Last Updated on November 20, 2025 by Ugurkan Demir

Sickle Cell Disease (SCD) is a major health concern, particularly for people of African descent. It is an inherited blood disorder affecting millions worldwide.
In the United States, approximately 100,000 people live with SCD. This condition significantly impacts both quality of life and sickle cell disease life expectancy.
Studies show that individuals with SCD typically live between 52 and 54 years. Understanding sickle cell disease life expectancy highlights the need for improved treatments and comprehensive care to enhance outcomes for those affected.
Key Takeaways
- Sickle Cell Disease is a prevalent genetic disorder affecting approximately 100,000 people in the US.
- The condition significantly impacts life expectancy, with an average range of 52 to 54 years.
- SCD is mainly found in people of African descent.
- Improving medical care is key to better life quality and expectancy for SCD patients.
- Liv Hospital is dedicated to top-notch care for complex hereditary conditions like SCD.
Understanding Sickle Cell Disease: A Genetic Blood Disorder

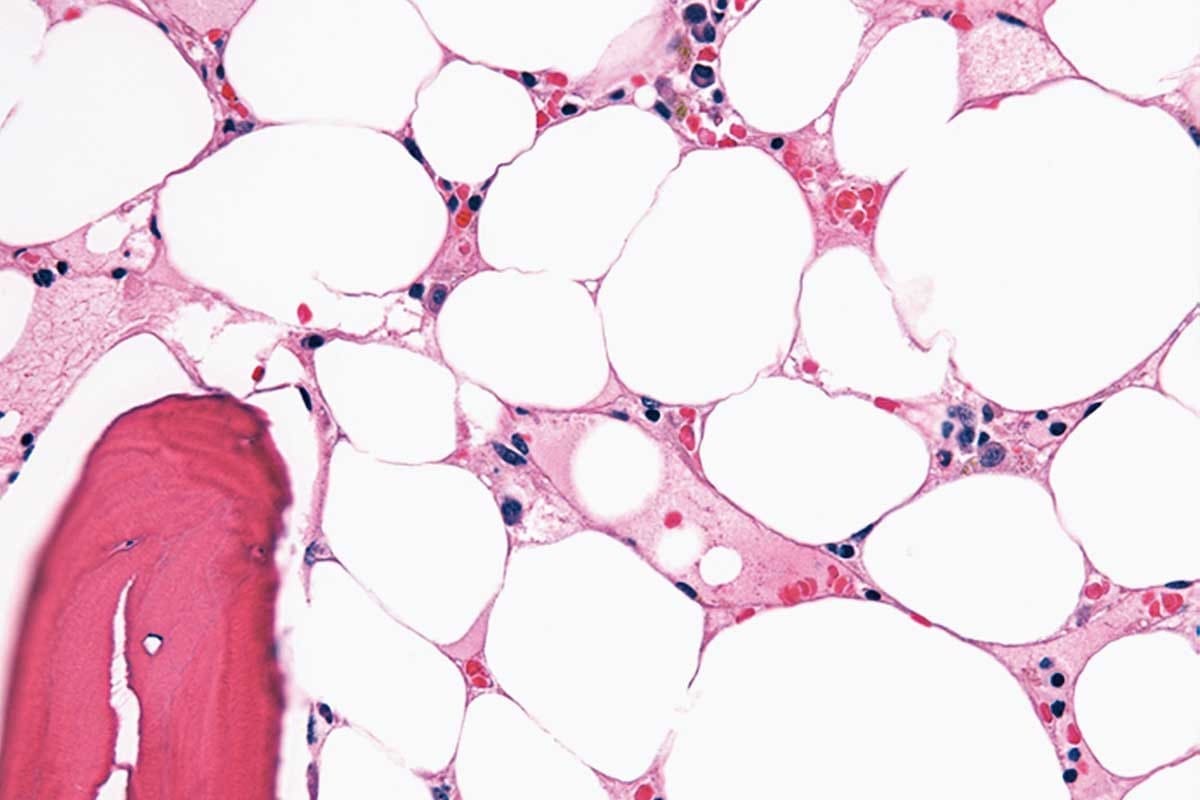
Sickle Cell Disease (SCD) is a genetic disorder that affects red blood cells. It changes how these cells carry oxygen. This is because of a problem with the hemoglobin protein in the cells.
The Science Behind Sickle Cell Disease
SCD comes from a mutation in the HBB gene. This gene is important for making hemoglobin. The mutation leads to sickle hemoglobin, or HbS, which makes red blood cells sickle-shaped and fragile.
This mutation is a single change in the HBB gene. It swaps glutamic acid for valine at the sixth position of the beta-globin chain. This causes hemoglobin to clump together when there’s less oxygen. This is why red blood cells become misshapen.
How Sickle Cell Trait Differs from the Disease
It’s important to know the difference between sickle cell trait and Sickle Cell Disease. People with the sickle cell trait have one normal and one mutated HBB gene. They usually don’t show the full symptoms of SCD but can pass the mutated gene to their kids.
The main differences are:
- Genetic Makeup: SCD has two mutated HBB genes, while the trait has one normal and one mutated gene.
- Symptoms: SCD causes severe anemia, pain, and infections. The trait is usually symptom-free.
- Risk to Offspring: Carriers of the sickle cell trait can pass the mutated gene to their children. This can lead to SCD if the other parent is also a carrier.
Knowing these differences is key for genetic counseling. It helps people make informed choices about their health and family planning.
Genetic Inheritance Patterns of Sickle Cell Disease

Sickle Cell Disease follows an autosomal recessive inheritance pattern. This means a person needs two abnormal hemoglobin genes, one from each parent, to have the disease.
This pattern is key to understanding the risks for future children. If both parents carry the sickle cell gene, there’s a 25% chance each child will have SCD. A 50% chance they’ll be a carrier, and a 25% chance they won’t have SCD or be a carrier.
Autosomal Recessive Inheritance
In autosomal recessive inheritance, the disease shows up when someone has two mutated genes. Carriers, with one normal and one mutated gene, usually don’t show symptoms but can pass the mutated gene to their kids.
- A person with SCD has two abnormal hemoglobin genes.
- Carriers have one normal and one abnormal gene.
- The risk of passing the mutated gene to offspring depends on the genotype of both parents.
Carrier Status and Risk Factors
Being a carrier of the sickle cell gene is usually not harmful. But it’s important for family planning. Carriers are often healthy or have mild symptoms but can pass the gene to their children. When both parents are carriers, there’s a higher risk their kids could get SCD.
Knowing if you’re a carrier is key to understanding the risk of SCD in your children. Genetic testing can tell you if you’re a carrier. This helps with making family planning decisions.
Genetic Counseling Considerations
Genetic counseling is vital for families with SCD. It explains the risks of passing the disease to future children and what it means to be a carrier. Counselors help families understand their risks, make informed choices about having children, and manage the disease well.
- Genetic counseling helps families understand the inheritance pattern of SCD.
- It provides information on the risks associated with being a carrier.
- Counselors can discuss various reproductive options and management strategies for SCD.
By grasping the genetic inheritance of Sickle Cell Disease, families can better handle the risks and implications. This helps them make informed decisions about their health and family planning.
Global Prevalence of Sickle Cell Disease
Sickle Cell Disease is a big health issue worldwide, mainly in certain places. It affects many people in different parts of the world. The rates of this disease vary greatly.
Worldwide Distribution Patterns
The spread of Sickle Cell Disease is not even across the globe. It’s more common in places where malaria used to be a big problem. This is because the sickle cell trait helps protect against malaria.
- Sub-Saharan Africa: This area has the most cases of SCD. Countries like Nigeria, Democratic Republic of Congo, and Uganda are hit hard.
- India and the Middle East: SCD is also common in parts of India and the Middle East. It’s a big health problem there.
- Mediterranean regions: Places near the Mediterranean, like Greece and Turkey, also see SCD cases.
High-Prevalence Regions
High-prevalence areas have a lot of people carrying the sickle cell gene. These places often had malaria in the past.
The global prevalence of SCD is quite high, with millions affected. The worldwide distribution shows the need for focused health efforts in these areas.
- Nigeria has a huge burden of SCD.
- The Democratic Republic of Congo and Uganda also have a lot of SCD cases.
- India’s tribal groups are hit hard by SCD.
Knowing where SCD is most common is key to fighting it. It helps in making health plans to manage and prevent SCD.
Sickle Cell Disease in the United States: Demographics and Statistics
Sickle Cell Disease (SCD) affects many people in the United States. Its impact varies by race and ethnicity. Knowing the demographics and statistics of SCD helps meet the healthcare needs of those affected.
Overall Prevalence in the US Population
The Centers for Disease Control and Prevention say SCD affects about 1 in 365 Black or African American births in the US. This shows how SCD impacts this group. The overall prevalence of SCD in the US is key for planning healthcare and public health strategies.
Key Statistics:
- SCD affects about 100,000 people in the United States.
- It occurs in approximately 1 in 365 Black or African American births.
- SCD also affects individuals of other racial and ethnic backgrounds, though less often.
Racial and Ethnic Distribution
SCD is more common among Black or African Americans in the US. But, it can also be found in Hispanic, Middle Eastern, and South Asian populations.
Notable Trends:
- Increased prevalence among minority populations.
- Genetic diversity contributes to SCD in non-Black populations.
- Growing awareness of SCD beyond traditional high-risk groups.
Geographic Hotspots Within the US
SCD is not spread evenly across the US. Some areas have more cases due to their demographics. Places with large African American populations tend to have higher SCD rates.
Regional Prevalence:
| Region | Prevalence |
| Northeast | Higher prevalence due to urban centers. |
| Southern States | Significant SCD prevalence, correlating with higher African American populations. |
Knowing these hotspots is vital for targeted public health efforts and resource planning.
The African American Connection: Dispelling Myths and Misconceptions
SCD is more common among African Americans, but it’s not just for them. It’s a genetic disorder that affects how red blood cells work. It’s found worldwide, showing it’s not just a racial issue.
Historical Context and Evolutionary Advantage
SCD is more common in African descendants because of malaria. The sickle cell trait helped protect against malaria. This gave an evolutionary edge in malaria-prone areas.
Key historical factors include:
- The geographic distribution of malaria and its impact on populations.
- The genetic adaptation of the sickle cell trait as a response to malaria.
- The transatlantic slave trade, which led to the spread of the sickle cell gene across different regions.
Beyond Race: Understanding the Genetic Basis
SCD comes from a mutation in the HBB gene. Knowing this helps with diagnosis and treatment.
| Genetic Aspect | Description |
| Autosomal Recessive Inheritance | SCD is inherited in an autosomal recessive pattern, meaning an individual must inherit two mutated HBB genes to express the disease. |
| Carrier Status | Individuals with one mutated gene are carriers and typically do not display the full symptoms of SCD but can pass the mutation to their offspring. |
| Genetic Testing | Genetic testing can identify carriers and affected individuals, aiding in family planning and early intervention. |
By understanding the genetic and historical contexts of SCD, we can work towards dispelling misconceptions and improving care for those affected.
Sickle Cell Disease Life Expectancy: Current Statistics
It’s important to know the life expectancy stats for Sickle Cell Disease patients. This info helps doctors and those with the disease. Thanks to new medical care, life expectancy has gotten better.
Average Life Expectancy for SCD Patients
In the US, SCD patients live between 52 and 54 years, studies show. This is a big jump from before. It’s thanks to better disease management and treatments.
Current statistics show a gap in life expectancy is getting smaller. Better healthcare and early treatment help a lot.
Comparison to General Population
SCD patients live shorter lives than the average American. The general population lives about 78 years. This shows the ongoing challenge for SCD patients.
| Population Group | Average Life Expectancy (Years) |
| SCD Patients | 52-54 |
| General Population | 78 |
Trends in Survival Rates Over Time
Survival rates for SCD patients have improved over time. New treatments like disease-modifying drugs and blood transfusions have helped.
Emerging therapies, like gene therapy, could improve life expectancy even more. Research and development are key to closing the life expectancy gap.
Medical Complications That Impact Life Expectancy
Patients with Sickle Cell Disease often face a shorter life expectancy. This is due to various acute and chronic medical issues. These problems can greatly reduce their quality of life and increase the risk of early death.
Acute Complications
Acute complications in Sickle Cell Disease are sudden and can be life-threatening. They need quick treatment to avoid serious harm. Some major acute complications include:
- Pain Crises: Severe pain episodes caused by vaso-occlusion. These can be triggered by dehydration, cold weather, or stress.
- Acute Chest Syndrome: A condition with a new lung issue on chest X-rays, often with fever, breathing problems, or chest pain. It’s a big cause of illness and death in SCD patients.
- Stroke: Ischemic or hemorrhagic strokes can happen due to sickled red blood cells blocking or rupturing brain blood vessels.
- Infections: SCD patients are more likely to get infections, mainly from encapsulated organisms, because of functional asplenia.
A medical expert notes, “Acute complications in SCD patients need immediate medical care to avoid long-term harm or death.”
“Acute chest syndrome is a medical emergency that requires prompt diagnosis and treatment to reduce morbidity and mortality.”
Chronic Complications
Chronic complications in Sickle Cell Disease come from repeated vaso-occlusion and hemolysis. This leads to organ damage over time. Some notable chronic complications include:
| Complication | Description | Impact on Life Expectancy |
| Chronic Anemia | Persistent anemia due to hemolysis | Reduces oxygen delivery to tissues, contributing to organ damage |
| Pulmonary Hypertension | High blood pressure in the arteries that supply the lungs | Increases the risk of heart failure and mortality |
| Renal Dysfunction | Damage to the kidneys due to sickling and vaso-occlusion | Can lead to end-stage renal disease, requiring dialysis or transplantation |
Managing these complications well is key to improving life quality and expectancy for Sickle Cell Disease patients. Regular monitoring and preventive care can help reduce some of these risks.
Screening, Early Detection, and Preventive Care
Improving life for SCD patients starts with early detection and care. Sickle Cell Disease is a genetic disorder that can be managed well with early action.
Newborn Screening Programs
Newborn screening programs are key in finding SCD early. They use a simple blood test to check for the sickle cell gene. Early diagnosis leads to early preventive actions, lowering the risk of SCD complications.
In the U.S., all states screen newborns for SCD. This means babies with the disease are found soon after birth. Healthcare providers can then closely watch the child’s health and act quickly if needed.
Prenatal Testing Options
Prenatal testing lets parents find out if their unborn child has SCD. They can learn if their baby has SCD or is a carrier. This knowledge helps them make choices about the pregnancy and prepare for a child with SCD.
Parents can choose from CVS and amniocentesis for prenatal testing. These tests can spot SCD in the fetus. This way, parents can plan and prepare for their child’s future.
Regular Health Monitoring for SCD Patients
SCD patients need regular health checks. Preventive care includes vaccinations, regular visits, and watching for complications. By managing the disease, patients can lower the risk of serious problems and live better lives.
| Preventive Measure | Benefit |
| Newborn Screening | Early diagnosis and intervention |
| Prenatal Testing | Informed decision-making for expectant parents |
| Regular Health Monitoring | Reduced risk of complications, improved quality of life |
Modern Treatments Improving Quality of Life and Survival
Medical treatments have greatly improved life and survival for those with Sickle Cell Disease (SCD). These treatments help manage symptoms and treat the disease’s root causes. This gives patients a better outlook than ever before.
Disease-Modifying Medications
Disease-modifying drugs, like hydroxyurea, are key in SCD care. Hydroxyurea boosts fetal hemoglobin, cutting down on pain crises and blood transfusions. A study in the New England Journal of Medicine showed it reduces pain crises.
“Hydroxyurea is a well-tolerated and effective treatment that has been shown to reduce the frequency of painful crises and improve quality of life for patients with SCD.”
N Engl J Med
Other treatments are being researched, aiming to find new ways to help.
Blood Transfusion Therapy
Blood transfusions are vital in SCD care. They lower the risk of serious problems by reducing sickled red blood cells. Chronic transfusion therapy is used for those at high risk of stroke or severe issues.
- Reduces the risk of stroke and other complications
- Decreases the frequency of painful crises
- Improves overall quality of life
Stem Cell Transplantation
Stem cell transplantation is the only cure for SCD. It replaces the patient’s marrow with healthy donor marrow. Though risky, it’s considered for severe cases.
Emerging Gene Therapies
Gene therapy is a new hope for SCD. It aims to fix the genetic issue causing the disease. Clinical trials are testing its safety and effectiveness.
- Gene editing, like CRISPR/Cas9, might fix the SCD mutation.
- Lentiviral vectors are used to give healthy HBB gene to stem cells.
These new treatments and therapies are changing SCD care. They offer hope for a better life and survival.
Conclusion: Living Well with Sickle Cell Disease
Understanding Sickle Cell Disease (SCD) is key for those affected by it. SCD’s impact varies worldwide, with some areas and groups hit harder. In the U.S., it’s more common among African Americans, but it affects others too.
Managing SCD is vital to avoid complications and enhance life quality. Thanks to medical progress, people with SCD can now live more fulfilling lives. This includes regular health checks, certain medications, and sometimes blood transfusions or stem cell transplants.
Knowing the genetic roots of SCD helps individuals manage their health better. Ongoing research and awareness are critical for better care and outcomes. With proper management, SCD’s effects on life expectancy and well-being can be lessened.
FAQ
How prevalent is sickle cell disease?
Sickle cell disease affects about 100,000 people in the United States. About 1 in 365 African Americans are born with it.
Does sickle cell disease only affect African Americans?
No, it’s not just African Americans. People from Mediterranean, Middle Eastern, and Indian backgrounds can also have it.
What is the difference between having the sickle cell trait and having sickle cell disease?
The sickle cell trait means carrying one mutated HBB gene. Sickle cell disease means having two mutated HBB genes, one from each parent.
How is sickle cell disease inherited?
It’s inherited in an autosomal recessive pattern. A person needs two mutated HBB genes, one from each parent, to have the disease.
What are the risks associated with being a carrier of the sickle cell trait?
Carriers are usually healthy. But they can pass the mutated gene to their kids. These kids might get sickle cell disease if they get another mutated gene from the other parent.
Where is sickle cell disease most common globally?
It’s most common in sub-Saharan Africa, the Mediterranean, and parts of the Middle East and India.
What is the average life expectancy for individuals with sickle cell disease?
Life expectancy has improved. But it’s lower than average. People with sickle cell disease usually die in their mid-40s.
What are the acute and chronic complications of sickle cell disease?
Acute complications include pain crises, acute chest syndrome, and stroke. Chronic complications include anemia, organ damage, and increased infection risk.
How can sickle cell disease be managed effectively?
Effective management includes regular health checks, medications like hydroxyurea, blood transfusions, and preventive measures to avoid complications.
What is the role of newborn screening programs in detecting sickle cell disease?
Newborn screening programs are key. They detect sickle cell disease early. This allows for timely interventions and preventive care to improve outcomes.
Are there any emerging treatments for sickle cell disease?
Yes, gene therapies are promising. Ongoing research is exploring new ways to manage and potentially cure the condition.
References
- Ganesh, R., & Bhor, M. (2023). Sickle cell disease cuts 20 years from life expectancy, study finds. The American Journal of Managed Care. https://www.ajmc.com/view/sickle-cell-disease-cuts-20-years-from-life-expectancy-study-finds