Every year, millions of people in the United States have orthopedic surgery. A big worry is the chance of complications. Surgical infection is a major and serious risk.
The biggest complication can make recovery longer, need more medical help, and cost more. It’s important for doctors and patients to know the main risks. This helps prevent and manage these problems well.
Key Takeaways
- Surgical infection is a major complication of orthopedic procedures.
- The risk of infection can lead to prolonged recovery and additional medical costs.
- Understanding the risks is key to effective management and prevention.
- Orthopedic surgery complications can have a big impact on patient outcomes.
- Prevention strategies are important to reduce the risk of complications.
The Landscape of Orthopedic Surgery in Modern Medicine
Modern orthopedic surgery includes many procedures, like joint replacements and spinal surgeries. It has grown a lot, thanks to new technology and a focus on patient care. The quick use of digital healthcare has changed how we engage with patients. This shows how tech is changing orthopedic care.
Common Types of Orthopedic Procedures
Orthopedic surgeries can be divided into several types. These include:
- Joint replacement surgeries, such as hip and knee replacements
- Orthopedic trauma surgeries, including fracture repairs
- Spinal surgeries, such as discectomies and spinal fusions
- Soft tissue surgeries, including tendon and ligament repairs
These surgeries help with many conditions, from osteoarthritis to injuries from sports or accidents. A study found, “Digital health technologies have improved patient results and cut down recovery times.” This shows how important modern healthcare is in orthopedic surgery.
General Risk Factors for Complications
While orthopedic surgery is mostly safe, some factors can raise the risk of problems. These include:
- Patient-related factors, such as age, obesity, and existing health issues
- Procedure-related factors, like the surgery’s complexity and the surgeon’s skill
Knowing these risk factors helps in finding ways to lower the chance of complications. As the field keeps growing, using digital healthcare is key to better patient care and results.
Surgical Site Infections: The Leading Orthopedic Surgery Complication
Surgical site infections in orthopedic surgery are a big problem. They make patients stay in the hospital longer and cost more. This is bad for everyone involved.
SSIs are a big worry in orthopedic surgery. They affect how well patients do and the cost of healthcare. Knowing how common they are helps us find ways to stop them.
Incidence and Statistics
SSIs happen in different ways in orthopedic surgery. The rate depends on the surgery, the patient, and the hospital. About 1% to 5% of surgeries get an SSI. But some surgeries, like spinal and joint replacements, have higher rates.
| Type of Orthopedic Surgery | Incidence of SSI |
| Spinal Surgery | 2.5% |
| Joint Replacement | 1.8% |
| Other Orthopedic Surgeries | 1.2% |
These numbers show we need to be careful about infections. We must focus on care before, during, and after surgery to lower SSI risks.
Types of Surgical Infections
SSIs are divided into two types: superficial and deep. Superficial infections are in the skin and just below. Deep infections go deeper, into muscle or bone.
Superficial Incisional Infections show as redness, swelling, and drainage. They are usually treated with antibiotics and wound care.
Deep Incisional Infections are more serious. They can affect implants. These need strong treatment, like removing the infected part.
Knowing the types of infections helps us treat them better. Early action can prevent worse problems. This improves patient care.
Understanding the Most Common Orthopedic Surgery Complications
It’s key to know the common problems after orthopedic surgery to improve care and results. These surgeries, like joint replacements and fracture fixes, each have their own risks.
Ranking Complications by Frequency
Complications in orthopedic surgery can be sorted by how often they happen. Surgical site infections are a big issue, affecting recovery and costs a lot.
| Complication Type | Frequency Rate |
| Surgical Site Infections | 2-5% |
| Nerve Injuries | 1-3% |
| Venous Thromboembolism | 1-2% |
Ranking Complications by Severity
Severity is as important as how often complications happen. Pulmonary embolism, for example, is rare but can be deadly.
- Pulmonary Embolism: High severity, low frequency
- Nerve Damage: Variable severity, moderate frequency
- Surgical Site Infections: Moderate severity, higher frequency
Variation Across Different Procedures
The kind of surgery greatly affects the risks and types of problems. For example, joint replacement surgeries face different challenges than arthroscopic procedures.
Knowing these differences helps doctors plan better care before, during, and after surgery to lower risks.
Venous Thromboembolism: A Life-Threatening Risk
Venous thromboembolism includes deep vein thrombosis and pulmonary embolism. It’s a big risk for those having orthopedic surgery. A blood clot in a vein can travel to the lungs, causing a pulmonary embolism.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is when a blood clot forms in deep veins, usually in the legs. Symptoms are swelling, pain, and redness in the leg. If not treated quickly, it can get worse.
Key symptoms of DVT:
- Swelling in the affected leg
- Pain or tenderness
- Redness or discoloration
- Warmth to the touch
Pulmonary Embolism
A pulmonary embolism happens when a blood clot travels to the lungs, blocking blood flow. It’s very serious and needs quick medical help. Symptoms include trouble breathing, chest pain, and coughing up blood.
Recognizing the signs of pulmonary embolism is key for quick action.
| Symptoms | Description |
| Difficulty Breathing | Shortness of breath or feeling winded even when sitting |
| Chest Pain | Pain or discomfort that gets worse with deep breathing or coughing |
| Coughing Up Blood | Coughing up blood or bloody mucus |
Risk Assessment for Blood Clots
Figuring out the risk of blood clots involves looking at several things. These include the surgery type, patient age, and how mobile they are. Knowing these risks helps in taking the right steps to prevent them.
Doctors use tools and guidelines to check the risk of venous thromboembolism in orthopedic surgery patients. This is important for picking the best way to prevent it.
Nerve Injuries and Neurological Complications
Orthopedic surgery carries a risk of nerve damage. This can happen for many reasons during surgery. It leads to serious neurological problems.
Nerve damage in orthopedic surgery can come from several causes. These include direct injury, compression, or stretching of nerves. Knowing these causes helps reduce risks.
Mechanisms of Nerve Damage
Nerve injuries in orthopedic surgery often result from:
- Direct trauma during the surgical procedure
- Compression or stretching of nerves due to positioning or retraction
- Ischemia or reduced blood flow to the nerves
A study found that nerve injury rates vary. This depends on the surgery type and patient factors.
“Careful preoperative planning and intraoperative techniques can significantly reduce the risk of nerve damage.”
Common Nerve Injuries by Procedure Type
Different orthopedic procedures have different nerve injury risks. For example:
- Total hip arthroplasty is associated with a risk of femoral nerve injury
- Spine surgery can result in nerve root injuries or cauda equina syndrome
Knowing the specific risks of each procedure is key for making informed choices.
Long-term Implications of Nerve Damage
Nerve injuries can have lasting effects. These include chronic pain, numbness, and limited function. The impact on quality of life is significant.
Early detection and proper management of nerve injuries are vital for the best outcomes.
Implant and Hardware Failures in Orthopedic Procedures
In orthopedic surgery, implant or hardware failure is a big problem. It can make recovery longer and might need more surgeries. These failures can change how well the surgery works and affect the patient’s life.
Prosthesis Loosening
Prosthesis loosening happens when the artificial joint or implant comes loose from the bone. It can be caused by bad placement, weak bones, or too much wear. Prosthesis loosening often means another surgery is needed to fix it and get the joint working right again.
Mechanical Failures
Mechanical failures happen when parts like screws, plates, or rods break or don’t work right. This can be because of a flaw in making them, wrong use, or too much stress. Mechanical failures can cause a lot of problems, like pain, infection, and needing more surgery.
Material Degradation Issues
Material degradation is when the materials in implants or hardware get worse over time. This can be because of rust, wear, or getting tired. Material degradation can cause implant failure, which might need more medical help.
The effects of implant and hardware failures are serious. It shows how important it is to choose the right patient, do the surgery carefully, and take good care after. Knowing about these problems helps doctors and patients set better goals and get better results.
Bone Healing Complications After Surgery
After orthopedic surgery, the bone healing process can face several challenges. This process involves many cellular and molecular steps. If these steps are disrupted, it can make recovery harder.
Delayed Union
A delayed union happens when bone healing takes longer than expected. This can be caused by poor blood supply, infection, or unstable fracture sites. It can extend recovery times and increase the risk of more problems.
Nonunion
Nonunion is when the bone doesn’t heal at all. It can be caused by severe trauma, infection, or bone fragments not aligning right. Nonunion often needs more surgery to help the bone heal.
Malunion
Malunion occurs when the bone heals in the wrong position. This can cause deformity or make it hard to move. It might need surgery to fix the bone’s alignment and function.
It’s important for both doctors and patients to know about these bone healing issues. By understanding the risks and taking steps to prevent them, we can improve surgery outcomes.
Joint-Specific Orthopedic Surgery Complications
Orthopedic surgery can face challenges specific to each joint. These challenges affect how well a patient recovers and how long it takes. Each joint has its own unique anatomy and function, making some surgeries riskier than others.
Knee Replacement Complications
Knee replacement surgery is often successful but can have complications. These include:
- Infection: Infection is a risk with any surgery, but it’s more common with knee replacements.
- Implant Loosening: The implant can loosen over time, causing pain and needing more surgery.
- Instability: The knee might feel unstable, making everyday activities hard.
Hip Replacement Complications
Hip replacement surgery also has its own set of risks.
- Dislocation: The new hip joint can dislocate, which is common in the first few months after surgery.
- Fracture: Fractures can happen during or after surgery, more so in older patients with weak bones.
- Wear and Tear: Over time, the artificial parts can wear out, needing more surgery.
Shoulder Surgery Complications
Shoulder surgery includes many procedures, like rotator cuff repairs and replacements. Complications can include:
- Nerve Damage: Nerves near the surgery site can be damaged.
- Infection: Infection is a risk, like with other surgeries.
- Stiffness: Stiffness after surgery is common but can be treated with physical therapy.
Spine Surgery Complications
Spine surgery, for conditions like degeneration or deformities, has its own risks.
- Nerve Injury: Spinal surgery can harm nearby nerves.
- Infection: Infection is a risk, more so in complex surgeries with instruments.
- Hardware Failure: Hardware like rods and screws can fail over time.
It’s important for orthopedic surgeons to know these complications. This knowledge helps them reduce risks and improve patient results. By understanding the risks of each surgery, doctors can better manage patient expectations and find ways to lessen these risks.
Post-Operative Pain Management Challenges
Managing pain after orthopedic surgery is tough for patients and doctors. It’s key to keep patients comfortable, help them recover, and avoid complications.
Acute Post-Operative Pain
Acute pain is common after orthopedic surgery. It’s sharp and intense, happening right after the surgery. Managing this pain well is key to avoid chronic pain.
- Using many types of pain relief
- Reducing opioid use
- Trying regional anesthesia
Chronic Pain Development
Chronic pain is a big worry after surgery. It happens when acute pain isn’t managed well, lasting longer than healing time.
Things that can lead to chronic pain include:
- Nerve damage during surgery
- Poor pain management
- Existing pain conditions
Pain Management Strategies
Good pain management is essential for both acute and chronic pain. Strategies include:
- Medicine like NSAIDs and opioids
- Non-medical methods like physical therapy
- Interventional steps like nerve blocks
With a comprehensive pain management plan, doctors can better patient outcomes. This reduces chronic pain risk and boosts care satisfaction.
Risk Factors That Increase Orthopedic Surgery Complications
Knowing the risk factors is important to lower the chance of problems in orthopedic surgery. Many things can affect the risk of complications. It’s key for doctors and patients to understand these.
Patient-Related Factors
Factors related to the patient are big in deciding the risk of problems. These include:
- Age: Older patients might face a higher risk because of less physical strength and health issues.
- Comorbidities: Conditions like diabetes, heart disease, and obesity can make surgery and recovery harder.
- Lifestyle Factors: Smoking and drinking too much alcohol can slow healing and raise the risk of issues.
Procedure-Related Factors
The type and how complex the orthopedic procedure is also affects the risk of problems. Consider these factors:
- Complexity of the Procedure: More complex surgeries might have a higher risk of complications.
- Surgical Technique: The surgeon’s skill and the method used can change the outcome.
- Implant or Hardware Use: Using implants or hardware can add risks, like implant failure or reaction to materials.
Understanding these risk factors helps healthcare providers manage patient expectations and outcomes. This can lower the number of complications.
Modern Approaches to Preventing Orthopedic Surgery Complications
Modern orthopedic surgery uses a variety of methods to avoid complications. It combines the latest technology and proven practices. This approach covers everything from before surgery to aftercare.
Preoperative Preparation
Getting ready for surgery is key to avoiding problems. Doctors check patients thoroughly and help them manage health issues. They also teach patients about what to do after surgery.
For example, people with diabetes are told how to control their blood sugar. Smoking cessation advice is given to help wounds heal better and improve surgery results.
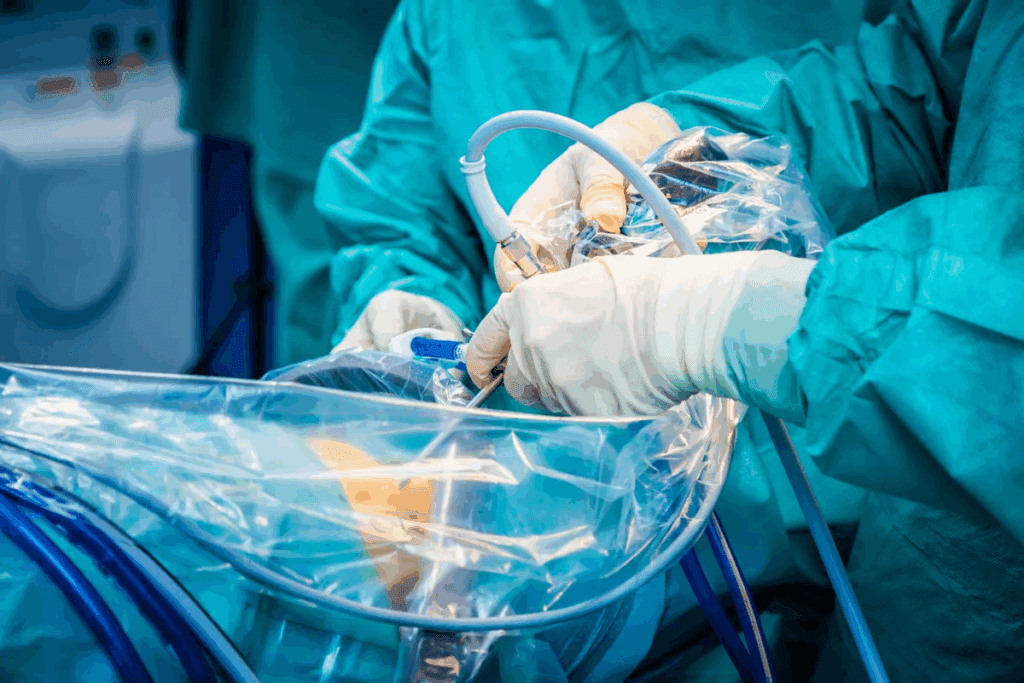
Intraoperative Precautions
During surgery, careful steps are taken to prevent issues. Surgeons use precise techniques and the latest tools. They also follow strict rules to avoid infections.
Using antibiotic prophylaxis is common to lower infection risks. Enhanced recovery after surgery (ERAS) protocols also help reduce complications and improve results.
Postoperative Care Protocols
After surgery, care is just as important. Standard plans for pain, blood clot prevention, and early movement are key. These plans help prevent complications.
- Watching for signs of infection or other issues
- Starting rehabilitation programs based on the patient’s needs
- Ensuring patients take their medicines as directed
Technological Advances in Prevention
New technologies have greatly helped prevent surgery problems. Digital health tools like artificial intelligence (AI) and machine learning (ML) offer personalized care and predict risks.
| Technological Advance | Description | Benefit |
| AI and ML | Predictive analytics for complication risk | Personalized patient care |
| 3D Printing | Custom implants and surgical guides | Improved surgical precision |
| Robotic Surgery | Enhanced surgical accuracy and control | Reduced risk of complications |
Using these technologies in surgery is a big step forward. It helps prevent problems and improves patient results. As shown in the KPJ Healthcare Berhad Integrated Annual Report 2024, digital health solutions are key to better surgery care.
Effective Management of Complications When They Occur
Managing complications well is key to good results in orthopedic surgery. A solid plan for handling issues can greatly improve recovery and success.
Early Detection Strategies
Finding complications early is essential for quick action. This includes regular check-ups after surgery, watching for infection signs, and using new diagnostic tools.
A study shows, “Finding and treating complications early can greatly lower risks in orthopedic patients.” Keeping a close eye on patients helps catch problems before they get worse.
Treatment Approaches
How to treat complications depends on the problem. For infections, doctors use antibiotics and care for the wound. If implants fail, surgery to fix them might be needed.
- Antibiotic therapy for infections
- Revision surgery for implant or hardware failure
- Physical therapy to address mobility issues
Revision Surgery Considerations
Revision surgery is a big deal when the first surgery doesn’t work out. Decisions are based on the patient’s health, the complication, and the benefits and risks of surgery.
Key considerations for revision surgery include:
- Assessing the cause of the initial complication
- Evaluating the patient’s suitability for further surgery
- Planning the revision surgery to address specific issues
By taking a detailed approach to managing complications, doctors can make patients’ outcomes better and lower the chance of more problems.
The Patient’s Role in Minimizing Orthopedic Surgery Complications
Orthopedic surgery success relies on the team and the patient’s actions. Surgeons and healthcare professionals do a lot, but patients play a big role too. They can greatly affect their healing and the chance of problems.
Following Medication Protocols
Following medication protocols is key after surgery. Patients take medicines to manage pain, prevent infection, and stop blood clots. It’s important to take these medicines exactly as told by the doctor. Missing doses or taking the wrong amount can cause problems.
Patients should also watch for side effects and how medicines interact. Keeping a list of all medicines, including how much and how often, helps doctors make better decisions.
Adhering to Activity Restrictions
After surgery, patients have activity limits to help healing and avoid damage. Following these limits is very important for a good recovery. This means avoiding heavy lifting, bending, or hard activities for a while.
It’s also important to listen to your body and not ignore pain or discomfort. Going back to normal activities slowly, with doctor’s advice, helps avoid complications.
Attending Follow-up Appointments
Follow-up appointments are essential for checking on healing and addressing any issues. Patients should keep all appointments and talk to their healthcare team about any problems or questions.
These visits are also when patients learn about rehabilitation exercises and physical therapy. These are important for getting strength and mobility back after surgery.
Recognizing Warning Signs
Knowing warning signs of complications is a big responsibility for patients. This includes signs like more pain, swelling, redness, or warmth at the surgery site, or fever or chills.
Patients should know who to call and when to get emergency help if they notice anything unusual. Quick action can make a big difference in treatment success and outcome.
Conclusion: Navigating the Risks of Orthopedic Surgery
It’s important to know the possible problems with orthopedic surgery. This knowledge helps both patients and doctors. By understanding risks like infections, blood clots, and nerve damage, we can prevent and manage them better.
To handle these risks, we need a full plan. This includes getting ready for surgery, being careful during it, and caring for the patient after. These steps help lower the chance of problems, making recovery better.
Managing surgery complications starts with quick action. Patients must follow their treatment plans, rest when needed, and go to check-ups. Working together, doctors and patients can overcome surgery risks and get good results.
FAQ
What are the most common complications of orthopedic surgery?
Common issues after orthopedic surgery include infections at the surgical site and blood clots. Nerve damage, problems with implants, and issues with bone healing are also common. These can include delayed healing, nonunion, and malunion.
How can surgical site infections be prevented in orthopedic surgery?
To prevent infections, start with pre-surgery steps. This includes antibiotics and cleaning the skin. Keeping the surgery area clean is key.
After surgery, proper wound care and watching for infection signs are important.
What is venous thromboembolism, and how is it related to orthopedic surgery?
Venous thromboembolism is when blood clots form in deep veins. These clots can travel to the lungs, causing a serious condition. Orthopedic surgery, like knee or hip procedures, increases this risk due to the body being immobile for a long time.
What are the risks associated with nerve injuries during orthopedic surgery?
Nerve injuries can cause numbness, weakness, or even paralysis. The risk depends on the surgery type and the nerves involved.
How can patients minimize the risk of complications after orthopedic surgery?
To lower risks, follow your doctor’s medication and activity advice. Attend all follow-up appointments and watch for any signs of trouble.
What are the signs of complications after orthopedic surgery that patients should watch out for?
Look out for increased pain, swelling, redness, or warmth at the surgery site. Fever, numbness, and trouble moving the affected area are also warning signs. Be aware of leg pain or swelling, which could be a sign of blood clots.
How are bone healing complications managed in orthopedic surgery?
To manage bone healing issues, doctors may use revision surgery or bone grafting. Orthobiologics can also help speed up healing.
What are the challenges of post-operative pain management in orthopedic surgery?
Managing pain after surgery is tough because of the complex nature of pain. It’s important to find effective pain relief without the risks of addiction or side effects. Doctors use various methods, including different types of pain medication and non-drug treatments.
How do implant and hardware failures occur in orthopedic surgery?
Implant failures can happen due to loosening, mechanical issues, or wear and tear. These problems might require another surgery to fix.
What are the unique risks associated with different types of joint surgeries?
Each joint surgery, like knee or hip replacements, has its own risks. For example, knee replacements can have issues with the prosthesis loosening. Shoulder or spine surgeries might risk nerve damage.
How can technological advancements help prevent orthopedic surgery complications?
New technologies, like computer-assisted surgery, can make procedures more precise. They can also reduce blood loss and improve how implants fit and function.
What is the role of patient-related factors in orthopedic surgery complications?
Factors like age, health conditions, and lifestyle can increase the risk of complications. Understanding these can help doctors prevent and manage issues better.
How can early detection and treatment improve outcomes in orthopedic surgery complications?
Catching and treating complications early can greatly improve results. It helps reduce the severity of problems and prevents long-term damage. Monitoring closely and acting quickly when needed is key.
Reference
- Florescu, S. C., et al. (2013). Venous thromboembolism following major orthopedic surgery. Journal of Medicine & Life, 6(3), 273-277. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3865129/