuromodulation techniques, like spinal cord stimulation
We’re always looking for new ways to manage pain. Our goal is to find the best treatment for each patient.
Psychological Approaches to Managing Chronic Back Pain
Chronic back pain is more than just physical. It also affects our minds. To manage it well, we need to understand how our body and mind work together.
The Mind-Body Connection in Pain Perception
The way we feel pain is linked to our mind and body. Chronic back pain can get worse when we’re stressed, anxious, or depressed. It’s a cycle that’s hard to stop. Knowing this helps us find better ways to handle pain.
Studies show that our thoughts and feelings can change how we feel pain. People who stay positive and find ways to cope tend to handle pain better. Those who feel hopeless or negative often struggle more.
Cognitive Behavioral Therapy for Pain Management
Cognitive Behavioral Therapy (CBT) is a key tool for managing chronic back pain. It helps people change their negative thoughts and behaviors that make pain worse.
CBT teaches patients to deal with their pain in better ways. It helps them live their lives more fully, not controlled by pain. This therapy lets people take charge of their pain management.
- CBT helps in identifying negative thought patterns.
- It aids in developing coping strategies.
- CBT promotes a positive outlook on life despite chronic pain.
Stress Reduction Techniques
Reducing stress is key to managing chronic back pain. Meditation, deep breathing exercises, and yoga can help lower stress and ease pain.
These methods do more than just help with pain. They also make us feel better overall. Adding them to our daily lives can help us deal with chronic back pain better.
In summary, dealing with chronic back pain requires a psychological approach. By understanding the mind-body link, using CBT, and practicing stress reduction, we can improve our lives a lot.
Advanced Treatment Options at Specialized Centers
Liv Hospital is a leader in treating severe back pain after surgery. We use the latest treatments available. Our goal is to provide top-notch healthcare through our rigorous care pathways and updated protocols.
Liv Hospital’s Approach to Post-Surgical Pain
At Liv Hospital, we take a detailed approach to post-surgical pain. Our team uses the newest pain management techniques. We focus on each patient’s needs, making sure they get the best care.
Multidisciplinary Pain Management Teams
Our pain management teams include experts from many fields. These include anesthesiology, physical medicine, and rehabilitation, as well as psychologists and support staff. Together, they create effective treatment plans for our patients.
| Specialty | Role in Pain Management |
|---|---|
| Anesthesiology | Provides expertise in interventional pain procedures |
| Physical Medicine and Rehabilitation | Focuses on restoring function and managing pain through physical means |
| Psychology | Supports patients in coping with chronic pain and improving mental health |
International Best Practices and Protocols
We follow international best practices in pain management. This ensures our patients get safe and effective care. Our commitment to staying current with research helps us offer the latest treatments.
Our treatment protocols are designed to be flexible and adaptive. This lets us adjust our approach for the best results. We combine advanced treatments with a caring environment to improve our patients’ lives.
Conclusion: Creating a Comprehensive Recovery Plan
Creating a detailed recovery plan is key for dealing with severe back pain after surgery. We’ve looked at why back pain happens after surgery, like Failed Back Surgery Syndrome and nerve damage.
A plan should mix physical therapy, medicine, and pain management techniques. At Liv Hospital, we’ve seen how teams help patients get better faster.
It’s important to work with doctors to make a plan that fits you. This plan should meet your unique needs for the best results.
Understanding why back pain happens and having a good recovery plan can greatly improve your life. It helps you recover better and feel better sooner.
What are the common causes of severe back pain after surgery?
Severe back pain after surgery can come from many sources. These include post-surgical pain, failed back surgery syndrome, and scar tissue. Other causes are inadequate spinal fusion, nerve damage, and disease in adjacent segments.
How can I manage severe back pain after surgery?
Managing severe back pain after surgery needs a full approach. This includes physical therapy, medication, and pain management techniques. Psychological support is also key.
What is failed back surgery syndrome, and how is it treated?
Failed back surgery syndrome is a complex issue. It needs a detailed treatment plan. We will cover what it is, its causes, and how to manage it.
Can scar tissue formation cause pain after surgery?
Yes, scar tissue and fibrosis can lead to pain after surgery. We will explain how scarring happens and how to treat scar-related pain.
What are the signs of incomplete fusion after spinal surgery?
Signs of incomplete fusion include ongoing pain, instability, and limited movement. We will talk about why fusion fails and how to treat it.
How can nerve damage cause persistent pain after surgery?
Nerve damage during surgery can cause long-lasting pain. We will discuss the types of nerve injuries, symptoms, and how to manage nerve pain.
What is adjacent segment disease, and how is it managed?
Adjacent segment disease is a risk after spinal surgery. We will explain the biomechanical changes, signs, and management options.
How can physical rehabilitation help manage post-surgical back pain?
Physical rehabilitation is vital for post-surgical back pain. We will share evidence-based therapy, strengthening exercises, and gradual activity return strategies.
What are the available treatment options for managing chronic back pain?
We will discuss pharmacological treatments, injection therapies, and nerve blocks for post-surgical pain. We will also cover emerging chronic pain treatments.
How can psychological approaches help manage chronic back pain?
Psychological methods are key for chronic back pain. We will talk about the mind-body connection, cognitive behavioral therapy, and stress reduction techniques.
What advanced treatment options are available at Liv Hospital for managing post-surgical pain?
At Liv Hospital, we offer advanced pain management. This includes multidisciplinary teams and international best practices.
References
PubMed Central (NCBI): Identifying Pain after Lumbar Spine Surgery (Specific PMC ID)