Last Updated on November 27, 2025 by Bilal Hasdemir

When it comes to precision, safety, and quick recovery, mastering the total laparoscopic hysterectomy is key. At Liv Hospital, our team of experts is committed to providing top-notch care and support during this life-changing surgery.
TLH is a minimally invasive surgery that removes the uterus through a laparoscope. It offers many benefits, like shorter recovery times and less pain after surgery. Our specialists will walk you through the steps, explaining the important parts and the advantages of this advanced treatment.
Key Takeaways
- TLH is a minimally invasive surgical procedure.
- The procedure offers benefits such as reduced recovery time.
- Our specialists provide step-by-step guidance on the TLH procedure.
- Patient-centered care is our top priority.
- TLH requires precision and skill.
Understanding Total Laparoscopic Hysterectomy (TLH)

We dive into Total Laparoscopic Hysterectomy, a method that’s becoming more popular. It’s known for being less invasive. This surgery is used to treat issues like fibroids, endometriosis, and heavy bleeding.
Definition and Clinical Indications
Total Laparoscopic Hysterectomy means removing the uterus through small incisions in the belly. It doesn’t involve cutting the vagina. It’s for those with fibroids, endometriosis, adenomyosis, or bleeding that can’t be managed with other treatments.
TLH is used for many reasons. It’s getting more common as doctors get better at it. Some main reasons include:
- Uterine fibroids causing big problems
- Endometriosis with bad pain or trouble getting pregnant
- Adenomyosis leading to heavy periods
- Bleeding that doesn’t stop with other treatments
Advantages of TLH Over Other Hysterectomy Methods
TLH has many benefits over other types of hysterectomies. These advantages are:
| Advantages | Description |
|---|---|
| Minimally Invasive | It uses smaller cuts, causing less damage to the belly and tissues. |
| Less Postoperative Pain | Because of the small cuts, there’s less pain after surgery. |
| Faster Recovery | Patients get back to normal faster, thanks to the smaller cuts. |
| Better Cosmetic Results | The small cuts mean less scarring than with open surgery. |
In summary, Total Laparoscopic Hysterectomy is a big step forward in gynecology. It’s a safe, effective, and less invasive option compared to older methods. As surgery keeps improving, TLH will likely stay a key choice for many gynecological issues.
Current Statistics and Outcomes of Laparoscopic Hysterectomy
Laparoscopic hysterectomy is becoming a top choice for many women. It offers benefits over traditional open hysterectomy. The stats on laparoscopic hysterectomy show a big change in gynecological surgery.
Recent studies show the positive outcomes of laparoscopic total hysterectomy. These include shorter recovery times and fewer complications. As technology improves, more women are choosing laparoscopic hysterectomy. This is because it’s less invasive and allows for a quicker return to daily life.
Prevalence and Success Rates
The use of laparoscopic hysterectomy is increasing. More surgeons are learning this technique. Success rates are high, with low complication rates and high patient satisfaction.
Studies show that patients have less pain and shorter hospital stays after laparoscopic total hysterectomy. These favorable outcomes make the laparoscopic method more popular.
The field of gynecological surgery is always changing. The role of laparoscopic hysterectomy will likely grow. This is thanks to new surgical techniques and technology.
Pre-Operative Patient Assessment and Selection
Assessing patients before surgery is key to making sure they’re right for Total Laparoscopic Hysterectomy (TLH). We check each patient carefully to see if they’re good candidates for this surgery.
Evaluating Surgical Candidates
We look at several important things when checking if someone can have surgery. This includes their medical history, how they’re doing now, and any surgeries they’ve had before.
- Medical history, including previous illnesses and chronic conditions
- Current health status, with a focus on cardiovascular and respiratory health
- Previous surgical procedures, which can impact the complexity of the TLH
By looking at these things, we can figure out the best plan for each patient.
Essential Pre-Operative Imaging and Laboratory Tests
To check if a patient is ready for TLH, we use different tests before surgery.
- Imaging tests, such as ultrasound or MRI, to see the uterus and nearby areas
- Laboratory tests, like blood work and urinalysis, to check overall health
These tests help us find any problems that might affect the surgery or how the patient recovers.
Operating Room Setup and Equipment
We make sure our operating rooms have the latest technology. They are also staffed by experienced professionals. This setup helps make the Total Laparoscopic Hysterectomy (TLH) procedure a success.
Essential Laparoscopic Instruments
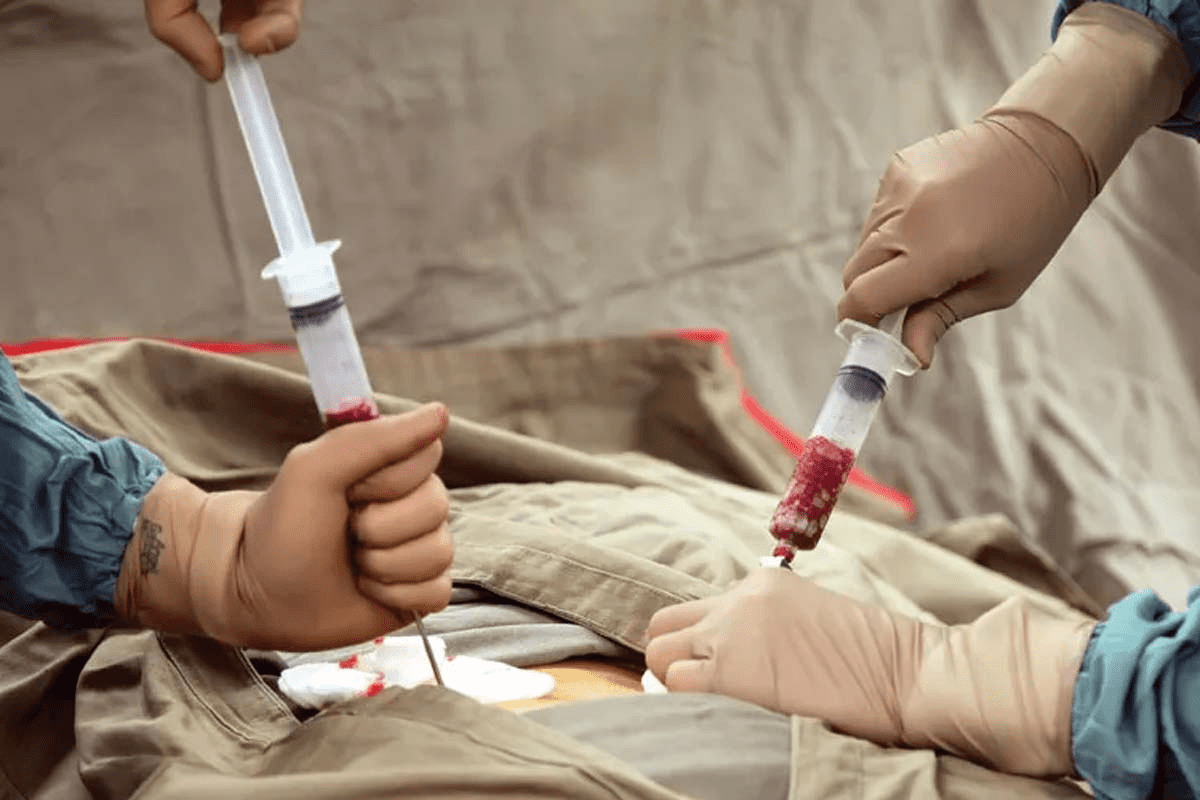
Choosing the right laparoscopic instruments is key for TLH success. They allow for precise dissection and reduce tissue damage. Important tools include:
- Laparoscope: It lets the surgeon see the surgical area.
- Trocars: These tools help insert instruments into the abdomen.
- Graspers and dissectors: They help the surgeon move and cut tissue.
- Energy devices: Used for cutting and stopping bleeding.
Operating Room Configuration
A well-set-up operating room helps the surgical team work better. This reduces the chance of problems. Important factors include:
- Lighting: Good lighting is needed for clear vision.
- Equipment positioning: Equipment is placed to avoid clutter and make it easy to reach.
- Operating room layout: It’s designed to help the team move smoothly.
Anesthesia Protocol and Patient Positioning
Effective anesthesia and precise patient positioning are key for a successful Total Laparoscopic Hysterectomy. We will look at the important factors for both to ensure a smooth procedure.
Anesthetic Considerations for TLH
The choice of anesthesia for TLH is very important. General anesthesia is often used because it allows for controlled breathing and muscle relaxation. But, some studies show that regional anesthesia can be a good option in some cases. It can lead to less pain after surgery and a quicker recovery.
When setting up the anesthesia plan, we must think about the patient’s health. This includes any health issues that could affect how they react to anesthesia. Careful monitoring of the patient’s vital signs during surgery is key to quickly handle any problems.
Optimal Patient Positioning Techniques
Proper patient positioning is essential for a smooth surgery and to avoid complications. The lithotomy position is often used for TLH because it gives great access to the pelvic area. It’s important to make sure the patient’s legs are well-supported and to avoid putting pressure on any points to prevent nerve damage.
Besides the lithotomy position, Trendelenburg positioning is sometimes used. It helps by moving the intestines away from the pelvis, making it easier to see during surgery. But, we must avoid extreme positions that could cause discomfort or harm to the patient.
Initial Access and Strategic Trocar Placement
Getting into the body and placing trocars is key in a TLH surgery. It’s important to do it right to avoid problems and get a clear view.
Primary Port Insertion Techniques
There are two main ways to put in the first port. The open method makes a small cut and lets the surgeon see inside. The closed method uses a needle to inflate the area before the port goes in. Which method is best depends on the patient and the surgeon.
For those who have had surgery before, we suggest the open technique to avoid adhesions. The closed method is quicker and better for those without previous surgeries.
Secondary Port Placement Strategies
Once the first port is in, the next ones are put in with the surgeon watching. They are placed carefully to reach the uterus and other areas well. The goal is to move instruments easily without straining the ports or the patient.
The second ports go in the lower parts of the abdomen. Where they go depends on the surgery and the surgeon’s style. It’s important to keep them away from the first port and bony areas for comfort and efficiency.
For more info on laparoscopic hysterectomy, check out this chapter on laparoscopic surgery.
Uterine Manipulation and Round Ligament Division
Uterine manipulation and round ligament division are key steps in total laparoscopic hysterectomy. They help surgeons get the best view and make the surgery go smoothly.
Selecting and Placing the Uterine Manipulator
We use a uterine manipulator to move the uterus in a controlled way. This makes it easier to see and work on the pelvic area. The right uterine manipulator depends on the patient’s body and the surgeon’s choice.
Techniques for Round Ligament Division
Dividing the round ligament is a first step in TLH. We use special laparoscopic tools for precise cutting. This cuts down on bleeding and keeps the area clear for surgery. We usually use electrocautery or advanced bipolar devices for this.
Mastering uterine manipulation and round ligament division helps surgeons do better in total laparoscopic hysterectomy. This means patients get the benefits of less invasive surgery.
FAQ
What is Total Laparoscopic Hysterectomy (TLH)?
Total Laparoscopic Hysterectomy (TLH) is a surgery where the uterus is removed through small cuts in the belly. This is done using a laparoscope.
What are the benefits of TLH compared to other hysterectomy methods?
TLH has many advantages. It causes less pain after surgery, you can leave the hospital sooner, and you recover faster. This is compared to open surgery or other methods.
What are the key considerations for pre-operative patient assessment and selection for TLH?
Doctors check a patient’s health and medical history before TLH. They look for any issues that might make surgery harder, like adhesions or a big uterus.
What imaging and laboratory tests are essential before undergoing TLH?
Tests like ultrasound and MRI are important. Blood tests, like a complete blood count (CBC), also help plan the surgery.
What equipment is required for a TLH procedure?
You need a laparoscope and special tools like graspers and dissectors. A uterine manipulator and an electrosurgical unit are also needed.
How is the patient positioned during TLH?
The patient lies on their back with their legs in stirrups. This position helps the surgeon see the pelvic area better.
What are the techniques used for primary and secondary trocar placement in TLH?
The first port is placed at the belly button. The other ports are put in under the surgeon’s watchful eye. The choice depends on the patient’s body and the surgeon’s preference.
How is the uterus manipulated during TLH?
A uterine manipulator helps move and support the uterus. This makes it easier to remove during the surgery.
What are the considerations for round ligament division during TLH?
The round ligament is cut to get to the back of the pelvis. This is done with care to avoid harming nearby tissues.
What are the success rates and outcomes of TLH?
TLH is very successful with low complication rates. Experienced surgeons make it safer, with less pain and quicker healing.
What is the difference between TLH and other types of hysterectomy?
TLH is different because it’s a minimally invasive surgery. It uses laparoscopy to remove the uterus, unlike other methods.
Is TLH a safe procedure?
TLH is safe when done by skilled surgeons. It has a low risk of serious problems. But, as with any surgery, there are some risks.
References
- Pados, G., Becker, S., Rovira Negre, R., Rabischong, B., Ferreira, H., & Rossitto, C. (2019). Surgical steps of total laparoscopic hysterectomy: Part 1: benign disease. Facts, Views & Vision in ObGyn, 11(2), 103-110. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6897515/ PMC+1
- Textbook of Simplified Laparoscopic Hysterectomy (n.d.). Chapter 14 – The ten operative steps. In Simplified laparoscopic hysterectomy: Practical, safe and economic methodology. Retrieved from https://www.glowm.com/simplified-laparoscopic-hysterectomy/chapter-14—the-ten-operative-steps Glowm
- Einarsson, J. I., & Suzuki, Y. (2009). Total laparoscopic hysterectomy: 10 steps toward a successful procedure. Rev Obstet Gynecol, 2(1), 57-64. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2673000/ PMC+1