Beta thalassemia major, also known as Cooley’s anemia, is a severe inherited blood disorder that greatly reduces hemoglobin production. This leads to chronic and life-threatening anemia from early childhood.
Also called b thal major, this condition makes it difficult for the body to produce beta-globin — a key protein needed to form hemoglobin and healthy red blood cells. Understanding b thal major and how to manage it can significantly improve the quality of life for those affected.
Managing beta thalassemia well means getting the right care and treatments.
Key Takeaways
- Beta thalassemia major is a severe inherited blood disorder.
- It significantly reduces hemoglobin production.
- Chronic anemia is a major complication.
- Understanding the condition is key for effective management.
- Comprehensive care improves life quality.
Understanding B Thal Major: Definition and Clinical Significance
Beta thalassemia major is a genetic disorder that makes it hard for the body to make healthy hemoglobin. It’s also known as Cooley’s anemia. People with this condition often have severe anemia, poor growth, and skeletal issues. If not treated, it can cause death, usually from heart failure.
What is Beta Thalassemia Major (Cooley’s Anemia)?
Beta thalassemia major is a severe form of thalassemia. It happens when someone gets two mutated beta-globin genes, one from each parent. This leads to a big drop or total loss of beta-globin chain production. This causes severe anemia and other health problems.
The Spectrum of Beta Thalassemia Conditions
Beta thalassemia ranges from mild to severe. The severity depends on how many mutated genes a person has and how big the mutation is. Heterozygous thalassemia means having one normal and one mutated gene, leading to mild or no symptoms. On the other hand, homozygous thalassemia means two mutated genes, causing the severe form of the disease.
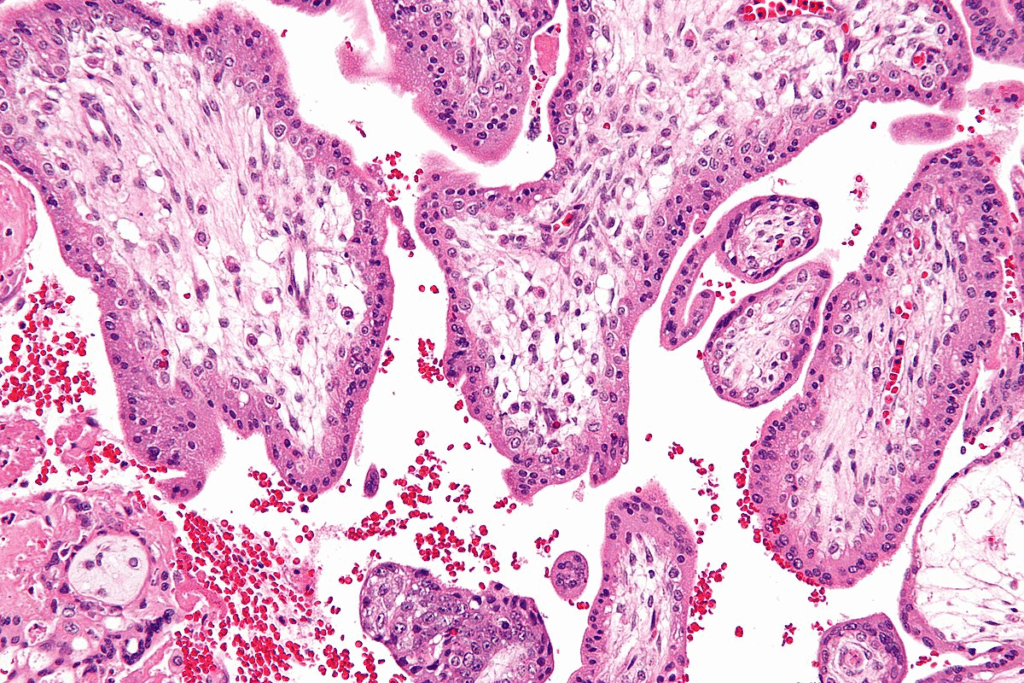
Impact on Hemoglobin Production
The main issue with beta thalassemia major is how it affects hemoglobin production. Without enough beta-globin chains, there’s too much alpha-globin. This causes damage to red blood cells. Symptoms include severe anemia, fatigue, pallor, delayed growth, bone deformities, and an enlarged spleen.
| Condition | Genetic Status | Symptoms |
| Beta Thalassemia Major | Homozygous Mutation | Severe anemia, growth delays, bone deformities |
| Beta Thalassemia Minor | Heterozygous Mutation | Mild or no symptoms |
The Genetic Foundation of Beta-Thalassemia
Understanding the genetics of beta thalassemia is key to managing it. Beta thalassemia major, also known as Cooley’s anemia, is a severe form. It happens due to genetic mutations that affect the beta-globin chains of hemoglobin.
Beta Thalassemia Gene Mutations
Beta thalassemia is caused by mutations in the HBB gene. These mutations cause a lack of beta-globin chains, which are vital for hemoglobin. The severity of the condition varies based on the type and extent of these mutations.
Inheritance Patterns and Risk Factors
Beta thalassemia is inherited in an autosomal recessive pattern. This means a person needs two mutated genes (one from each parent) to have the major form of the disease. Carriers, with one normal and one mutated gene, usually have mild or no symptoms but can pass the mutated gene to their children.
Heterozygous Thalassemia vs. Homozygous Presentation
Carriers of beta thalassemia (heterozygous) often have a milder form or no symptoms. On the other hand, those who are homozygous (have two mutated genes) have beta thalassemia major. This is a severe form with serious anemia and other health issues. Knowing the genetic status is important for genetic counseling and family planning.
The genetic foundation of beta thalassemia shows why genetic testing and counseling are vital for families with this condition.
Key Fact 1: Global Distribution and Epidemiology
Beta thalassemia major, also known as Cooley’s anemia, is found worldwide, but more in certain areas. It’s common in places where malaria used to be a big problem. This is because the thalassemia trait helped protect against malaria.
Prevalence in Mediterranean Regions
The Mediterranean is a hotspot for beta thalassemia. Countries like Greece, Italy, and Cyprus have a lot of carriers and people with the condition. To deal with it, these places have started screening programs and genetic counseling.
Middle Eastern and Southeast Asian Populations
Beta thalassemia is also big in the Middle East and Southeast Asia. Places like Iran, Saudi Arabia, and Thailand have a lot of carriers. This makes it a big health issue in these areas.
Thalassemia in the United States
In the U.S., beta thalassemia is more common in people from the Mediterranean, Middle East, and Southeast Asia. It’s not as common as in other places, but it’s important to screen those at risk.
Key Fact 2: Clinical Manifestations and Early Signs
It’s important to know the signs of beta thalassemia major for early treatment. This condition shows many symptoms that can really affect a person’s life.
Chronic Anemia and Its Systemic Effects
Chronic anemia is a big problem in beta thalassemia major. It happens because the body doesn’t make enough beta-globin chains of hemoglobin. This causes fatigue, weakness, and pallor.
The anemia makes the body try to make blood cells in places other than the bone marrow. This can lead to more health issues.
Growth Delays and Developmental Issues
Children with beta thalassemia major might grow slower and face developmental problems. This is because of the chronic anemia and iron overload. It can slow down the growth of bones and organs, causing delayed puberty and other issues.
Fatigue, Pallor, and Quality of Life Impact
Patients with beta thalassemia major often feel fatigue and pallor. These symptoms really hurt their quality of life. They make it hard to do everyday things and affect their happiness.
It’s key to manage these symptoms well. This can greatly improve the life of these patients.
Key Fact 3: Complications of Beta Thalassemia Major
Beta thalassemia major causes many problems, like bone and heart issues. These need careful management. The disease affects many parts of the body, needing a detailed care plan.
Bone Deformities and Skeletal Changes
Bone changes are a big issue in beta thalassemia major. The bone marrow grows too much, causing skeletal deformities. This can make cheekbones stick out and change the face shape.
These changes happen because the bone marrow grows. It tries to make more red blood cells.
Splenomegaly and Hepatomegaly
Another problem is big spleen and liver. This is because of too many red blood cells. The body tries to clean out damaged cells, but it can harm organs over time.
Cardiac and Endocrine Complications
Heart problems are a big worry in beta thalassemia major. This is because of iron overload from blood transfusions. Iron can cause heart failure and irregular heartbeats.
Also, endocrine issues like growth hormone and thyroid problems can happen. This is because iron builds up in glands.
Managing these problems is key to a better life for those with beta thalassemia major. A good care plan is vital for managing the disease well.
Diagnostic Approaches for B-Thalassemia
Diagnosing beta thalassemia major requires a detailed process. It includes blood tests and genetic studies. Getting the diagnosis right is key to managing the condition well.
Complete Blood Count and Hemoglobin Analysis
The first step is a Complete Blood Count (CBC). It checks the patient’s hemoglobin and red blood cells. Hemoglobin electrophoresis then spots any odd hemoglobin types.
Genetic Testing and Mutation Identification
Genetic testing is critical. It finds the HBB gene mutations that cause beta thalassemia. Knowing this helps plan the treatment.
Prenatal Diagnosis and Genetic Counseling
For families with beta thalassemia history, prenatal diagnosis is possible. It can find the condition in the fetus. Genetic counseling helps discuss risks and options.
Healthcare providers use these methods to give detailed care. This care is tailored for patients with beta thalassemia major.
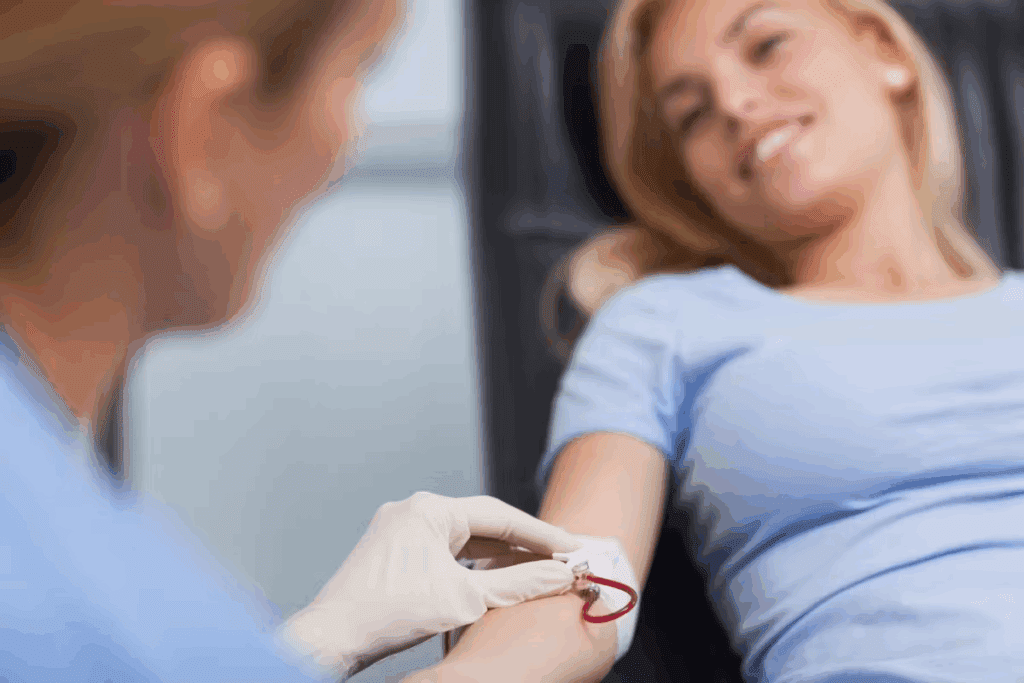
Key Fact 4: Blood Transfusion Therapy Protocols
Blood transfusions are key in treating beta thalassemia major. They keep hemoglobin levels healthy, lowering the chance of serious problems.
Importance of Regular Transfusion Regimens
For those with beta thalassemia major, regular blood transfusions are essential. They help:
- Keep hemoglobin levels up
- Lessen the risk of anemia-related issues
- Boost overall life quality
Sticking to transfusion schedules is critical. It keeps hemoglobin levels stable. Irregular transfusions can cause big health problems.
Transfusion Schedules and Hemoglobin Targets
Transfusion plans are made for each patient. Hemoglobin targets are usually 9-12 g/dL. It’s important to check hemoglobin levels often to adjust transfusions as needed.
Managing Transfusion Reactions and Complications
Even though blood transfusions save lives, they can cause issues like transfusion reactions, iron overload, and infections. To manage these, healthcare teams use:
- Watching for signs of transfusion reactions
- Iron chelation therapy to handle iron overload
- Testing blood products for infections
Understanding the role of blood transfusions and following set protocols helps healthcare teams improve care for beta thalassemia major patients.
Key Fact 5: Iron Overload and Chelation Management
Iron overload is a big problem for people with beta thalassemia major. They need regular blood transfusions to keep their hemoglobin levels up. But, these transfusions lead to too much iron in the body.
This extra iron can harm the heart, liver, and endocrine glands. It’s a serious issue that needs careful management.
Mechanisms of Iron Accumulation
Iron overload happens because of repeated blood transfusions. Each transfusion adds a lot of iron to the body. Over time, the body can’t handle all this iron.
Iron starts to build up in tissues and organs. This can cause heart problems, liver damage, and issues with the endocrine system.
Types of Iron Chelation Medications
Iron chelation therapy is key in managing iron overload. There are different chelators, each with its own benefits and side effects.
- Deferoxamine: Given through subcutaneous or intravenous infusion, deferoxamine has been used for years.
- Deferiprone: An oral chelator, deferiprone is good at reducing iron in the heart.
- Deferasirox: Taken orally, deferasirox is given once a day. This makes it easier for patients to stick to their treatment.
The right chelator depends on the patient’s needs, how severe the iron overload is, and other health conditions.
Monitoring Iron Burden and Therapy Adjustment
Managing iron overload means keeping an eye on iron levels and adjusting treatment as needed. Serum ferritin levels are often used to check iron stores. But, they can be affected by other things.
Direct measures like liver iron concentration (LIC) from biopsy or MRI can give a clearer picture of iron levels.
| Monitoring Method | Description | Frequency |
| Serum Ferritin | Marker of iron stores | Every 1-3 months |
| Liver Iron Concentration (LIC) | Direct measure of liver iron | Annually or as needed |
| T2* MRI | Assessment of cardiac iron | Annually or as needed |
By watching iron levels closely and adjusting treatment, doctors can reduce the risks of iron overload. This helps improve the lives of patients with beta thalassemia major.
Key Fact 6: Stem Cell Transplantation as Curative Therapy
Hematopoietic stem cell transplantation is seen as a cure for beta thalassemia major. It gives hope to those affected. This method replaces the patient’s bad bone marrow with healthy stem cells from a donor.
Patient Selection and Donor Matching
Success in stem cell transplantation relies on picking the right patient and matching the donor. Patients are checked to see if they’re healthy enough and match with a donor. Amatched sibling donor is the best choice for this treatment.
Transplantation Procedure and Post-Transplant Care
The transplant process starts with making the patient’s body ready by using chemotherapy or radiation. Then, the donor’s stem cells are given to the patient. After the transplant, it’s important to watch for any problems and manage them.
Long-Term Outcomes and Success Rates
Studies show good results for patients who get stem cell transplants for beta thalassemia major. With the right donor and care after the transplant, many patients can be cured. They no longer need blood transfusions or chelation therapy for life.
Key Fact 7: Emerging Gene Therapy Approaches
Gene therapy is making big strides as a possible cure for beta thalassemia major. It changes a patient’s genes to make healthy hemoglobin. This tackles the disorder’s root cause.
Current Research and Clinical Trials
Many clinical trials are testing gene therapy for beta thalassemia. They use viral vectors to add a working HBB gene to stem cells.
Gene therapy is showing great promise in early trials. Some patients have stopped needing blood transfusions. But, there are hurdles like ensuring it works long-term and managing side effects.
Gene Addition and Gene Editing Strategies
Gene therapy for beta thalassemia uses two main methods: gene addition and gene editing. Gene addition adds a healthy gene to cells. Gene editing, like CRISPR/Cas9, fixes the mutation directly.
Gene editing could lead to a lasting cure by fixing the genetic flaw precisely. But, it’s complex and raises ethical and technical questions.
Future Prospects for Genetic Cure
The outlook for gene therapy in beta thalassemia is bright. Ongoing studies aim to make these treatments safer and more effective. A successful gene therapy could cure not just beta thalassemia but also other forms like heterozygous thalassemia.
| Gene Therapy Approach | Description | Potential Benefits |
| Gene Addition | Introduces a healthy copy of the HBB gene into hematopoietic stem cells. | Potential for long-term correction of beta thalassemia. |
| Gene Editing | Uses CRISPR/Cas9 to directly correct the HBB gene mutation. | Precise correction of the genetic defect, potentially leading to a cure. |
As research keeps improving, gene therapy might become a real option for beta thalassemia patients. It could bring a genetic cure within reach.
Comprehensive Care Models for Beta Thalassemia
Beta thalassemia major needs a detailed and coordinated care plan. This is to handle its complex symptoms and related issues.
A key part of this care is the multidisciplinary team approach. This involves hematologists, cardiologists, endocrinologists, and more. They work together to tackle the disease’s different parts.
Multidisciplinary Team Approach
The multidisciplinary team is essential for caring for beta thalassemia patients. They collaborate to:
- Keep an eye on anemia and transfusion needs
- Manage heart and hormone problems
- Offer support to patients and their families
Advanced Protocols and Quality Improvement
Using advanced treatment plans, like regular blood transfusions and iron chelation, is key. Ongoing quality improvement helps make these plans better. This leads to better results for patients.
International Treatment Standards
Following international treatment standards is vital. These standards are based on the latest research and guidelines. They help manage beta thalassemia well.
With a care model that includes a team approach, advanced treatments, and international standards, care can improve. This leads to a better life for beta thalassemia patients.
Conclusion: Advancing Beta Thalassemia Management
New treatments and care methods are making a big difference for those with beta thalassemia major. Research and new treatments give hope for better managing beta thalassemia.
It’s important to know what beta thalassemia disease is to manage it well. This disease affects how the body makes hemoglobin, leading to severe anemia and other issues.
Gene therapy and stem cell transplants are changing how we treat beta thalassemia. These new methods could cure beta thalassemia, greatly improving patients’ lives around the world.
Good care for beta thalassemia needs a team approach and the latest treatments. Healthcare teams must keep up with new research and guidelines to give the best care to patients with beta thalassemia major.
FAQ
What is beta thalassemia major?
Beta thalassemia major, also known as Cooley’s anemia, is a severe form of thalassemia. It causes significant health issues from early childhood. This is due to a genetic mutation affecting hemoglobin production.
What are the symptoms of beta thalassemia major?
Symptoms include chronic anemia, fatigue, and pallor. Growth delays and developmental issues also occur. These symptoms significantly impact the quality of life.
How is beta thalassemia major diagnosed?
Diagnosis involves a complete blood count and hemoglobin analysis. Genetic testing to identify mutations is also done. Prenatal diagnosis is used for at-risk pregnancies.
What is the genetic basis of beta thalassemia?
Beta thalassemia is caused by mutations in the beta-globin gene. It is inherited in an autosomal recessive pattern. Heterozygous individuals are carriers, while homozygous individuals have the major form.
How is beta thalassemia major managed?
Management includes regular blood transfusions. Iron chelation therapy is used to manage iron overload. In some cases, stem cell transplantation is considered as a curative therapy.
What is iron overload in beta thalassemia major?
Iron overload occurs due to repeated blood transfusions. It leads to iron accumulation in organs. This can cause cardiac, hepatic, and endocrine complications.
What is the role of gene therapy in beta thalassemia?
Gene therapy aims to correct the genetic defect causing beta thalassemia. It uses gene addition or gene editing strategies. This offers a potentially curative approach.
How does beta thalassemia major affect quality of life?
Beta thalassemia major significantly impacts quality of life. It causes chronic anemia and frequent medical interventions. It also has the risk of complications, requiring a complete care model.
What is the global distribution of beta thalassemia?
Beta thalassemia is prevalent in Mediterranean, Middle Eastern, and Southeast Asian populations. The frequency varies by region.
Can beta thalassemia major be cured?
While traditional management involves lifelong treatment, stem cell transplantation and emerging gene therapies offer hope. They are considered curative options for some patients.
Reference
- CDC Thalassemia Healthcare Provider Resource Toolkit
https://www.cdc.gov/thalassemia/hcp/toolkit/index.html