Last Updated on November 4, 2025 by mcelik

Shoulder pain is common among people of all ages and activity levels. Shoulder bursitis is a condition that can cause a lot of discomfort. It affects the fluid-filled sacs (bursae) that cushion the joints. These sacs help reduce friction between bone and soft tissue.
We know how much it can affect your daily life. That’s why we’re here to give you more information about this condition.
Key Takeaways
- Shoulder bursitis is a condition that causes pain and inflammation in the shoulder.
- It can affect individuals of all ages and activity levels.
- Repetitive shoulder movements can contribute to the development of shoulder bursitis.
- Understanding the causes and symptoms is key for effective management.
- Seeking medical attention is important for proper diagnosis and treatment.
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.

The shoulder is a complex structure that allows for a wide range of movements. This makes it both versatile and prone to injuries. Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
The shoulder joint is surrounded by muscles, tendons, and ligaments. These provide stability and help with movement. The rotator cuff, a group of muscles and tendons, is key. It stabilizes the shoulder joint and enables movements like lifting and rotating the arm.
The Role of Bursae in the Shoulder
When bursae become inflamed or irritated, it can lead to bursitis. This causes pain and limited mobility in the shoulder. Understanding bursae’s role in the shoulder is essential. It helps us see how bursitis occurs and how to treat it effectively.
What is Bursitis and Shoulder Connection

It’s important to know about bursitis and how it affects the shoulder. Bursitis is when the bursae, fluid-filled sacs, get inflamed. These sacs cushion joints and reduce friction between bones, tendons, and ligaments.
Definition of Bursitis
Bursitis happens when one or more bursae get inflamed. This can be due to repetitive motion, direct trauma, or infection. It causes a lot of pain and discomfort, making daily life harder. Bursitis definition also includes the symptoms and how it affects the joint.
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Bursitis in the shoulder can really hurt the joint’s function. It can cause pain when you move your arm, make it harder to move, and weaken the muscles around it. Shoulder bursitis symptoms include pain when lifting, tenderness, and swelling.
The link between bursitis and the shoulder is complex. It involves the bursae, tendons, and ligaments. When bursitis happens, it might mean there’s a bigger problem that needs fixing.
Understanding the bursitis and shoulder connection is key to treating it right. It’s not just about easing the pain but also fixing the root cause. Treatment can range from rest and physical therapy to medication and sometimes surgery.
Types of Shoulder Bursitis
It’s important to know the different types of shoulder bursitis for proper treatment. Shoulder bursitis can be divided by where and how the inflammation happens.
Subacromial Bursitis
Subacromial bursitis happens when the bursa under the acromion gets inflamed. This usually comes from repetitive overhead movements. It causes shoulder pain and makes it hard to move the shoulder.
Subdeltoid Bursitis
The symptoms of subdeltoid bursitis can be like those of subacromial bursitis. So, getting a correct diagnosis is key.
Scapulothoracic Bursitis
Scapulothoracic bursitis is a rarer form that affects the bursa between the scapula and the chest wall. It causes pain between the shoulder blade and the chest wall. This pain is often mistaken for other issues.
Getting a correct diagnosis is vital to treat scapulothoracic bursitis right. This ensures the right treatment.
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Common Causes of Shoulder Bursitis
Knowing what causes shoulder bursitis is key to preventing and treating it. Shoulder bursitis can come from many sources. These include repetitive strain, direct trauma, and certain medical conditions.
Repetitive Motion Injuries
Repetitive motion injuries often lead to shoulder bursitis. Activities like throwing, lifting, or swimming can irritate the bursae. This leads to inflammation.
Jobs or sports that require frequent arm movements raise the risk of bursitis. For example, athletes in sports like tennis or baseball are at higher risk. This is because their activities involve a lot of repetitive movements.
Traumatic Injuries
Traumatic injuries to the shoulder can also cause bursitis. A direct blow or a fall onto the shoulder can irritate or inflame the bursae.
Such trauma can lead to acute bursitis, which may resolve with rest and treatment. But severe or repeated trauma can cause chronic bursitis. This requires more extensive management.
Infection and Other Medical Conditions
In some cases, shoulder bursitis is caused by infection or underlying medical conditions. Septic bursitis occurs when bacteria infect the bursae. This often happens through a puncture wound or direct infection.
Certain medical conditions, like rheumatoid arthritis or gout, can also raise the risk of bursitis. These conditions can cause inflammation in the bursae, leading to bursitis.
| Cause | Description | Examples |
| Repetitive Motion Injuries | Irritation due to repeated movements | Throwing, lifting, swimming |
| Traumatic Injuries | Direct blow or fall onto the shoulder | Contact sports injuries, falls |
| Infection and Medical Conditions | Infection or underlying conditions | Rheumatoid arthritis, gout, septic bursitis |
Risk Factors for Developing Shoulder Bursitis
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Age-Related Factors
Age is a big factor in getting shoulder bursitis. As we get older, our shoulder bursae can lose effectiveness. This makes inflammation and irritation more likely. People over 40 are more at risk because of joint wear and tear.
Occupational Risks
Some jobs raise the risk of shoulder bursitis because of repetitive actions, heavy lifting, or working overhead for long times. Construction workers, painters, and those on assembly lines are at higher risk. It’s important to focus on workplace ergonomics and use proper techniques to lower these risks.
| Occupation | Risk Level | Preventive Measures |
| Construction Worker | High | Regular breaks, proper lifting techniques |
| Painter | Moderate to High | Ergonomic equipment, stretching exercises |
| Assembly Line Worker | Moderate | Task rotation, ergonomic workstation |
Sports and Activities
Playing certain sports or doing activities can also raise the risk of shoulder bursitis. Athletes in overhead sports like tennis, swimming, or baseball face more strain on their shoulders. Heavy lifting or bending also increases the risk.
By knowing these risk factors, people can take steps to prevent shoulder bursitis. They can change their activities, improve their technique, and add preventive exercises to their routine.
Recognizing Shoulder Bursitis Symptoms
Shoulder bursitis shows different symptoms that can change in how bad they are. Spotting these signs early helps manage the condition better.
Pain Patterns and Characteristics
The pain from shoulder bursitis can be sharp or dull. It usually happens around the bursa. Moving the arm can make the pain worse, like when lifting or rotating it. Sometimes, the pain spreads down the arm or keeps you awake at night.
Doctors say pain is the main reason people go to see a doctor. This pain is a big clue about the problem.
Range of Motion Limitations
Shoulder bursitis also makes it hard to move your arm or shoulder. Pain and swelling limit how much you can move. This makes everyday tasks harder.
- It’s hard to lift your arm up high.
- Rotating your shoulder hurts.
- You can’t do things you normally do.
Visual and Physical Signs
There are also signs you can see. Swelling or redness around the shoulder might show up. Sometimes, the area feels warm.
To diagnose shoulder bursitis, we use a detailed approach. This includes physical exams, imaging tests, and ruling out other conditions. Accurate diagnosis is key for effective treatment and care.
Physical Examination Techniques
A thorough physical exam is the first step. We check the shoulder’s range of motion, strength, and pain. Specific tests, like the Neer test and Hawkins-Kennedy test, help spot subacromial bursitis.
We also look for tenderness, swelling, and warmth in the shoulder. Palpation helps pinpoint the affected bursa and its inflammation level.
Imaging Tests
Imaging tests are often needed to confirm the diagnosis. We use X-rays, ultrasound, and MRI to check the shoulder and soft tissues. Ultrasound is great for seeing bursae and inflammation. MRI shows soft tissue details, like tendons and ligaments.
Differential Diagnosis
Differential diagnosis is vital in diagnosing shoulder bursitis. We look at other conditions like rotator cuff tendinitis and osteoarthritis. A detailed patient history and physical exam, along with imaging, help us make the right diagnosis.
This approach ensures we provide the right treatment. Accurate diagnosis is essential for effective therapy and better patient outcomes.
Medical Treatment Options for Shoulder Bursitis
There are many ways to treat shoulder bursitis. Each method has its own good points and things to watch out for. The right treatment depends on how bad the bursitis is, the patient’s health, and the bursitis’s details. We’ll look at the different treatments, like medicine, injections, and surgery.
Medication Approaches
Medicine is key in easing shoulder bursitis symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and swelling. Sometimes, oral corticosteroids are used for quick relief from severe swelling. Pain relievers like acetaminophen also help with pain.
“NSAIDs are a mainstay in treating bursitis,” says a top orthopedic doctor. “They help with both pain and swelling. But, it’s important to think about the risks to the stomach and heart.”
Corticosteroid Injections
- Corticosteroid injections can quickly reduce inflammation.
- They’re often used when other treatments don’t help enough.
- For long-term conditions, more injections might be needed.
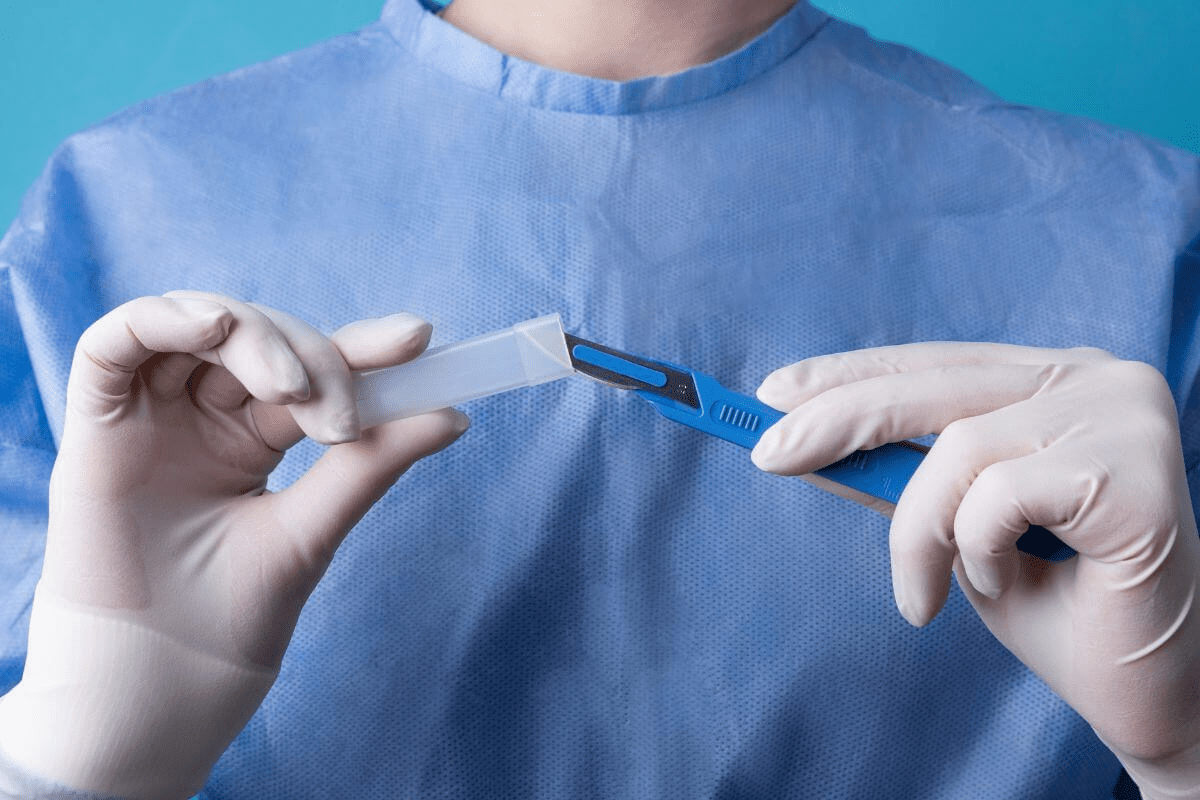
Surgical Interventions
If other treatments don’t work, surgery might be an option. Bursectomy, or removing the inflamed bursa, is one such surgery. This can be done through a small incision, which helps with recovery and lowers risks.
Surgery is usually for very severe bursitis that really affects a person’s life. “Surgery should be a last choice but can really help with chronic bursitis,” says a surgical expert.
Physical Therapy for Shoulder Bursitis
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Therapeutic Exercises
Therapeutic exercises help improve shoulder movement, build muscle, and aid in healing. We create a set of exercises that fit the person’s needs and progress.
- Range of motion exercises to maintain or improve flexibility
- Strengthening exercises for the rotator cuff and scapular stabilizers
- Scapular strengthening exercises to support proper shoulder mechanics
These exercises are adjusted as needed to help the patient gradually get back to normal activities.
Manual Therapy Techniques
Manual therapy is a key part of physical therapy for shoulder bursitis. It helps reduce pain, loosen stiffness, and increase joint movement.
Some techniques we use include:
- Soft tissue mobilization to reduce muscle tension
- Joint mobilization to improve joint mobility
- Myofascial release to address fascial restrictions
Progression and Recovery Milestones
Tracking progress is key in treating shoulder bursitis. We set clear goals to see how well physical therapy is working and make changes as needed.
| Recovery Phase | Milestones |
| Initial Phase | Reduction in pain, improvement in range of motion |
| Intermediate Phase | Strengthening of shoulder muscles, improved function |
| Advanced Phase | Return to normal activities, maintenance of strength and flexibility |
By focusing on these milestones, we can adjust the treatment to meet the individual’s needs. This ensures a successful recovery from shoulder bursitis.
Bursitis and Shoulder Pain: Home Remedies and Self-Care
Home remedies and self-care are key in treating shoulder bursitis. They help ease symptoms and aid in healing. By adding these steps to your daily life, you can feel better faster.
Rest and Activity Modification
Resting and changing your activities are great for shoulder bursitis. Stay away from things that make it worse. Take breaks to rest your shoulder, if you do repetitive tasks.
Avoid heavy lifting and bending to lessen stress on your shoulder. This lets it heal, reducing pain and swelling.
Ice and Heat Therapy
Ice and heat are simple ways to manage bursitis symptoms. Ice reduces swelling and numbs pain. Use an ice pack wrapped in a towel for 15-20 minutes, several times a day.
When the swelling goes down, heat can relax muscles and improve blood flow. Try a warm bath or a heating pad on low, but watch for burns.
Over-the-Counter Pain Management
OTC pain relief is important for bursitis care. Medications like ibuprofen or acetaminophen can lessen pain and swelling. Always check with your doctor before starting any new medicine.
Stick to the recommended dosage and watch for side effects. If your pain doesn’t get better or gets worse, see a doctor to adjust your treatment.
Using these home remedies and self-care tips can greatly help with shoulder bursitis. They can improve your life quality. But, always get medical advice for the best treatment and diagnosis.
Prevention Strategies for Shoulder Bursitis
To prevent shoulder bursitis, we need to use proper techniques, work ergonomically, and make lifestyle changes. Knowing what causes shoulder bursitis helps us take steps to avoid it. This way, we can lower our chances of getting this painful condition.
Proper Technique and Ergonomics
Using proper technique and having ergonomic workspaces are key. They help avoid injuries that might lead to bursitis. Here’s how:
- Keep the right posture during work and daily tasks.
- Make sure your work area is set up to avoid shoulder strain.
- Choose tools and equipment that don’t require too much repetition.
Strengthening and Flexibility Exercises
Doing strengthening exercises and flexibility routines helps prevent bursitis. Here are some good ones:
- Do shoulder rolls and blade squeezes to improve posture and reduce tension.
- Use resistance bands to strengthen the rotator cuff.
- Stretch regularly to keep your range of motion good.
Lifestyle Modifications
Changing our lifestyle can also help prevent shoulder bursitis. Here are some tips:
- Avoid doing the same overhead movements too much or take breaks when you must do them.
- Keep a healthy weight to lessen joint pressure.
- Stay active to keep your muscles and joints healthy.
By following these prevention tips, we can lower our risk of getting shoulder bursitis. This helps us keep our shoulders healthy and functional.
Potential Complications of Untreated Shoulder Bursitis
Shoulder bursitis left untreated can cause many problems. These issues can affect your daily life a lot. They can include chronic pain, disability, and even frozen shoulder.
Chronic Pain and Disability
Chronic pain is a big problem if shoulder bursitis is not treated. The inflammation and irritation can cause ongoing pain. This pain can make it hard to do daily tasks, sleep well, and enjoy life.
In severe cases, this pain can make you disabled. Simple tasks become very hard to do.
Key aspects of chronic pain and disability include:
- Persistent pain that lasts beyond the initial inflammation
- Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
- Increased risk of developing other musculoskeletal issues
Frozen Shoulder Development
Frozen shoulder, or adhesive capsulitis, is a condition where the shoulder is stiff and painful. If shoulder bursitis is not treated, it can lead to frozen shoulder. This is because the inflammation can cause scarring and tightening of the joint capsule.
The progression of frozen shoulder involves three stages:
- Freezing stage: Increasing pain and stiffness
- Frozen stage: Reduced range of motion
- Thawing stage: Gradual improvement in mobility
Impact on Quality of Life
Untreated shoulder bursitis can really affect your quality of life. Chronic pain and reduced mobility can harm your physical and mental health. This can lead to depression and anxiety.
It’s important to understand these complications. This shows why you should see a doctor for shoulder bursitis. Early treatment can prevent long-term problems and improve your health.
Recovery Timeline: What to Expect
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Acute Phase
The acute phase is the first part of recovery, lasting a few days to weeks. It focuses on reducing inflammation and pain. Rest, ice therapy, and anti-inflammatory meds are recommended to ease symptoms.
Rehabilitation Phase
After the acute phase, you move into the rehabilitation phase. This stage is vital for getting your shoulder back to normal. A physical therapy program is suggested, including exercises for flexibility and strength.
Return to Normal Activities
The final stage is about slowly getting back to your usual activities. It’s important to listen to your body and not rush back too fast. A slow return helps avoid re-injury and ensures a lasting recovery.
Here’s a quick overview of the recovery timeline for shoulder bursitis:
| Phase | Duration | Key Activities |
| Acute Phase | A few days to 2 weeks | Rest, ice therapy, anti-inflammatory medications |
| Rehabilitation Phase | 2-6 weeks | Physical therapy, flexibility and strengthening exercises |
| Return to Normal Activities | 6 weeks and beyond | Gradual return to activities, monitoring for re-injury |
Knowing the recovery timeline for shoulder bursitis prepares you for what’s ahead. By sticking to the recommended treatments and guidelines for each phase, you can successfully recover and get back to your normal activities with confidence.
Shoulder Bursitis vs. Other Shoulder Conditions
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Rotator Cuff Injuries
Rotator cuff injuries are a big reason for shoulder pain. They can look like bursitis at first glance. But, rotator cuff injuries damage the tendons or muscles around the shoulder. Bursitis, on the other hand, is about inflammation in the bursae.
Key differences:
- Location of pain: Rotator cuff injuries usually hurt the front and side of the shoulder. Bursitis can hurt in different spots, depending on the bursa.
- Nature of pain: Rotator cuff injuries might hurt when you move your shoulder in certain ways. Bursitis tends to cause more general pain and tenderness.
Tendinitis vs. Bursitis
Tendinitis and bursitis are both inflammatory issues, but they target different parts of the shoulder. Tendinitis is about the tendons getting inflamed. Bursitis is about the bursae getting inflamed.
| Characteristics | Tendinitis | Bursitis |
| Structures Affected | Tendons | Bursae |
| Common Causes | Overuse, repetitive strain | Repetitive motion, trauma, infection |
| Symptoms | Pain with movement, tenderness | Pain, swelling, limited mobility |
Arthritis and Bursitis Differences
Arthritis and bursitis are two different conditions that can show similar signs. Arthritis is about the joint itself getting inflamed. Bursitis is about the bursae around the joint getting inflamed.
Differential diagnosis:
- Arthritis usually causes joint pain and stiffness. Bursitis causes pain and swelling in the soft tissues around the joint.
- Arthritis often affects more than one joint. Bursitis usually sticks to one area.
When to See a Doctor for Shoulder Pain
Shoulder pain can come from many things, like small injuries or serious health issues. It’s hard to know when to see a doctor. But, there are important signs to look out for. Knowing these can help you get medical help early and avoid bigger problems.
Red Flag Symptoms
Some symptoms mean you need to see a doctor right away. These include:
- Sudden severe pain
- Pain with fever or swelling
- Numbness or tingling
- Weakness in the arm or shoulder
These signs can mean serious issues like infections, breaks, or nerve problems.
Persistent or Worsening Symptoms
If your shoulder pain doesn’t go away or gets worse, see a doctor. Long-lasting pain might mean problems like bursitis, tendinitis, or rotator cuff injuries.
Follow-up Care Guidelines
After you start treatment, getting follow-up care is key. It helps your healing and stops pain from coming back. You might need physical therapy, changes in your lifestyle, and regular visits to your doctor.
| Follow-up Activity | Frequency | Purpose |
| Physical Therapy | 2-3 times a week | Improve range of motion and strength |
| Lifestyle Modifications | Ongoing | Prevent recurrence and promote healing |
| Check-ups | Every 4-6 weeks | Monitor progress and adjust treatment |
Conclusion
Understanding the shoulder’s anatomy is crucial for accurate diagnosis and effective treatment of various conditions.
Managing shoulder bursitis involves medical treatment, physical therapy, and lifestyle changes. We’ve talked about the importance of proper diagnosis and the role of corticosteroid injections. Therapeutic exercises also play a big part in improving shoulder function and preventing future problems.
In summary, shoulder bursitis is treatable with a well-rounded approach. We hope this summary has given you useful insights. By using this knowledge, you can take care of your shoulder health and keep it functioning well.
FAQ
What is shoulder bursitis?
Shoulder bursitis is when the bursae in the shoulder joint get inflamed. This causes pain, stiffness, and makes it hard to move the arm.
What are the symptoms of shoulder bursitis?
Symptoms include pain or tenderness in the shoulder, swelling or redness, and trouble moving the arm.
What causes shoulder bursitis?
It can be caused by repetitive motion injuries, traumatic injuries, infections, or conditions like arthritis or gout.
How is shoulder bursitis diagnosed?
Doctors use a physical exam, medical history, and imaging tests like X-rays or MRI to diagnose it.
What are the treatment options for shoulder bursitis?
Treatment includes medication, corticosteroid injections, physical therapy, and sometimes surgery.
How can I manage shoulder bursitis at home?
Rest, ice and heat therapy, over-the-counter pain meds, and avoiding activities that make it worse can help.
Can shoulder bursitis be prevented?
Yes, by using proper technique, doing strengthening and flexibility exercises, and making lifestyle changes.
What are the possible complications of untreated shoulder bursitis?
Untreated bursitis can lead to chronic pain, disability, frozen shoulder, and a big impact on your quality of life.
How long does it take to recover from shoulder bursitis?
Recovery time depends on the severity and treatment. It involves an acute phase, rehabilitation, and getting back to normal activities.
When should I seek medical attention for shoulder pain?
See a doctor if you have red flag symptoms, symptoms get worse, or if you’re worried about your shoulder pain.
Can shoulder bursitis be confused with other shoulder conditions?
Yes, it can be confused with rotator cuff injuries, tendinitis, or arthritis. Proper diagnosis is key.
What is the role of physical therapy in treating shoulder bursitis?
Physical therapy is vital. It improves range of motion, strengthens muscles, and helps in recovery.
Are there any lifestyle changes that can help manage shoulder bursitis?
Yes, maintaining a healthy weight, avoiding repetitive strain, and improving posture can help manage it.
References
- Ferreira, M. L., et al. (2024). A systematic review of clinical practice guidelines on the management of common shoulder disorders. American Journal of Physical Medicine & Rehabilitation. Retrieved from https://pubmed.ncbi.nlm.nih.gov/37832814/