Nearly 1 in 5 patients face complications after orthopedic surgery, studies show. This surgery, though sometimes needed, comes with big risks. These risks can affect how well you recover and your overall health.
Complications can range from infection and nerve damage to prolonged recovery times and limited mobility post-surgery. It’s key for patients to know these risks. This helps them make better choices about their treatment.
If you’re thinking about orthopedic surgery, know the risks. Understanding these can help you get ready for the challenges of recovery.
Key Takeaways
- Orthopedic surgery carries significant risks, including infection and nerve damage.
- Complications can lead to prolonged recovery times and limited mobility.
- Understanding the risks is key for making informed decisions.
- Patients should be aware of the possible complications.
- Being prepared can help you through the recovery process.
The Major Cons of Orthopedic Surgery Explained
It’s important for patients to know the downsides of orthopedic surgery before deciding. These surgeries treat many musculoskeletal problems. But, they come with risks.
“The complexity of orthopedic surgery demands a thorough understanding of possible complications,” a study says. It points out how important it is to place implants correctly. This helps avoid needing more surgeries because of dislocation.
Why Understanding Surgical Risks Matters
Orthopedic surgeries, like any big surgery, have risks that can affect recovery. Problems like infection, nerve damage, and surgery not working are big worries. Knowing these risks helps to lessen them.
Recent data shows that putting implants in the right place is key. Using navigation systems helps make this more accurate. This shows how important new surgical methods are in avoiding problems.
Balancing Benefits Against Possible Drawbacks
When thinking about orthopedic surgery, weighing the good against the bad is key. Surgery can help with chronic pain and improve movement. But, it’s important to know about possible recovery issues and long-term problems.
Infection after surgery is a big problem. It can make recovery take longer and even lead to surgery not working. Knowing these risks helps patients make better choices and get ready for what might happen.
By looking at the downsides of orthopedic surgery, people can make smarter choices. They can work with their doctors to get the best results.
General Anesthesia Risks in Orthopedic Procedures
General anesthesia is key in many orthopedic surgeries. But, it also has risks and complications. Knowing these risks helps patients make better choices about their surgery.
Common Anesthesia Complications
General anesthesia can cause several problems, from mild to severe. Some common issues include:
- Respiratory problems, such as trouble breathing or pneumonia
- Cardiovascular issues, like changes in heart rate or blood pressure
- Nausea and vomiting
- Sore throat or damage to the vocal cords
- Malignant hyperthermia, a rare but serious condition
Factors That Increase Anesthesia Risk
Some factors can make anesthesia risks higher in orthopedic procedures. These include:
| Risk Factor | Description |
| Age | Older adults face higher risks due to less physical strength. |
| Pre-existing Medical Conditions | Conditions like heart disease, diabetes, or lung disease raise risks. |
| Smoking | Smoking can cause respiratory problems. |
| Obesity | Obesity increases risks of respiratory and cardiovascular problems. |
Long-Term Effects of General Anesthesia
General anesthesia is usually safe, but there can be long-term effects. Some patients might experience:
- Cognitive dysfunction, like memory issues or trouble concentrating
- Prolonged recovery time
- In rare cases, long-term neurological effects
It’s vital for patients to talk about their risks and concerns with their healthcare provider before surgery.
Infection: A Serious Post-Surgical Complication
Infection is a major problem after orthopedic surgery. It can affect the patient’s recovery and the success of the surgery. Infections can take many forms and have serious effects.
Surgical Site Infections
Surgical site infections (SSIs) are a big worry in orthopedic surgery. These infections happen at the surgery site and can be skin infections or deeper. SSIs can cause longer hospital stays, more surgeries, and higher costs.
Risk factors for SSIs include:
- Prolonged surgical time
- Presence of other infections at the time of surgery
- Poor wound care
- Diabetes and other comorbidities
Deep Tissue and Bone Infections
Deep tissue and bone infections are serious and hard to treat. These infections can affect the bone or the tissue around it. Treatment often means long antibiotic use and sometimes more surgery.
The consequences of deep tissue and bone infections can be severe, including:
- Chronic pain
- Reduced mobility
- Potential need for amputation in extreme cases
Implant-Associated Infections
Implant-associated infections happen when bacteria grow on implants like joint replacements. These infections are hard to treat because bacteria can stick to the implant, making antibiotics less effective.
The Pandit Deendayal Upadhyaya National Institute for Persons with Physical Disabilities offers important rehabilitation services. They help manage infections and other complications in patients with physical disabilities. This shows how important it is to have complete care after orthopedic surgery.
| Type of Infection | Description | Common Treatments |
| Surgical Site Infections | Infections occurring at the surgical site, ranging from superficial to deep tissue | Antibiotics, wound care, possible additional surgery |
| Deep Tissue and Bone Infections | Infections involving deep tissue or bone, such as osteomyelitis | Prolonged antibiotic therapy, possible surgery to remove infected tissue or hardware |
| Implant-Associated Infections | Infections associated with implanted devices, challenging to treat due to biofilm formation | Antibiotics, possible revision surgery to remove or replace the implant |
Blood Clots and Circulatory Complications
Blood clots are a big worry after orthopedic surgery. These clots can form in deep veins, known as deep vein thrombosis (DVT). If they break loose and go to the lungs, it’s a serious problem called pulmonary embolism.
Deep Vein Thrombosis Risk Factors
Many things can raise the risk of DVT after surgery. These include being immobile for a long time, the surgery type, age, obesity, and a history of blood clots. Knowing these risks helps in taking the right steps to prevent them.
Being immobile is a big factor in blood clot formation. When patients don’t move much after surgery, blood can pool in their legs. This increases the chance of clots. So, moving early and using blood thinners are often advised.
Pulmonary Embolism Dangers
A pulmonary embolism happens when a blood clot travels to the lungs. It blocks an artery and can be deadly. Symptoms include sudden breathlessness, chest pain, and coughing up blood. This shows how important it is to stop DVT before it happens.
Quick diagnosis and treatment are key for pulmonary embolism. Treatment usually involves blood thinners to stop more clots. In severe cases, doctors might need to remove the clot.
Preventive Measures and Their Own Risks
Stopping blood clots is a top goal for patients having orthopedic surgery. Doctors use blood thinners, compression devices, and get patients moving early. But, these steps have risks too.
For example, blood thinners can cause bleeding, which is a big problem for surgery patients. Compression devices are safer but might not work for everyone. So, finding the right balance for each patient is important.
Nerve Damage and Neurological Complications
Orthopedic surgery can fix many musculoskeletal problems but also has risks. These include nerve damage and neurological issues. Nerve injuries can happen for many reasons, like the surgery method, the patient’s body, and how complex the surgery is.
Types of Nerve Injuries During Surgery
Nerve injuries can be mild or severe. Neuropraxia is a mild form where nerve function is just temporarily disrupted. More serious injuries include axonotmesis, where the nerve’s axons are damaged, and neurotmesis, where the nerve is completely cut.
- Compression injuries happen when nerves get squished during surgery or by swelling after it.
- Transection injuries occur when nerves are cut or severed during the procedure.
- Ischemic injuries happen when nerves don’t get enough blood flow.
Symptoms of Nerve Damage
Symptoms of nerve damage vary based on the injury’s type and severity. Common signs include:
| Symptom | Description |
| Numbness | A reduction or loss of sensation in the affected area. |
| Weakness | Muscle weakness or paralysis in the area supplied by the damaged nerve. |
| Pain | Sharp, burning, or stabbing pain, often described as neuropathic pain. |
| Tingling | A pins-and-needles sensation, often accompanied by numbness. |
A medical expert notes, “Nerve damage during orthopedic surgery can significantly affect a patient’s recovery and long-term outcome.”
“The risk of nerve injury is a critical consideration in orthopedic surgery, necessitating careful preoperative planning and intraoperative techniques to minimize this risk.”
Permanent vs. Temporary Neurological Effects
Nerve damage can be either temporary or permanent. It depends on the injury’s extent and the body’s recovery ability. Sometimes, nerves can heal, leading to full or partial recovery. But, severe injuries might cause permanent neurological problems.
It’s important for patients and healthcare providers to understand the risks and outcomes of nerve damage in orthopedic surgery. Being informed helps patients make better choices, and providers can work to reduce these risks.
Post-Surgical Pain Management Challenges
Managing pain after orthopedic surgery is a big challenge for patients. It’s key for a smooth recovery. Good pain management affects how well a patient can get back to normal life.
Acute Post-Operative Pain
Right after surgery, patients face acute pain. This pain is the body’s way of reacting to the surgery. Managing this pain well is important to avoid bigger problems. Doctors often use pain meds like opioids or NSAIDs to help.
Development of Chronic Pain Syndromes
Sometimes, acute pain can turn into chronic pain. Chronic pain lasts longer than expected and can really affect a person’s life. Things like how severe the surgery was, any pain issues before, and genetics play a role.
Managing chronic pain needs a team effort. This includes medicine, physical therapy, and sometimes mental health support. Knowing the risks and acting early can help prevent chronic pain.
Opioid Dependency Risks
Using opioids for pain can lead to dependency. This is a serious issue that can harm health for a long time. The risk is higher for those who have used drugs before or take a lot of opioids for a long time.
| Risk Factors for Opioid Dependency | Description |
| History of Substance Abuse | Patients with a history of substance abuse are at higher risk of developing opioid dependency. |
| High Dose or Prolonged Use | Higher doses or longer durations of opioid use increase the risk of dependency. |
| Genetic Predisposition | Some individuals may be more susceptible to opioid dependency due to genetic factors. |
To lower these risks, doctors are looking at new ways to manage pain. They’re using non-opioid meds and special recovery plans. These methods aim to cut down on opioid use while keeping pain under control.
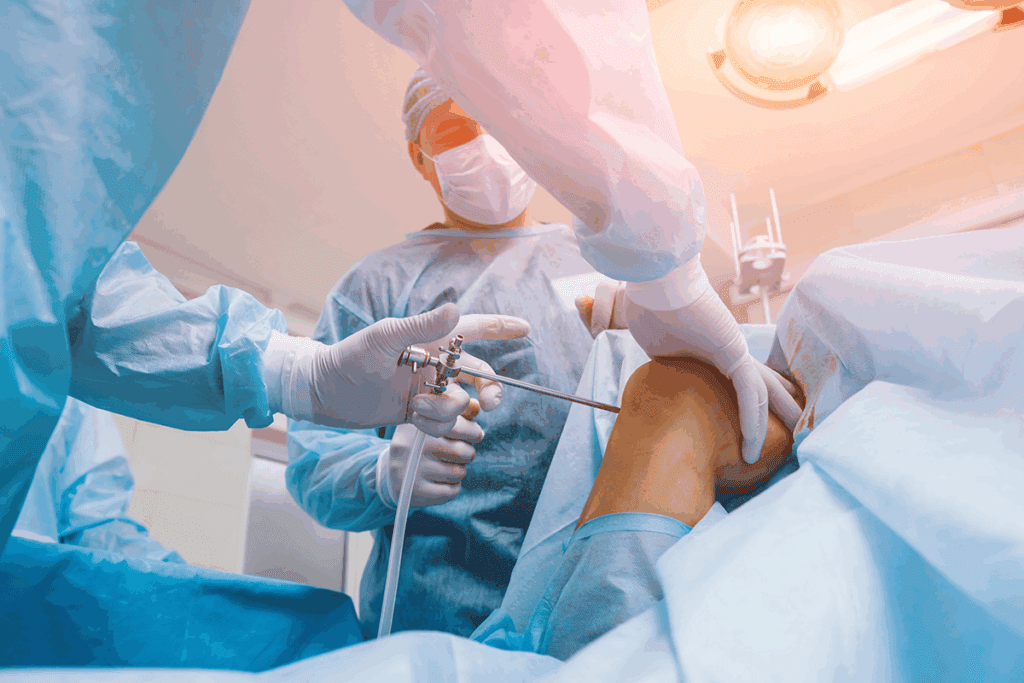
Extended Recovery and Rehabilitation Period
Orthopedic surgery often needs a long recovery time. This can be tough for patients. The length and effort of rehab depend on the surgery type.
Typical Recovery Timelines for Different Procedures
Recovery times differ for various surgeries. Joint replacements usually need 6 to 12 weeks to start feeling better. But, spinal fusions might take 3 to 6 months or more to fully recover.
| Surgical Procedure | Typical Recovery Time | Physical Therapy Requirements |
| Joint Replacement | 6-12 weeks | Moderate to High |
| Spinal Fusion | 3-6 months | High |
| Arthroscopic Surgery | 2-6 weeks | Low to Moderate |
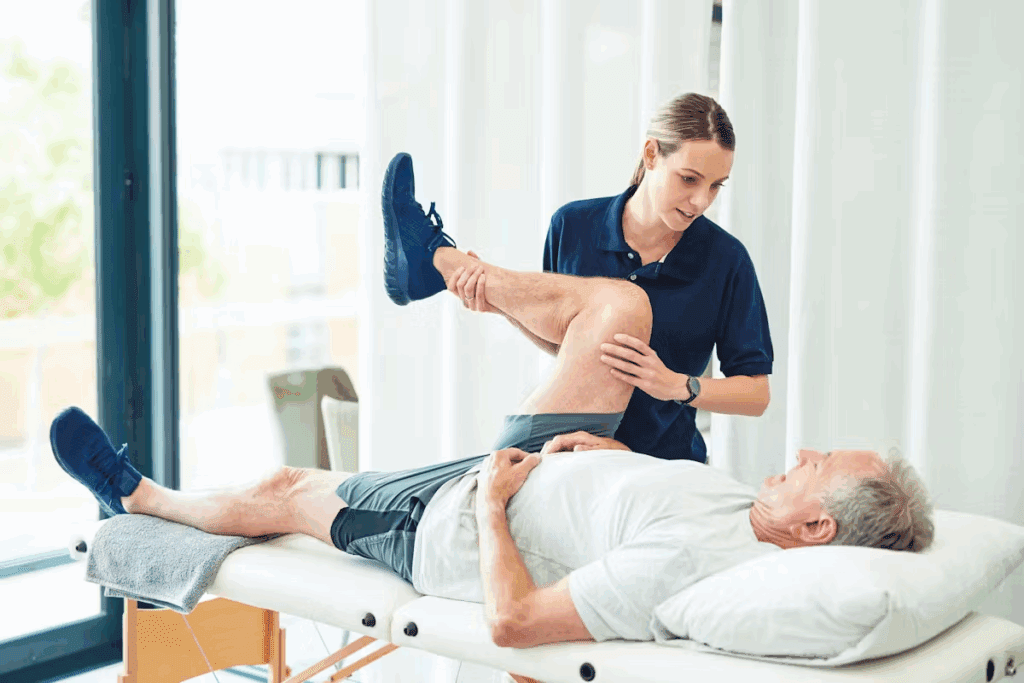
Physical Therapy Requirements
Physical therapy is key in rehab after orthopedic surgery. The amount and intensity of therapy depend on the surgery and patient’s health. Places like the Pandit Deendayal Upadhyaya National Institute for Persons with Physical Disabilities offer help with physiotherapy and occupational therapy.
Challenges in Returning to Normal Activities
Getting back to normal after surgery is hard. Patients struggle to regain strength, flexibility, and movement. Following a detailed rehab plan is vital for success.
Rehab programs made for each patient can greatly help in recovery. It’s also key for patients to know the long-term benefits of finishing their rehab as advised.
Limited Mobility and Functional Restrictions
Orthopedic surgery can sometimes lead to limited mobility and functional restrictions. These issues can affect a patient’s quality of life. The impact varies based on the surgery type and the patient’s health.
Temporary vs. Permanent Limitations
How much mobility is limited can depend on if it’s temporary or permanent. Temporary limitations are common in the early recovery phase. Patients may need to avoid certain activities to heal properly. Sometimes, though, limitations can be permanent, requiring lifestyle and daily routine changes.
- Temporary limitations often resolve with physical therapy and rehabilitation.
- Permanent limitations may necessitate long-term adjustments in daily activities.
Impact on Daily Activities
Limited mobility and functional restrictions can make daily activities hard. Simple tasks like bathing, dressing, or cooking can become challenging. Patients might need help from caregivers or family members, affecting their independence.
- Difficulty with personal care routines.
- Challenges in managing household chores.
- Limitations in participating in recreational or social activities.
Adaptive Equipment Needs
To overcome mobility challenges, patients often need adaptive equipment. This includes walkers, canes, wheelchairs, or tools for daily living. The need for such equipment can be short-term or long-term, based on surgery extent and recovery.
Examples of adaptive equipment include:
- Grabbers or reachers to pick up items without bending or stretching.
- Bathroom safety equipment, such as shower chairs or grab bars.
- Modified utensils for easier eating and cooking.
Understanding the possibility of limited mobility and functional restrictions helps patients prepare for surgery challenges. They can plan for adaptive equipment needs and arrange support during recovery.
Implant Failure and Hardware Complications
Implant failure is a risk in orthopedic surgery, even with modern advancements. Implants help fix joints and bones, easing pain and improving function. It’s important for patients to know about these risks.
Mechanical Failure of Implants
Implants can fail due to many reasons. These include wrong size, bad placement, or too much stress. A study shows how key accurate placement is to avoid failure.
When implants fail, it often means more surgery is needed. This can make recovery longer and riskier.
Material Wear and Degradation
Over time, implants can wear down. This happens because of friction, corrosion, or fatigue. The materials, like metals, ceramics, and plastics, can break down.
| Material | Common Issues | Potential Consequences |
| Metal | Corrosion, wear | Metal ion release, implant loosening |
| Ceramic | Fracture, wear | Implant failure, inflammation |
| Plastic (Polyethylene) | Wear, deformation | Osteolysis, implant loosening |
Foreign Body Reactions and Allergies
Some people react to the materials in implants. These reactions can be mild or severe. They might need the implant removed.
Key factors influencing foreign body reactions include:
- Material composition of the implant
- Presence of coatings or surface treatments
- Individual patient sensitivity
It’s vital for doctors and patients to understand these risks. This helps make better choices about using implants in surgery.
Psychological and Emotional Impact
Orthopedic surgery is not just about the body; it also affects the mind. Patients often feel a mix of emotions during and after surgery. These feelings can impact their recovery and overall happiness.
Depression and Anxiety During Recovery
Recovering from orthopedic surgery can feel long and lonely, leading to depression and anxiety. The change in daily life, along with the pain, can really affect a person’s mental health. It’s key for doctors to notice these signs and offer help.
The Pandit Deendayal Upadhyaya National Institute for Persons with Physical Disabilities found that counseling helps a lot. It improves patients’ emotional and mental health, making the recovery easier.
Body Image and Self-Perception Changes
Orthopedic surgery can change how patients see themselves. Scars, mobility issues, or hardware can make it hard to feel good about one’s body. It’s tough, but with the right mindset, patients can adjust.
Coping with Temporary Dependency
After surgery, many patients need help with everyday tasks. This can be hard for those who value being independent. To deal with this, setting realistic goals and using support systems is helpful.
| Psychological Aspect | Impact on Patients | Support Measures |
| Depression and Anxiety | Feelings of isolation, sadness, and worry | Psychological counseling, support groups |
| Body Image Changes | Self-consciousness about scarring or hardware | Counseling, support groups, preparation |
| Temporary Dependency | Frustration, loss of independence | Family support, home care services, realistic expectations |
It’s important to understand the emotional and mental effects of orthopedic surgery. By recognizing these and providing support, doctors can help patients recover better.
Specific Cons of Joint Replacement Surgery
Joint replacement surgery has its downsides. It aims to ease pain and improve joint function but comes with risks. Patients need to know about these complications.
Dislocation Risks in Hip Replacements
Hip replacement surgery carries a risk of dislocation. This can happen for several reasons. These include the wrong implant placement, weak muscles, or certain movements.
To lower this risk, doctors suggest certain precautions and exercises. These help strengthen the muscles around the joint. Yet, dislocation can happen and might need more surgery to fix.
Loosening of Components Over Time
Another issue with joint replacement is the loosening of parts over time. This can cause pain and reduce how well the joint works. It happens due to wear and tear, a bad fit, or bone loss around the implant.
In some cases, this problem needs a second surgery to fix. This is to keep the joint working properly.
Limited Lifespan of Prosthetic Joints
Prosthetic joints don’t last forever. A hip replacement usually lasts 15 to 20 years. But, this can change based on the patient’s age, how active they are, and the type of prosthesis.
| Prosthesis Type | Average Lifespan | Factors Affecting Lifespan |
| Hip Replacement | 15-20 years | Activity level, age, prosthesis material |
| Knee Replacement | 15-25 years | Weight, activity level, alignment |
Knowing this helps set realistic expectations. It’s important for making the right choice about joint replacement surgery.
Spine Surgery Complications and Drawbacks
It’s important for patients to know the risks of spine surgery. This surgery can help with many spinal problems. But, it also has possible complications that can affect the outcome.
Failed Back Surgery Syndrome
Failed Back Surgery Syndrome (FBSS) is a big problem after spine surgery. It means pain that doesn’t go away or comes back. This can happen for many reasons, like not choosing the right patient or not fully fixing the problem.
Experts say managing FBSS needs a team effort. They point out several reasons for it:
- Inadequate preoperative diagnosis
- Incomplete surgical decompression
- Postoperative instability
- Scar tissue formation
Adjacent Segment Disease
Adjacent Segment Disease (ASD) is another issue after spine surgery, often after fusions. It’s when the segments next to the fused area start to wear out. This can cause new pain or problems with nerves.
Several things can make ASD more likely:
- The number of levels fused
- The rigidity of the fusion construct
- Pre-existing degeneration at adjacent levels
Spinal Cord and Nerve Root Injuries
Spinal cord and nerve root injuries are serious risks of spine surgery. These injuries can happen from direct damage, compression, or lack of blood flow. The effects can be mild or very severe.
“The risk of neurological injury is a critical consideration in spine surgery, requiring meticulous surgical technique and careful patient monitoring,” according to a leading neurosurgeon.
Knowing these risks helps patients make better choices. While spine surgery can help many, understanding the possible problems helps prepare and set realistic expectations.
Surgical Failure and Unsatisfactory Outcomes
Thinking about orthopedic surgery? It’s important to know about the risk of surgical failure. These surgeries aim to ease pain and improve function. But sometimes, they don’t meet what patients hope for.
Incomplete Resolution of Symptoms
One big letdown is when symptoms don’t fully go away after surgery. Patients might keep feeling pain or have trouble moving. This can really affect their daily life.
Why doesn’t the surgery work for everyone? It could be because the problem is complex, there are other health issues, or unexpected problems happen during or after the surgery.
Recurrence of Original Condition
Another worry is when the problem comes back. For example, herniated discs or torn ligaments might not stay fixed. This can happen if the root cause isn’t fully treated or if it comes back after surgery.
When this happens, patients might need more surgery. This can be tough both physically and emotionally.
Need for Revision Procedures
At times, the first surgery doesn’t work as planned, or complications arise. This might mean needing a second surgery. These follow-up surgeries are usually more complicated and riskier.
Before deciding on orthopedic surgery, it’s key to understand these possible outcomes. Talk to your doctor about your specific risks and what you can expect. This way, you can make a well-informed choice about your treatment.
Long-Term Side Effects of Orthopedic Surgery
Orthopedic surgery aims to ease pain and improve function. Yet, it can also lead to long-term side effects. It’s important for patients to know about these complications to make informed choices.
Arthritis Development in Adjacent Joints
One major side effect is arthritis in joints near the surgery site. This happens because the surgery can change how these areas move. This extra stress can harm nearby joints.
A study in a Journal showed knee replacement surgery can lead to hip arthritis. This shows the need to think about how surgery affects all joints in the long run.
| Joint Affected | Incidence of Arthritis | Average Time to Onset |
| Knee | 30% | 5 years |
| Hip | 25% | 7 years |
| Shoulder | 20% | 10 years |
Scar Tissue Formation and Adhesions
Scar tissue is a common side effect of orthopedic surgery. While some scarring is normal, too much can cause pain and limit movement.
“The formation of scar tissue and adhesions can significantly impact a patient’s recovery trajectory, sometimes necessitating additional interventions,” notes an orthopedic surgeon.
Physical therapy is often used to manage scar tissue and prevent adhesions.
Permanent Changes in Gait or Posture
Orthopedic surgery can sometimes change a patient’s gait or posture. This is more common for surgeries in the lower body or spine.
For example, a hip replacement might require a patient to walk differently. This can lead to changes in their posture.
It’s vital for patients to talk to their healthcare provider about these possible long-term effects. This way, they can understand the risks and benefits of their surgery.
Special Considerations for Athletes and Active Individuals
Athletes and those who are very active need to think about how surgery affects their sports performance. Orthopedic surgery is often needed but can be tough for athletes.
Performance Limitations After Surgery
After surgery, athletes often find it hard to perform at their best. The surgery and recovery time can make it hard to do sports. For example, surgeries like joint replacements or ligament repairs mean athletes can’t do high-impact activities for a while.
The extent of these limitations depends on the surgery. For instance, a knee surgery might mean changing how an athlete trains to avoid stressing the knee too much.
Return to Sport Challenges
Getting back to sports after surgery is tough. It’s not just about getting physically better. Athletes need to regain their sport-specific skills and endurance too. Gradual progression under a doctor’s guidance is key to safely getting back to sports.
Athletes must go through thorough rehab. This includes physical therapy to build strength, flexibility, and coordination. The rehab plan is made to fit the athlete’s surgery and sport needs.
Increased Risk of Re-injury
One big worry for athletes after surgery is the increased risk of re-injury. The area that was operated on might be more likely to get hurt again. This is true if the athlete jumps back into sports too soon or without proper rehab.
Also, the body might find new ways to get hurt during recovery. This is why athletes need to work with their healthcare team. A good rehab plan can help avoid these risks.
Conclusion: Making Informed Decisions About Orthopedic Surgery
It’s important to know the downsides of orthopedic surgery to make smart health choices. Orthopedic surgery has both good and bad sides that need to be thought about carefully.
People thinking about orthopedic surgery should know about possible problems. These include infections, nerve damage, and when implants don’t work right. Knowing these risks helps prepare for the tough parts of recovery and getting better.
Deciding on orthopedic surgery means looking at the good and bad sides. Talking to your doctor about your situation and worries is key. This helps figure out the best treatment for you.
Being informed about the downsides of orthopedic surgery helps patients take charge of their health. This ensures they get the right treatment for their needs.
FAQ
What are the most significant risks associated with orthopedic surgery?
Orthopedic surgery can lead to infections, blood clots, nerve damage, and implant failure. It’s important to know these risks before deciding on surgery.
How does general anesthesia impact orthopedic surgery?
General anesthesia is key in many orthopedic surgeries. But, it also has risks like common complications and long-term effects.
What types of infections can occur after orthopedic surgery?
After surgery, you might face infections at the surgical site, deep tissue, bone, or around implants. These can affect your surgery’s outcome.
What are the risks of blood clots after orthopedic surgery?
Blood clots, like deep vein thrombosis, are a big risk. If not treated, they can lead to serious conditions like pulmonary embolism.
Can nerve damage occur during orthopedic surgery?
Yes, nerve damage is a possible complication. It can cause temporary or permanent effects on your nerves.
How is pain managed after orthopedic surgery?
Managing pain after surgery is key. But, it can be hard due to opioid risks and chronic pain.
What is the typical recovery timeline for orthopedic surgery?
Recovery times vary by procedure. But, most patients need a lot of rehab and physical therapy to get back to normal.
Can orthopedic surgery result in limited mobility?
Yes, surgery can limit your mobility. This can affect your daily life and might require special equipment.
What are the risks associated with implant failure in orthopedic surgery?
Implant failure, wear, and reactions to foreign bodies are risks. They can affect the success of your surgery.
How does orthopedic surgery impact mental health?
Surgery can deeply affect your mental health. You might experience depression, anxiety, and changes in how you see yourself.
What are the specific cons of joint replacement surgery?
Joint replacement surgery has risks like dislocation and limited prosthetic lifespan. These can affect your surgery’s success.
What are the specific cons of spine surgery?
Spine surgery is complex and risky. It can lead to failed back surgery syndrome and injuries to the spinal cord and nerves.
Can orthopedic surgery result in unsatisfactory outcomes?
Yes, surgery can fail. This might mean your symptoms don’t fully go away or you need more surgery.
What are the long-term side effects of orthopedic surgery?
Long-term effects include arthritis, scar tissue, and changes in how you move. These can impact your quality of life.
Are there special considerations for athletes undergoing orthopedic surgery?
Athletes face unique challenges after surgery. These include performance limits, challenges in returning to sports, and a higher risk of injury.
How can patients make informed decisions about orthopedic surgery?
Patients should understand the risks and benefits of surgery. This helps them make informed choices about their treatment.
References
- Al-Rumaih, M., et al. (2025). Vascular injuries and complications in orthopedic surgery: Incidence, risk factors, and management. Vascular Surgery, 89(1), 45-53. https://www.sciencedirect.com/science/article/pii/S2773157X24001309




































