Last Updated on November 20, 2025 by Ugurkan Demir
We often think sickle cell disease only affects certain groups. But it’s not true. Sickle cell disease can happen to anyone, no matter their background. Learn white sickle cell disease statistics, symptoms, and demographics.
About 1 in 333 white newborns in the U.S. has sickle cell trait. It’s more common in African populations. But it’s important to know Caucasians, like those from southern Europe, can also get it.
At LivHospital, we know how vital it is to care for everyone with sickle cell disease. Our team is here to offer top-notch support and guidance.
Key Takeaways
- Sickle cell disease is not exclusive to specific ethnic groups and can affect Caucasians.
- The prevalence of sickle cell trait in white newborns is about 1 in 333 in the United States.
- Caucasians from southern Europe are among those who can be affected by sickle cell disease.
- Comprehensive care is key for those with sickle cell disease, no matter their ethnicity.
- LivHospital is committed to providing expert support for those affected by sickle cell disease.
The Science Behind Sickle Cell Disease
It’s important to understand sickle cell disease to see how it affects people. SCD is a genetic disorder that changes how red blood cells make hemoglobin. It happens because of a mutation in the HBB gene.
What Causes Sickle Cell Disease
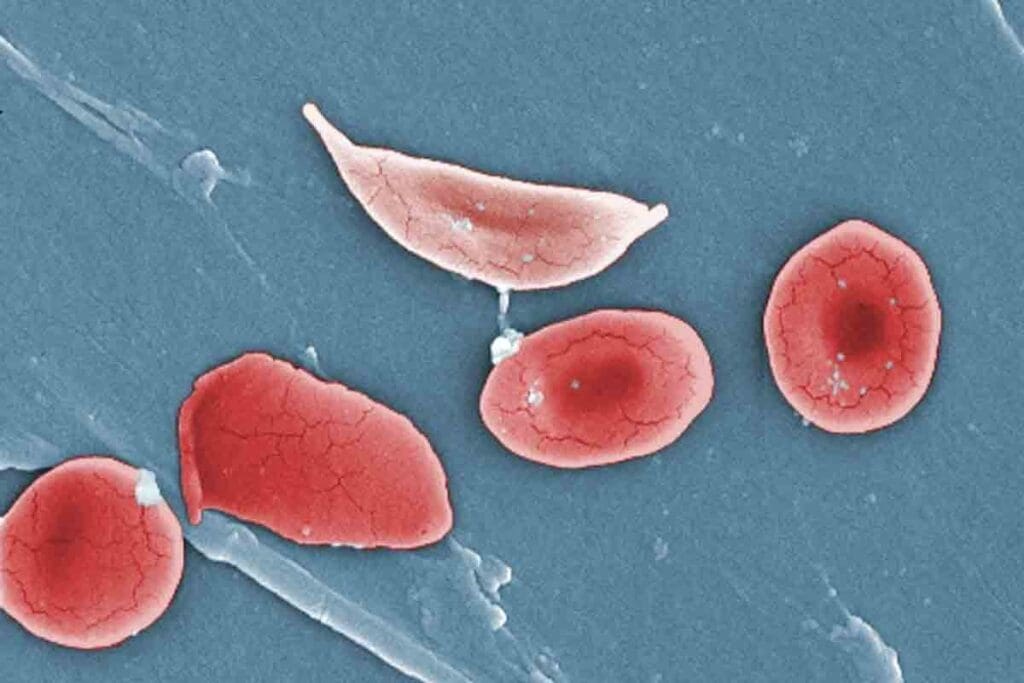
Sickle cell disease happens when someone gets two bad copies of the HBB gene, one from each parent. This leads to sickle hemoglobin, or HbS. The HbS causes red blood cells to bend into a sickle shape under certain conditions. This shape makes them break down early and causes problems.
“The genetic basis of sickle cell disease is rooted in a single nucleotide mutation in the HBB gene,” explains a leading researcher in hematology. “This mutation leads to the substitution of glutamic acid with valine at the sixth position of the beta-globin chain, resulting in HbS.”
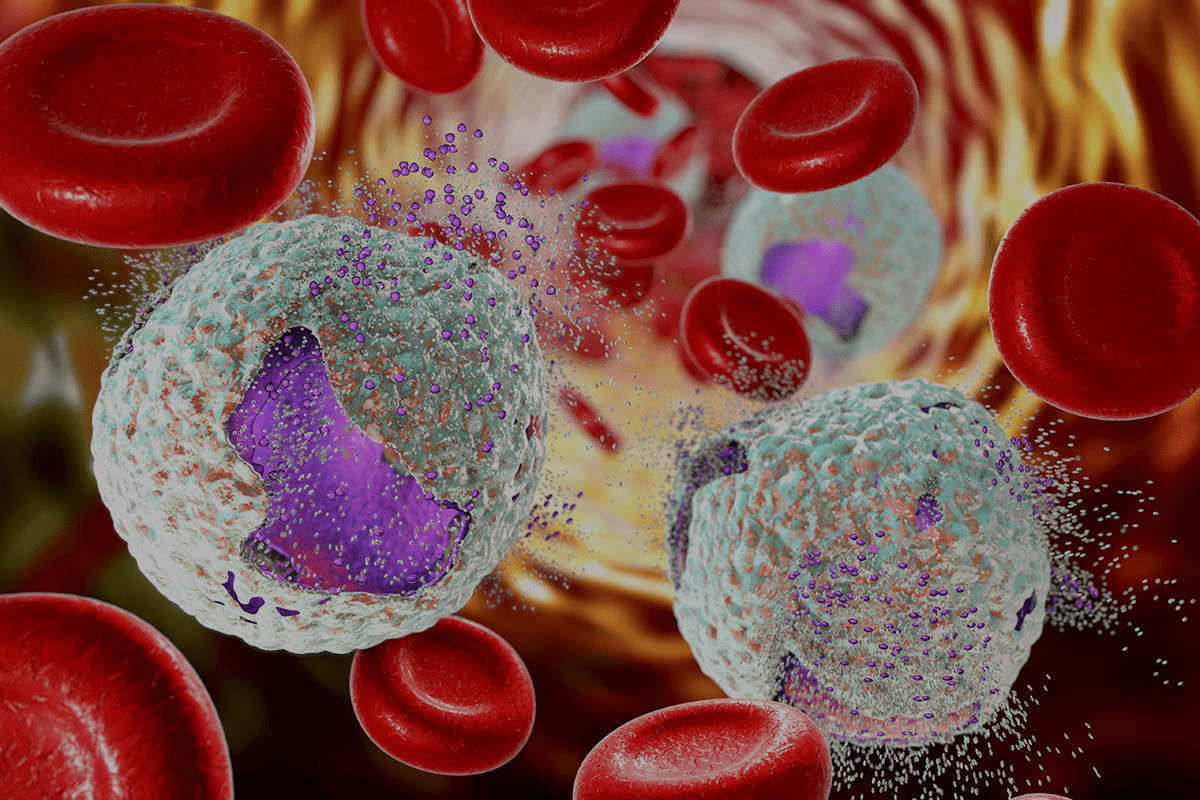
How Sickle Cell Affects Red Blood Cells
In SCD, red blood cells change from disk-shaped to sickle-shaped. This shape change makes it hard for them to move through small blood vessels. This leads to blockages and other issues. The sickled cells also break down easily, causing anemia.
Common Symptoms and Complications
The symptoms and complications of sickle cell disease vary. Common issues include:
- Recurrent episodes of pain due to vaso-occlusive crises
- Anemia resulting from the premature destruction of red blood cells
- Increased susceptibility to infections
- Potential for stroke and other cardiovascular complications
A hematologist,says, “Early diagnosis and care can greatly improve life for those with sickle cell disease.” Knowing the science behind SCD is key to managing and treating it.
White Sickle Cell Disease: Prevalence and Statistics

Sickle cell disease is more common in some ethnic groups. But it also affects white people, though less often. This section will look at how common it is among Caucasians. We’ll explore the current data and what it means.
Current Data on Caucasian Carriers in the US
Recent studies found sickle cell trait in about 1 in 333 white newborns in the US. This shows why it’s key to be aware of and screen for it in Caucasians.
The CDC says sickle cell disease affects 3% to 9% of Hispanics and Latinos. The sickle cell gene is thought to help fight malaria, which is why it’s found in many populations.
The 1 in 333 Statistic: What It Means
The 1 in 333 statistic is important for genetic counseling and family planning. It shows healthcare providers need to know the risk. They should offer the right screening and advice.
This rate means sickle cell disease is a big health issue for Caucasians. It’s not as common as in other groups, but it’s a concern that needs attention.
Hospital Data and Clinical Observations
Hospital data and clinical observations help us understand sickle cell disease in Caucasians. Studies show patients need a lot of care, like pain management and regular checks.
- Early diagnosis and treatment can greatly improve life for those with sickle cell disease.
- Even though it’s less common in Caucasians, the challenges in treating it are similar across ethnic groups.
Can Caucasians Get Sickle Cell Anemia? Debunking Myths
Sickle cell disease can affect anyone, not just certain groups. It’s often linked to people of African descent. But it’s not exclusive to any ethnicity.
Common Misconceptions About Ethnic Distribution
Common Misconceptions
Many think sickle cell disease only affects African or African Americans. But it can happen to anyone, no matter their ethnicity.
- Sickle cell disease is found in individuals of Mediterranean, Middle Eastern, and Indian descent.
- It’s also present in people from Central and South America, mainly those of Hispanic origin.
- The disease is not limited by ethnicity; it’s a genetic condition that can be present in any population.
Recent studies show athat bout 1 in 333 white people in the U.S. carry the sickle cell trait. This shows we need to understand this condition more broadly.
Scientific Evidence of Sickle Cell in White Populations
Research shows sickle cell disease is found in white populations, though less often than in other groups. It’s been found in people of European descent, mainly in Southern Europe and the Mediterranean.
“Sickle cell disease is a global health issue, affecting diverse populations worldwide. It’s vital to recognize that this condition is not limited to any particular ethnic group.”
This research highlights the need to consider sickle cell disease in patients of all ethnicities. It’s not just for those traditionally linked to it.
Understanding Genetic Susceptibility Across Races
The genetic cause of sickle cell disease is a mutation in the HBB gene. This mutation can happen to anyone, no matter their ethnicity.
Genetic susceptibility to sickle cell disease is not race-specific; it’s about inheriting the mutated gene from one’s parents. Knowing this genetic aspect helps identify carriers and manage the disease across different populations.
Genetic testing and counseling are key for families of any ethnicity. They help understand risk and make informed choices.
Genetic Factors Behind Sickle Cell Disease in White People
Sickle cell disease is a genetic condition that affects how the body makes hemoglobin. It can happen to white people, too. This shows we need to look into the genetic reasons behind it.
It’s important to know the genetics of this disease for diagnosis and planning families. The disease comes from changes in the HBB gene. This gene is part of hemoglobin. If someone gets two changedHbSB genes, they get sickle cell disease.
The HBB Gene Mutation in Different Populations
The HBB gene change isn’t just for one group. It’s found in people from many places, like the Mediterranean, the Middle East, and South Asia. In white people, it’s because of old genetic exchanges and migrations.
In some Southern European countries, more people carry the sickle cell trait. This is because malaria was common there. Carrying the trait helped people survive malaria.
Inheritance Patterns and Carrier Status
How genes are passed down affects the chance of sickle cell disease in kids. If both parents carry the trait, there’s a 25% chance their child will have the disease. There’s a 50% chance the child will carry the trait like the parents. And a 25% chance the child won’t have the disease or carry the trait.
| Parent 1 Status | Parent 2 Status | Child’s Chance of Having Sickle Cell Disease | Child’s Chance of Being a Carrier |
| Carrier | Carrier | 25% | 50% |
| Carrier | Not a Carrier | 0% | 50% |
| Not a Carrier | Carrier | 0% | 50% |
Genetic Testing and Family Planning Considerations
Genetic testing can find who carries the sickle cell trait. It’s useful for families with a sickle cell history or for those from high-risk areas. Genetic counseling and testing help with family planning.
“Genetic testing can identify carriers of the sickle cell trait, allowing families to make informed decisions about pregnancy and the management of the condition.”
Knowing if you carry the trait helps families prepare for a child with sickle cell disease. It guides choices about having children.
Historical and Evolutionary Context: The Malaria Connection
The history of sickle cell disease is tied to malaria. This connection has influenced its spread in various populations. Scientists think the sickle cell gene evolved to fight malaria, making it common in areas where malaria is common.
Sickle Cell Trait as Protection Against Malaria
The sickle cell trait helps protect against malaria. This trait is key to understanding why the sickle cell gene is found in some groups.
- In malaria-prone areas, the sickle cell trait helped people survive.
- Those with the trait were more likely to beat malaria.
- This survival benefit led to more sickle cell gene in these groups over time.
Historical Migration Patterns and Gene Distribution
Migration patterns have shaped the spread of the sickle cell gene. Groups moving to or from malaria areas were more likely to carry the gene.
Some migrations that affected sickle cell gene distribution include:
- The trans-Saharan trade and migrations trought populations from malaria-endemic areas into contact with other groups.
- The Mediterranean migrations that affected Southern European populations.
- The movements of people from the Middle East and India into various parts of the world.
Why Southern European and Middle Eastern Whites Have Higher Rates
Southern European and Middle Eastern white populations have higher sickle cell disease rates. This is because they were once exposed to malaria. The sickle cell trait helped protect them.
Key factors contributing to higher rates in these populations include:
- Historical presence of malaria in these regions.
- Genetic legacy from populations that were exposed to malaria.
- Continued presence of the sickle cell gene in these populations due to historical migration patterns.
Understanding these historical and evolutionary factors is key to grasping sickle cell disease’s spread across ethnic groups, including whites.
Diagnosis Challenges for White Patients with Sickle Cell
Diagnosing sickle cell disease in white patients is hard because it’s rare in this group. This rarity can cause delays in diagnosis and wrong treatment. Doctors need to know more about this.
Physician Awareness and Possible Misdiagnosis
Doctors often don’t know much about sickle cell disease in white patients. This is because they think it mainly affects people of African descent. So, white patients might not get tested for it, leading to wrong diagnoses.
Research shows white patients with sickle cell disease often get diagnosed late. This late diagnosis can lead to poor management of symptoms. It’s key for doctors to be aware of sickle cell disease in all patients, not just those of African descent.
Key Factors Contributing to Misdiagnosis:
- Lack of awareness about sickle cell disease among healthcare providers
- Misconceptions about the ethnic distribution of the disease
- Insufficient screening of at-risk populations
Screening Recommendations for At-Risk White Populations
To fix the problem of late diagnosis, we need to screen at-risk white populations better. Newborn screening programs are helping by catching sickle cell disease early. But not all states screen for it, and some at-risk people might not be found at birth.
| Screening Criteria | Recommendations |
| Family History | Screening ris ecommended for individuals with a family history of sickle cell disease or trait |
| Ethnic Background | Consider screening for individuals of Mediterranean, Middle Eastern, or Southern European descent. |
| Symptomatic Individuals | Screening should be considered for individuals presenting with symptoms suggestive of sickle cell disease, regardless of ethnicit.y |
Personal Stories of Diagnostic Journeys
White patients with sickle cell disease share their struggles. Many faced wrong diagnoses before getting the right one. They often had to go through many medical tests.
A young white woman was diagnosed with sickle cell disease after years of pain and anemia. Her story shows the need for doctors to think of sickle cell disease, even in patients not usually at risk.
By sharing these stories, we can raise awareness about the challenges white patients face. This can help improve diagnosis and care for all ethnic groups.
Living with Sickle Cell Disease as a Caucasian
Caucasians with sickle cell disease face unique challenges. They need special care and understanding. It’s important to know that sickle cell disease can affect people of different ethnic backgrounds, including Caucasians.
Unique Social and Medical Challenges
Caucasian individuals with sickle cell disease have to deal with many challenges. Socially, they may face misconceptions about their condition, as it’s less common in this group. This can cause delays in diagnosis and make it hard to find support.
Medically, the challenges are just as big. Doctors might not suspect sickle cell disease in Caucasian patients, leading to misdiagnosis or delayed diagnosis. A study in the American Journal of Hematology found that delays in diagnosis can lead to worse disease management and more complications.
“The lack of awareness about sickle cell disease in non-African populations can lead to significant delays in diagnosis and treatment, affecting patient outcomes.”
Support Resources and Community Connections
Despite these challenges, there are many support resources for Caucasian individuals with sickle cell disease. Connecting with community organizations and support groups can offer emotional support and practical advice for managing the condition.
- National Sickle Cell Disease Association (NSCD)
- Sickle Cell Disease Foundation of America
- Local support groups and online forums
These resources help individuals and families deal with the complexities of sickle cell disease. They provide guidance on treatment options, pain management, and lifestyle adjustments.
Managing the Condition Effectively
Managing sickle cell disease effectively requires a complete approach. This includes hydroxyurea therapy, blood transfusions, and pain management strategies. Regular check-ups with healthcare professionals are key to preventing and managing complications.
“Advances in medical care have greatly improved the lives of those with sickle cell disease,” says a hematologist specializing in sickle cell disease. “With the right management, patients can live active and fulfilling lives.”
By understanding the unique challenges and using available support resources, Caucasian individuals with sickle cell disease can manage their condition better. This improves their quality of life.
Treatment Options and Medical Management
Managing sickle cell disease requires a mix of old and new treatments. It’s about using a wide range of strategies to tackle the disease from all sides.
Standard Treatment Protocols
Doctors use medicines like hydroxyurea to help patients. It makes painful crises less common and might cut down on blood transfusions. Blood transfusions are key too, as they lower the risk of serious problems by reducing sickled red blood cells.
We also have special pain plans for each patient. These can be simple pain relievers or stronger meds, based on how bad the pain is. Drinking plenty of water and managing stress are also big parts of care.
Key components of standard treatment protocols include:
- Hydroxyurea therapy
- Regular blood transfusions
- Pain management medications
- Hydration and stress management
Emerging Therapies and Research
New treatments bring hope to those with sickle cell disease. Gene therapy tries to fix the genetic problem at the source. Other research focuses on new meds to ease symptoms or prevent problems.
One big hope is for treatments that could cure the disease, like bone marrow transplants. These are risky but could cure some patients. Scientists are working hard to make these treatments safer and more available.
“Gene therapy has the power to change sickle cell disease treatment by fixing the cause of the disease.”
Specialized Care Considerations
Getting the right care is ketoor sickle cell disease. This means regular check-ups with experts and access to support services.
It’s very important for people with sickle cell, like Caucasians, to see doctors who know the disease well. This ensures they get care that fits their unique needs.
Considerations for specialized care include:
- Regular monitoring by specialists
- Access to complete support services
- Care tailored for different patient groups
Conclusion: Understanding Sickle Cell Disease Across All Ethnicities
Sickle cell disease is often seen as a problem mainly for people of African descent. But we’ve found it can happen to anyone, including Caucasians. It’s important to know about white sickle cell disease, even if it’s not as common.
It’s clear now that Caucasians can get sickle cell anemia. It’s rare, but it’s a fact. The disease is caused by a specific gene, not just by race.
Knowing that anyone can get sickle cell disease is key to early treatment. We need more genetic testing and awareness among doctors. This way, everyone, no matter their race, can get the right care.
By recognizing sickle cell disease in all ethnic groups, we can help more people. This approach is essential for better understanding and treating the disease.
FAQ
Can Caucasians get sickle cell anemia?
Yes, Caucasians can get sickle cell anemia. It’s less common in them than in people of African descent.
How common is sickle cell disease in white people?
Sickle cell disease is rare in white people. But it does happen. The rate varies in different groups due to genetics and history.
What are the genetic factors behind sickle cell disease in white people?
The HBB gene mutation causes sickle cell disease in all ethnic groups, including whites. How it’s passed down affects the risk of it being passed to children.
Can a white person have sickle cell disease?
Yes, a white person can have sickle cell disease. It’s not as common, but it’s not limited to any group.
Do white people get sickle cell anemia?
Yes, white people can get sickle cell anemia. It’s important to remember that sickle cell disease isn’t just found in certain groups.
What is the significance of the 1 in 333 statistic regarding sickle cell trait in Caucasians?
The 1 in 333 statistic shows that about 1 in 333 Caucasians carry the sickle cell trait. This highlights the need for awareness and genetic testing.
Are there unique challenges faced by Caucasians living with sickle cell disease?
Yes, Caucasians with sickle cell disease face special challenges. These include delayed diagnosis and not enough awareness among doctors.
What are the treatment options for sickle cell disease, and are they the same for all ethnicities?
Treatments for sickle cell disease are the same for everyone. They aim to manage symptoms, prevent problems, and explore new therapies.
How does sickle cell disease affect red blood cells?
Sickle cell disease makes red blood cells misshapen and breaks them down. This leads to anemia, pain, and other issues.
Is genetic testing recommended for family planning in cases of sickle cell disease?
Yes, genetic testing is advised for family planning. It helps find out if someone is a carrier and the risk of passing the disease to children.
Can whites get sickle cell disease if they have no African ancestry?
Yes, whites can get sickle cell disease even without African ancestry. This is due to history and genetics.
What is the historical context of sickle cell disease in relation to malaria?
Sickle cell trait offered some protection against malaria. This is why it’s more common in areas where malaria was once widespread.
Reference
- National Heart, Lung, and Blood Institute (NHLBI) – Sickle Cell Disease Fact Sheet