Red blood cell (RBC) disorders affect millions worldwide. They make it hard for the body to carry oxygen, leading to health problems. Understanding these conditions is key for the right diagnosis and treatment. At Liv Hospital, we offer top-notch, patient-focused care and the latest research for these illnesses.
We will look at seven common red blood cell disorders, giving you the important facts quickly. Blood cell disorders cover a wide range of conditions. They can affect different parts of the blood, from mild to severe. Knowing about these conditions helps patients understand their diagnosis and treatment options better.
Key Takeaways
- Red blood cell disorders affect the quantity, quality, shape, or function of red blood cells.
- These conditions can lead to various health issues due to impaired oxygen transport.
- Liv Hospital provides complete care for patients with red blood cell disorders.
- Understanding red blood cell disorders is vital for proper diagnosis and treatment.
- Seven common red blood cell disorders will be explored, providing key facts at a glance.
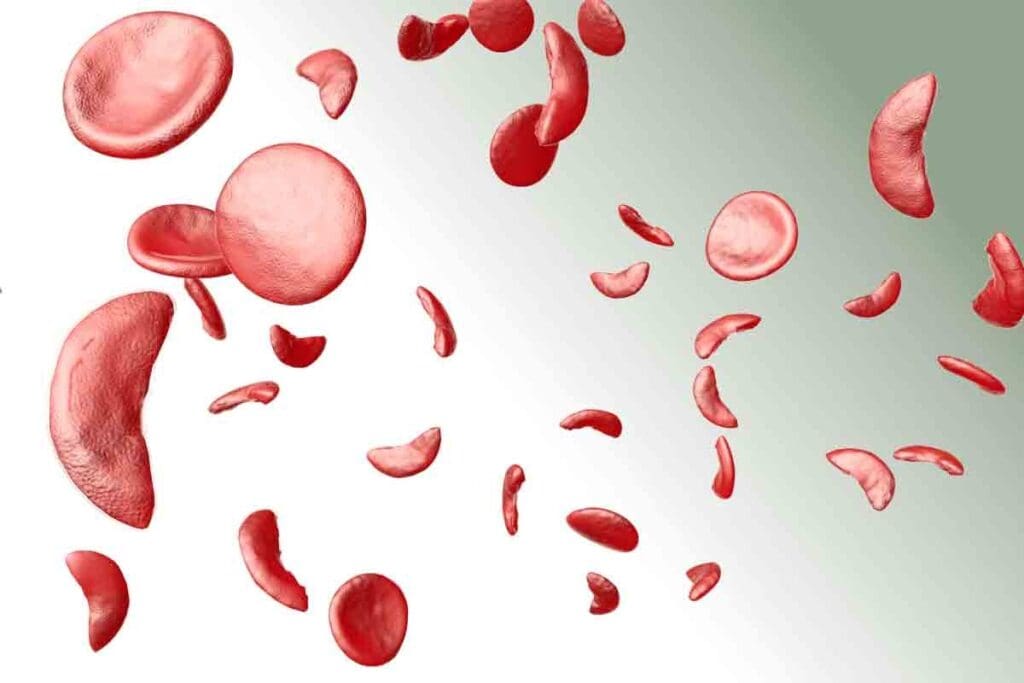
Understanding Red Blood Cells and Their Function

Red blood cells are key for carrying oxygen around our body. This is vital for our survival. They help keep our body’s internal balance.
The Role of Red Blood Cells in Oxygen Transport
Red blood cells, or erythrocytes, carry oxygen from the lungs to our body’s tissues. They also take carbon dioxide from tissues back to the lungs. This is thanks to hemoglobin, a protein in red blood cells that binds to oxygen.
Red blood cells are very important for oxygen transport. Without enough, our body’s tissues wouldn’t get the oxygen they need. This can cause fatigue, weakness, and shortness of breath.
“The primary function of red blood cells is to deliver oxygen to the body’s tissues, a task that is critical for life and supporting the body’s metabolic processes.”
Normal Red Blood Cell Production and Lifecycle
Red blood cells are made in the bone marrow through erythropoiesis. This process turns hematopoietic stem cells into mature red blood cells. These cells then enter the bloodstream.
Red blood cells live about 120 days. After that, they are removed and broken down. Their parts are recycled or excreted. This cycle keeps the body’s red blood cell supply steady.
Things like nutritional deficiencies, chronic diseases, and genetic disorders can upset this balance. This can cause blood disorders or red blood cell illness.
Knowing how red blood cells are made and live is key for diagnosing and treating related disorders. Recognizing signs of abnormal red blood cell function or production helps healthcare providers act early. This can prevent serious problems.
Overview of RBC Diseases and Their Impact on Health

Red blood cell disorders can greatly affect a person’s life and health. These conditions change how red blood cells are made, look, and work. This leads to many health problems.
We will look at what red blood cell diseases are, how they are classified, and their effects on health.
Definition and Classification of Red Blood Cell Disorders
Red blood cell disorders, or RBC diseases, are a group of conditions. They affect the number, quality, shape, or function of red blood cells. These disorders can be divided into several types, including:
- Anemias: a lack of red blood cells or hemoglobin
- Polycythemias: too many red blood cells
- Morphological disorders: changes in red blood cell shape
- Enzymopathies: problems with enzymes in red blood cells
Knowing these categories helps doctors diagnose and treat RBC diseases better.
How Red Blood Cell Abnormalities Affect Oxygen Delivery
Red blood cells are key in carrying oxygen to all parts of the body. Problems with these cells can make it hard to get oxygen. This can cause fatigue, weakness, and shortness of breath.
In anemia, for example, there are fewer red blood cells or less hemoglobin. This makes it harder to transport oxygen, leading to these symptoms.
The table below shows how different RBC abnormalities affect oxygen delivery:
| RBC Abnormality | Effect on Oxygen Delivery |
| Anemia | Reduced oxygen-carrying capacity |
| Polycythemia | Increased blood viscosity, potentially impairing oxygen delivery |
| Sickle Cell Disease | Abnormal hemoglobin structure impairs oxygen transport |
Global Prevalence and Public Health Significance
RBC diseases affect millions of people worldwide. They are more common in some places due to genetics, environment, and social factors.
Public health initiatives are key to raising awareness and improving care for RBC diseases. We need to work together to tackle these global health issues.
Common Symptoms and Warning Signs of Red Blood Cell Disorders
Knowing the signs of RBC disorders can help catch problems early. These disorders affect how red blood cells are made, work, or last. This can cause many health problems.
Physical Manifestations: Fatigue, Weakness, and Pallor
Fatigue and weakness are common signs. They happen when tissues don’t get enough oxygen.
Pale skin, or pallor, is another sign. It shows there are fewer red blood cells or they can’t carry enough hemoglobin.
Cardiovascular and Respiratory Symptoms
RBC disorders can also cause heart and lung problems. This is because the body tries to make up for not getting enough oxygen. Symptoms include:
- Shortness of breath (dyspnea)
- Rapid heartbeat (tachycardia)
- Dizziness or lightheadedness
When to Seek Medical Attention
If you have ongoing or serious symptoms, see a doctor. Early treatment can greatly help those with RBC disorders.
| Symptom | Description | Possible RBC Disorder |
| Fatigue | Persistent feeling of tiredness | Anemia, Sickle Cell Disease |
| Pallor | Pale skin | Iron-Deficiency Anemia |
| Shortness of Breath | Difficulty breathing | Severe Anemia, Thalassemia |
Iron-Deficiency Anemia: The World’s Most Common RBC Disorder
Iron-deficiency anemia affects over 1.6 billion people worldwide. It happens when the body doesn’t have enough iron. Iron is key for making hemoglobin, which carries oxygen in red blood cells.
Causes and Risk Factors
Iron-deficiency anemia can come from not eating enough iron, losing blood too much, or needing more iron during pregnancy. Chronic blood loss is a big risk factor. This can be from ulcers or heavy periods. People with some gut problems also absorb iron poorly.
The main risk factors are:
- Not eating enough iron
- Having diseases like celiac or Crohn’s
- Being pregnant or breastfeeding
- Donating blood often
Diagnosis and Laboratory Findings
To find iron-deficiency anemia, doctors use tests and check-ups. They look for low hemoglobin, small red blood cells, and low serum ferritin. Serum ferritin shows how much iron is stored in the body.
| Laboratory Test | Normal Range | Iron-Deficiency Anemia |
| Hemoglobin (g/dL) | 13.8-17.2 (male) | Decreased |
| MCV (fL) | 80-100 | Decreased |
| Serum Ferritin (ng/mL) | 20-250 | Decreased |
Treatment Approaches and Prevention Strategies
Treatment for iron-deficiency anemia includes iron pills and eating more iron. Oral iron supplements are often the first choice. Sometimes, iron given through a vein is needed. To prevent it, eat foods high in iron and vitamin C, which helps your body absorb iron better.
Knowing how to treat and prevent iron-deficiency anemia helps doctors help their patients. This improves health outcomes for many.
Sickle Cell Disease: A Genetic Red Blood Cell Disorder
Sickle cell disease is caused by a genetic mutation. This leads to abnormal hemoglobin production and misshapen red blood cells. It affects millions worldwide. We will look into its causes, symptoms, and how to manage it.
Pathophysiology and Inheritance Patterns
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation creates hemoglobin S, which changes red blood cells into a sickle shape under low oxygen.
The disease is inherited in an autosomal recessive pattern. This means a person needs two defective HBB genes, one from each parent, to have the disease.
Inheritance Patterns:
| Genotype | Phenotype | Risk of Passing to Offspring |
| Normal (AA) | Normal | Low |
| Carrier (AS) | Generally Normal | 50% chance of passing the mutated gene |
| Affected (SS) | Sickle Cell Disease | 100% chance of passing the mutated gene |
Clinical Manifestations and Complications
Sickle cell disease causes many symptoms. These include pain episodes, anemia, infections, and damage to organs over time. The sickling of red blood cells can block small blood vessels, causing tissue damage.
Common Complications:
- Acute Chest Syndrome
- Stroke
- Splenic Sequestration
- Aplastic Crisis
Management Approaches and Recent Advances
Managing sickle cell disease involves several steps. These include managing pain, preventing infections, and watching for complications. New treatments include hydroxyurea to reduce pain episodes and gene therapy to fix the genetic defect.
Emerging Treatments:
| Treatment | Description | Benefits |
| Hydroxyurea | Reduces frequency of painful crises | Decreased morbidity |
| Gene Therapy | Aims to correct genetic defect | Potential cure |
| Blood Transfusions | Reduces risk of complications | Improved outcomes |
Thalassemia: Understanding the Spectrum of Disorders
Thalassemias are a group of inherited blood disorders. They need careful management. These disorders affect hemoglobin production, causing symptoms from mild to severe.
Alpha and Beta Thalassemia Variants
Thalassemia is mainly split into alpha and beta types. Alpha thalassemia happens when there’s a problem with the alpha-globin genes. Beta thalassemia is caused by issues with the beta-globin genes.
Alpha Thalassemia: Its severity depends on how many genes are affected. It can range from a mild carrier state to severe hemoglobin H disease. The most severe is hemoglobin Bart’s hydrops fetalis syndrome.
Beta Thalassemia: Beta thalassemia major, or Cooley’s anemia, is the most severe. It affects both beta-globin genes. Beta thalassemia intermedia is less severe, with symptoms varying.
Severity Levels and Clinical Presentation
Thalassemia’s symptoms vary greatly. They can range from no symptoms to severe anemia needing transfusions. Common signs include fatigue, weakness, and pale skin.
| Disease Variant | Severity Level | Clinical Features |
| Alpha Thalassemia | Silent Carrier to HbH Disease | Mild to Severe Anemia, Splenomegaly |
| Beta Thalassemia Major | Severe | Severe Anemia, Growth Failure, Skeletal Changes |
| Beta Thalassemia Intermedia | Moderate | Variable Anemia, Splenomegaly |
Treatment Strategies and Genetic Counseling
Treatment for thalassemia varies by severity and type. It includes blood transfusions, iron chelation, and sometimes bone marrow transplants. Genetic counseling helps families understand the risk of passing it on to their children.
It’s key to have a detailed management plan. This includes regular check-ups, treatment, and support for mental health. It helps improve life quality for those with thalassemia.
Disorders of Red Cell Morphology: Spherocytosis and Elliptocytosis
Red blood cell abnormalities like spherocytosis and elliptocytosis affect the shape and function of red blood cells. These issues can cause health problems because the abnormal shape makes it hard for red blood cells to carry oxygen well.
Cellular Abnormalities and Genetic Basis
Spherocytosis makes red blood cells round instead of their usual disk shape. This shape change is often caused by genetic mutations affecting proteins in the red blood cell membrane. Elliptocytosis, on the other hand, makes red blood cells oval-shaped due to similar genetic mutations.
The genetics behind these disorders can be inherited in different ways. Some cases follow an autosomal dominant pattern, while others are recessive. Knowing the genetic cause is key for diagnosis and treatment.
Diagnostic Approaches and Clinical Features
Diagnosing these disorders involves clinical evaluation, lab tests, and sometimes genetic analysis. A complete blood count (CBC) and a peripheral blood smear are key initial tests. They help spot the abnormal shapes of red blood cells.
The symptoms of spherocytosis or elliptocytosis can vary. Some people may not show symptoms at all, while others may have severe anemia, jaundice, and an enlarged spleen. The severity of the condition determines the treatment needed.
Management Options and Long-term Outlook
Managing spherocytosis and elliptocytosis aims to reduce symptoms and prevent complications. For many, removing the spleen can greatly reduce hemolysis and improve life quality. But, this decision depends on individual risks and benefits.
Supportive care, like folic acid supplements, is also important. Regular check-ups with a healthcare provider are necessary to monitor the condition and adjust treatment as needed.
With proper management, people with these disorders can live active lives. Advances in genetic counseling and diagnostics help us better understand and manage these conditions.
RBC Enzymopathies: Metabolic Disorders Affecting Red Blood Cells
Metabolic disorders affecting red blood cells, known as RBC enzymopathies, can cause significant health problems if not properly managed. These conditions impact the enzymes within red blood cells, potentially leading to abnormalities of blood cells.
G6PD Deficiency and Other Common Enzymopathies
G6PD deficiency is one of the most common RBC enzymopathies, affecting millions worldwide. It is a genetic disorder that occurs when the body lacks sufficient glucose-6-phosphate dehydrogenase, an enzyme that helps red blood cells function normally. Other enzymopathies, such as pyruvate kinase deficiency, also affect red blood cell metabolism, leading to conditions like hemolytic anemia.
We recognize that these conditions can have a significant impact on patients’ quality of life. Early diagnosis and proper management are key to preventing complications and improving outcomes.
Triggers and Management Considerations
Individuals with RBC enzymopathies need to be aware of triggers that can lead to hemolytic crises. Common triggers include certain medications, infections, and specific foods. For example, people with G6PD deficiency should avoid fava beans and certain antibiotics.
Management strategies typically involve avoiding known triggers, maintaining a healthy lifestyle, and, in some cases, receiving medical treatment to manage symptoms. We emphasize the importance of personalized care plans tailored to each patient’s specific condition and needs.
Preventive Measures and Lifestyle Adjustments
Preventive measures play a vital role in managing RBC enzymopathies. Patients should be educated on recognizing early symptoms of hemolytic crises and seeking medical attention promptly. Lifestyle adjustments, such as dietary changes and avoiding certain environmental exposures, can also help mitigate risks.
By understanding their condition and working closely with healthcare providers, individuals with RBC enzymopathies can lead active and fulfilling lives. We are committed to providing support and guidance to help patients navigate their condition effectively.
Polycythemia Vera and Erythrocytosis: Excess RBC Production Disorders
Polycythemia vera and erythrocytosis are disorders where too many red blood cells are made. This can make blood thicker and increase the risk of blood clots. It’s important to diagnose and treat these conditions to avoid serious problems.
Causes and Classification
Polycythemia vera is a type of cancer that makes too many red and white blood cells, and platelets. Erythrocytosis is when only red blood cells are made in excess. Knowing why these happen helps doctors manage them better.
Most polycythemia vera cases are caused by a genetic mutation, like the JAK2 V617F mutation. Erythrocytosis can be caused by low oxygen levels, tumors, or certain medicines.
Symptoms and Complications
Symptoms of these conditions vary. People might feel headaches, dizzy, or tired because their blood is thicker. Serious problems like blood clots can also happen, leading to strokes or heart attacks.
Those with polycythemia vera might also have an enlarged spleen. This can cause belly pain and feeling full too soon.
Treatment Approaches and Monitoring
Treating these conditions aims to prevent blood clots and ease symptoms. Doctors might use blood removal, medicines like hydroxyurea, or low-dose aspirin to prevent clots.
It’s key to keep an eye on how the treatment is working. This helps adjust the plan as needed and manage any side effects. Each patient’s treatment should be tailored to their specific situation.
Diagnostic Approaches for Identifying Abnormal Erythrocytes
It’s key to accurately diagnose abnormal erythrocytes for managing red blood cell disorders. A mix of lab tests and clinical checks helps doctors find the cause of these issues.
Complete Blood Count and Blood Smear Analysis
A complete blood count (CBC) is a first step in diagnosing red blood cell disorders. It shows the number and quality of red blood cells. A blood smear analysis looks at red blood cells to spot shape problems.
Genetic Testing and Family Screening
Genetic tests are key for diagnosing genetic disorders like sickle cell disease and thalassemia. They check DNA for specific mutations. Family screening helps find carriers and affected family members for early help and advice.
Advanced Diagnostic Techniques in Hematology
New methods in diagnosing blood cells have improved. Flow cytometry spots specific cells, and molecular diagnostics find genetic mutations. These tools make diagnosis more accurate and help plan treatments.
Treatment Strategies and Management of RBC Diseases
Managing red blood cell (RBC) diseases needs a deep understanding of treatment options. We will look at different ways to manage these conditions. This will help improve patient outcomes and quality of life.
Medication Options and Supplementation
Medicines are key in treating RBC diseases. For example, iron chelation therapy helps reduce iron overload in thalassemia and sickle cell disease. Deferoxamine and deferasirox are common iron chelators. Folic acid is also recommended to support red blood cell production.
Other drugs, like hydroxyurea, help reduce pain in sickle cell disease. We will talk about the benefits and possible side effects of these treatments.
| Medication | Condition | Purpose |
| Deferoxamine | Thalassemia, Sickle Cell Disease | Iron Chelation |
| Deferasirox | Thalassemia, Sickle Cell Disease | Iron Chelation |
| Hydroxyurea | Sickle Cell Disease | Reduce painful crises |
| Folic Acid | Various RBC Diseases | Support Erythropoiesis |
Blood Transfusions and Cellular Therapies
Blood transfusions are vital for managing some RBC diseases, like sickle cell disease and thalassemia major. They help by reducing the risk of complications and ensuring enough oxygen delivery.
Cellular therapies, including gene therapy, are showing promise. They aim to fix the genetic issues causing the disease.
Emerging Treatments and Clinical Trials
New treatments for RBC diseases are being developed. These include new drugs, gene editing, and other innovative methods. They are in clinical trials now.
We are dedicated to keeping up with these new treatments. This way, we can offer our patients the best and latest care.
Conclusion: Living with Red Blood Cell Disorders and Future Perspectives
We’ve looked into the world of red blood cell disorders. We’ve covered their types, how to diagnose them, and how to treat them. Managing these conditions means creating a plan that fits each person’s needs.
New discoveries in hematology have made treating RBC disorders better. New treatments and ongoing studies give hope for a better life for those with these conditions.
Knowing about the different RBC diseases helps us give better care. Our goal is to offer top-notch healthcare and support to patients from around the world. We want to make sure they get the best care possible.
We’re always working to improve in hematology. Our commitment is to care for our patients and their families with kindness and expertise. We aim to improve their well-being.
FAQ
What are Red Blood Cell (RBC) disorders?
RBC disorders affect the number, shape, or function of red blood cells. This can impact how well oxygen is delivered to the body.
What are the common symptoms of RBC disorders?
Symptoms include feeling tired, weak, and pale. You might also have heart or breathing problems. The exact symptoms depend on the disorder.
What is Iron-Deficiency Anemia?
Iron-Deficiency Anemia happens when the body doesn’t have enough iron. This leads to fewer red blood cells and less oxygen being carried.
What is Sickle Cell Disease?
Sickle Cell Disease is a genetic condition. It causes red blood cells to be shaped like sickles. This can lead to health problems.
What is Thalassemia?
Thalassemia is a group of disorders caused by genetic changes. These changes affect hemoglobin production, leading to anemia and other issues.
What are RBC Enzymopathies?
RBC Enzymopathies, like G6PD deficiency, are metabolic disorders. They make red blood cells more prone to damage and destruction.
How are RBC disorders diagnosed?
Doctors use lab tests like Complete Blood Count and blood smears. They also do genetic testing and other advanced tests.
What are the treatment options for RBC disorders?
Treatment depends on the disorder. It can include medicines, blood transfusions, cellular therapies, and changes in lifestyle.
Can RBC disorders be managed effectively?
Yes, with the right diagnosis and treatment, many RBC disorders can be managed. This improves life quality and reduces complications.
Are there any emerging treatments for RBC disorders?
Yes, new treatments are being developed. These include gene therapy and other innovative approaches.
How can I prevent RBC disorders?
Some disorders are genetic, but others can be prevented or managed. This includes a balanced diet, avoiding triggers, and regular medical check-ups.
Reference
- National Heart, Lung, and Blood Institute. (2022, September). Anemia: Symptoms, causes, and treatments. National Institutes of Health. https://www.nhlbi.nih.gov/health/anemia