
Childhood cancer is a tough diagnosis that hits thousands of families hard. It’s a leading cause of death in children. This makes the job of pediatric oncologists very important in the battle against this disease. Learn pediatric oncologist duties and how they help diagnose and treat childhood cancers.
Pediatric oncologists are dedicated to providing the best possible cancer care for children. Pediatric oncologists are doctors who focus on treating cancer in kids and teens. They handle everything from finding the cancer to treating it and checking on the kids later.
Knowing what pediatric oncologist duties are helps us see how complex their job is. It shows us how vital they are in fighting childhood cancer.
Key Takeaways
- Pediatric oncologists diagnose and treat cancer in children and adolescents.
- Their work involves a range of responsibilities, from diagnosis to treatment and follow-up care.
- Comprehensive cancer care for children is key to better treatment results.
- Pediatric oncologists play a vital role in the fight against childhood cancer.
- Understanding their duties is essential in appreciating their work.
Understanding the Role of a Pediatric Oncologist
Pediatric oncologists do more than just treat cancer. They also support and care for young patients and their families. These doctors have special training to diagnose and treat cancers in kids and teens.
Definition and Specialization
A pediatric oncologist is a doctor who specializes in treating cancers in children and young adults. They know how to help kids understand and deal with cancer. They focus on the unique needs of pediatric cancers, which are different from adult cancers.
To become a pediatric oncologist, doctors go through a lot of education and training. This includes:
- Getting an MD or DO degree from medical school.
- Completing a pediatric residency program.
- Getting specialized training in pediatric oncology through fellowship programs.
Importance in Pediatric Healthcare
Pediatric oncologists are key in pediatric healthcare. They not only treat cancer but also manage its side effects. They work with a team of healthcare professionals to give children the best care possible.
“The care of a pediatric oncologist is not limited to treating cancer; it’s about supporting the whole child and their family through a challenging journey.”
— Expert in Pediatric Oncology
Pediatric oncologists are important in several ways:
| Area of Impact | Description |
| Accurate Diagnosis | They use advanced techniques to find the exact type of cancer. |
| Personalized Treatment Plans | They create treatment plans that fit each child’s needs. |
| Supportive Care | They provide care that meets the physical, emotional, and social needs of the child and their family. |
Pediatric oncologists combine their knowledge, advanced treatments, and caring approach. They make a big difference in the lives of children with cancer.
Core Duties of Pediatric Oncologists
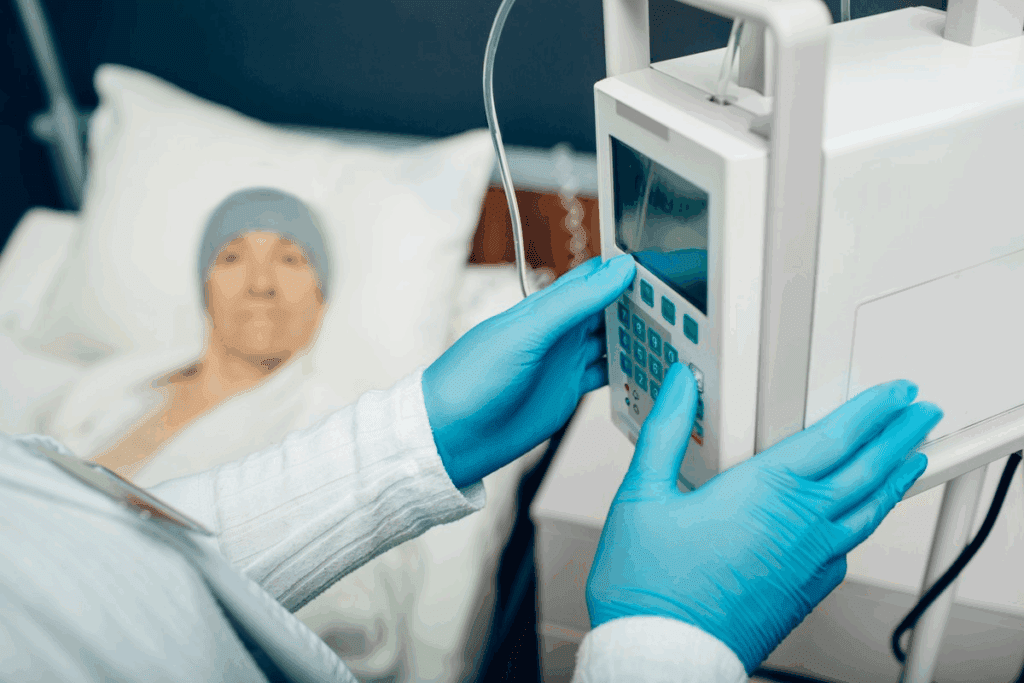
Pediatric oncologists handle a wide range of tasks, from diagnosing to treating and following up on patients. They are experts in treating children with cancer. They examine patients, order tests, and give treatments like chemotherapy.
Patient Diagnosis and Evaluation
Pediatric oncologists diagnose and evaluate children with cancer. They do detailed medical checks, order tests like imaging and biopsies, and interpret the results. Accurate diagnosis is key to finding the right treatment.
“Accurate diagnosis is the cornerstone of effective cancer treatment.” They use advanced tests to understand a child’s cancer. This helps them create effective treatment plans.
Develop Treatment Plans
After diagnosing, pediatric oncologists create treatment plans for each patient. These plans consider the cancer type, stage, and the child’s health. Treatments might include chemotherapy, radiation, or immunotherapy.
- Chemotherapy: Using drugs to kill cancer cells
- Radiation Therapy: Utilizing high-energy rays to target cancer cells
- Immunotherapy: Harnessing the body’s immune system to fight cancer
Coordination of Care
Pediatric oncologists work with other healthcare teams for complete care. They team up with surgeons, radiologists, nurses, and specialists. Good teamwork is vital for the best care for children with cancer.
“The care of a child with cancer is a team effort, requiring collaboration and coordination among healthcare professionals, families, and caregivers.”
Together, pediatric oncologists and healthcare teams provide top-notch care. They meet the complex needs of children with cancer.
Diagnostic Procedures Used by Pediatric Oncologists
To find and treat pediatric cancer, doctors use many tools. These tools help figure out the cancer type and how far it has spread. This information shapes the treatment plan.
Imaging Techniques
Imaging is key in finding pediatric cancer. We use:
- X-rays: To see bones and find problems.
- MRI (Magnetic Resonance Imaging): For detailed soft tissue images.
- CT scans (Computed Tomography): To see the body in cross-sections.
- Ultrasound: Uses sound waves to check organs and tissues.
These tools help us see how far the cancer has spread. They also help us check if treatment is working.
Biopsy Methods
A biopsy takes a tissue or cell sample for study. We use:
- Needle Biopsy: A needle collects tissue or fluid.
- Surgical Biopsy: Surgery removes a bigger tissue sample.
Biopsy results help us know the cancer type. This helps us plan the right treatment.
Blood Tests and Lab Work
Blood tests and lab work are key in diagnosing and watching pediatric cancer. We do:
- Complete Blood Count (CBC): Checks blood cell counts.
- Blood Chemistry Tests: Looks at organ function and finds issues.
- Tumor Markers: Finds substances from cancer cells.
These tests give us important info about the patient’s health. They help us change the treatment plan if needed.
By using these diagnostic tools together, we can accurately diagnose and manage pediatric cancer. This improves treatment chances and helps prevent cancer in children.
Treatment Options Available

Pediatric oncology therapies
We create treatment plans for kids with cancer that fit their needs. The plan depends on the cancer type, stage, and the child’s health.
Chemotherapy
Chemotherapy is key in treating many cancers in kids. It uses drugs to kill or slow cancer cells. We often mix different drugs for better results.
Key aspects of chemotherapy include:
- Administration: Chemotherapy can be given orally or intravenously.
- Side effects: Common side effects include nausea, hair loss, and fatigue.
- Monitoring: Regular blood tests and check-ups are critical to track how well the treatment is working and its side effects.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s used for cancers that are in one place or have spread to specific areas.
Benefits of radiation therapy include:
- Precision: Radiation can target cancer cells without harming nearby healthy tissues.
- Effectiveness: It works well for certain types of tumors.
Immunotherapy and Targeted Therapy
Immunotherapy and targeted therapy are new ways to fight cancer in kids. Immunotherapy boosts the immune system to fight cancer. Targeted therapy focuses on specific molecules that help cancer grow.
Advantages include:
- Specificity: Targeted therapy can harm fewer normal cells.
- Innovation: These therapies are leading in cancer research, giving new hope to patients.
| Treatment Type | Description | Key Benefits |
| Chemotherapy | Uses drugs to kill cancer cells | Effective for many cancer types, can be used in combination |
| Radiation Therapy | Uses high-energy rays to target cancer cells | Precise, effective for localized tumors |
| Immunotherapy | Boosts the immune system to fight cancer | Stimulates body’s natural defenses, potentially fewer side effects |
| Targeted Therapy | Targets specific molecules involved in cancer growth | Reduces harm to normal cells, innovative approach |
We keep improving in pediatric oncology, with a variety of treatments for each child. By mixing these therapies, we aim to better outcomes and quality of life for our young patients.
Managing Pediatric Cancer Symptoms
Managing symptoms in kids with cancer is key to bettering their life quality. We know a full approach is needed to meet their complex needs.
Pain Management
Pain is a big issue for kids with cancer. Effective pain management uses both medicines and non-medical methods. We use drugs and also distraction, relaxation, and physical therapy to help them.
It’s vital to check and change pain plans often. This keeps kids comfortable and happy.
Supporting Mental Health
Cancer and treatment can really affect a child’s mind. We offer supportive care like counseling and therapy. This helps kids and their families deal with the emotional side of cancer.
Our team works with mental health experts. We make sure kids get the emotional support they need. This includes help with anxiety, depression, and other feelings that come up during treatment.
Nutritional Guidance
Good nutrition is key for kids with cancer. We give nutritional guidance to help with symptoms like nausea and loss of appetite. These can hurt a child’s nutrition.
Our support includes special diets, supplements, and tips for eating. We make sure kids get the nutrients they need. This helps them stay healthy and handle treatment better.
By focusing on pain, mental health, and nutrition, we make a big difference. Our detailed approach to managing symptoms is part of our top-notch care promise.
Family Involvement in Pediatric Oncology
Effective care in pediatric oncology needs a team effort that includes the family. We know that family support is key for kids with cancer.
Educating Parents and Caregivers
We, as pediatric oncologists, teach parents and caregivers about the diagnosis and treatment. We aim to give clear, easy-to-understand information. This helps families make informed decisions for their child’s care.
For example, we explain the reasons behind each treatment, what to expect, and possible risks. This open talk helps reduce fears and misconceptions. It makes the care environment more supportive.
Supporting Family Members
Supporting family members is a big part of our job. A cancer diagnosis impacts the whole family, not just the child. We offer emotional support and counseling to help families deal with the stress and uncertainty.
We also connect families with resources and support groups. Here, they can share experiences and find comfort in knowing they’re not alone. This support network is very helpful in facing the challenges of pediatric cancer treatment.
Involving Children in Care Decisions
Involving children in their care decisions is delicate but important. We believe in being honest with kids about their condition and treatment. We use language that fits their age and understanding.
By letting children help with decisions, we help them feel more in control. This can greatly improve their cooperation and well-being during treatment.
| Aspect of Care | Family Involvement | Benefits |
| Education | Understanding diagnosis and treatment | Informed decision-making |
| Emotional Support | Coping with diagnosis and treatment | Reduced stress and anxiety |
| Care Decisions | Involving children in treatment plans | Improved cooperation and well-being |
Working Collaboratively with Other Healthcare Professionals
Pediatric cancer treatment is complex and needs a team effort. Pediatric oncologists know that treating children with cancer is more than just medicine. It’s about caring for their whole being, including their body, mind, and spirit.
Multidisciplinary Teams
A team in pediatric oncology includes many experts like surgeons and nurses. Working together, they make sure every part of a child’s care is covered. This team approach helps us understand each child’s needs better and tailor their treatment.
When a child is diagnosed with cancer, the team talks about the best treatment. This might include surgery, chemo, or radiation. The team’s knowledge helps us pick the best treatment for each child.
Referrals to Specialists
Referrals to specialists are key in pediatric oncology. Children might need to see experts like neurosurgeons or cardiologists. As pediatric oncologists, we help arrange these referrals and make sure our patients get the care they need.
| Specialist | Role in Pediatric Oncology |
| Neurosurgeon | Surgical intervention for brain tumors |
| Orthopedic Surgeon | Surgical intervention for bone tumors |
| Cardiologist | Monitoring cardiac health during and after treatment |
Importance of Communication
Good communication is vital in pediatric oncology. Clear and timely talks among healthcare professionals keep everyone on the same page. This improves care and helps with the emotional and psychological aspects of treatment.
Team meetings are important for discussing patient progress and making changes to treatment plans. Open communication ensures seamless care that meets our patients’ changing needs.
As we move forward in pediatric oncology, teamwork is more important than ever. By working together and keeping communication open, we can give children with cancer the best care possible.
Research and Advancements in Pediatric Oncology
The field of pediatric oncology is seeing big changes thanks to ongoing research and trials. We’re working hard to find new ways to treat cancer in kids. This ensures they get the best care possible.
Emerging Trends in Pediatric Cancer Research
Research today focuses on the genetic and molecular causes of childhood cancers. This helps us create targeted treatments that are more effective and less harmful.
Immunotherapy is a big trend now. It uses the body’s immune system to fight cancer. Immunotherapy has shown great promise in treating different types of pediatric cancers. It offers hope to kids who haven’t responded well to other treatments.
The Role of Clinical Trials in Pediatric Oncology
Clinical trials are key in moving pediatric oncology forward. They test the safety and effectiveness of new treatments. We’re involved in many trials to explore new therapies, like:
- Targeted therapy
- Immunotherapy
- Precision medicine
These trials are vital for introducing new treatments to pediatric cancer care. They help improve outcomes and reduce side effects for kids with cancer.
| Type of Clinical Trial | Focus | Potential Benefits |
| Phase I | Safety and dosage | Identifies safe doses and possible side effects |
| Phase II | Efficacy | Checks if the treatment works |
| Phase III | Comparative effectiveness | Compares the new treatment with standard ones |
Future Directions in Pediatric Cancer Treatment
As research keeps growing, we expect big leaps in pediatric oncology. We’re looking at using artificial intelligence in diagnosis and treatment planning. We also aim to create treatments tailored to each child’s cancer based on their genetic profile.
The future of pediatric oncology looks bright. Ongoing research and trials will lead to better, less harmful treatments. This will greatly improve the lives of children with cancer.
The Emotional Aspects of Pediatric Oncology
When a child gets a cancer diagnosis, it changes their life and the lives of their family and caregivers. This diagnosis brings big emotional challenges. We focus on giving full support to help them through this tough time.
Emotional Support During Diagnosis
Dealing with a diagnosis is hard. We offer emotional support and resources to help families get through this. Our team is here to care for the emotional and mental health of kids and their families.
Resources for Ongoing Support
We have many resources for emotional support, like counseling and support groups. We want to make sure families get the help they need before, during, and after treatment.
Importance of Long-term Follow-Up Care
Long-term care is key for kids who have had cancer. We stress the need for ongoing care. This helps watch for late effects of treatment and keeps emotional support going.
FAQ
What is the role of a pediatric oncologist in treating childhood cancer?
Pediatric oncologists focus on treating cancer in kids and teens. They provide care and support from start to finish.
How do pediatric oncologists diagnose cancer in children?
They use imaging, biopsies, and lab tests to find cancer. This helps them plan the best treatment.
What treatment options are available for childhood cancer?
Kids can get chemotherapy, radiation, immunotherapy, and targeted therapy. Doctors create a plan based on the cancer type and the child’s health.
How do pediatric oncologists manage symptoms in children with cancer?
They use pain management and support mental health. They also help with nutrition to improve life quality during treatment.
What is the importance of family involvement in pediatric oncology?
Family support is key. Doctors educate and support families. They involve kids in decisions and offer ongoing care.
How do pediatric oncologists work with other healthcare professionals?
They work in teams with other doctors. This ensures kids get the best care possible.
What is the current state of research in pediatric oncology?
Research is always ongoing. It aims to find better treatments and improve outcomes for kids with cancer.
How do pediatric oncologists support the emotional needs of children with cancer and their families?
They offer emotional support and resources. This helps families cope with the diagnosis and treatment.
What is the significance of long-term follow-up care in pediatric oncology?
It’s vital for monitoring treatment effects. It also provides ongoing support to families.
How do pediatric oncologists develop treatment plans for children with cancer?
They plan based on cancer type, stage, and the child’s health. They work with other doctors for a complete care plan.
References:
- McEachron, T. A. (2021). Recent advances in pediatric cancer research. Pediatric Research. https://pubmed.ncbi.nlm.nih.gov/34561271/
- McKenna, K. (2010). Parental involvement in paediatric cancer treatment decision-making processes. Pediatric Oncology Unit Study. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178788/

































