Last Updated on November 20, 2025 by Ugurkan Demir
Getting the right diagnosis of sickle cell disease is key for good care. Sickle cell disease causes problems like pain and damage to organs. It happens because of blood cells that don’t move right.
Differential diagnosis for sickle cell this disease is tricky because its signs can look like other illnesses. At Liv Hospital, we focus on making sure we get it right. We use careful steps and put our patients first.
Key Takeaways
- Understanding the clinical manifestations of sickle cell disease is vital for precise diagnosis.
- Laboratory features play a critical role in distinguishing sickle cell disease from similar conditions.
- Effective management relies on accurate and timely diagnosis.
- Differential diagnosis requires a comprehensive approach.
- Patient-centered care is essential for managing sickle cell disease.
Understanding Sickle Cell Disease Pathophysiology

It’s important to know how sickle cell disease works to treat it well. This disease is caused by a genetic problem that affects hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen.
Molecular Basis of Hemoglobin S (HbS)
The main cause of sickle cell disease is a genetic mutation. This mutation leads to abnormal hemoglobin, called Hemoglobin S (HbS). The mutation happens in the HBB gene, which tells our bodies how to make a part of hemoglobin.
The change from glutamic acid to valine at the sixth position of the beta-globin chain creates HbS. This can cause red blood cells to change shape under low oxygen, leading to sickle cells.
Finding HbS is key to diagnosing sickle cell disease. Laboratory diagnosis of sickle cell disease often uses tests like hemoglobin electrophoresis to find and measure HbS.
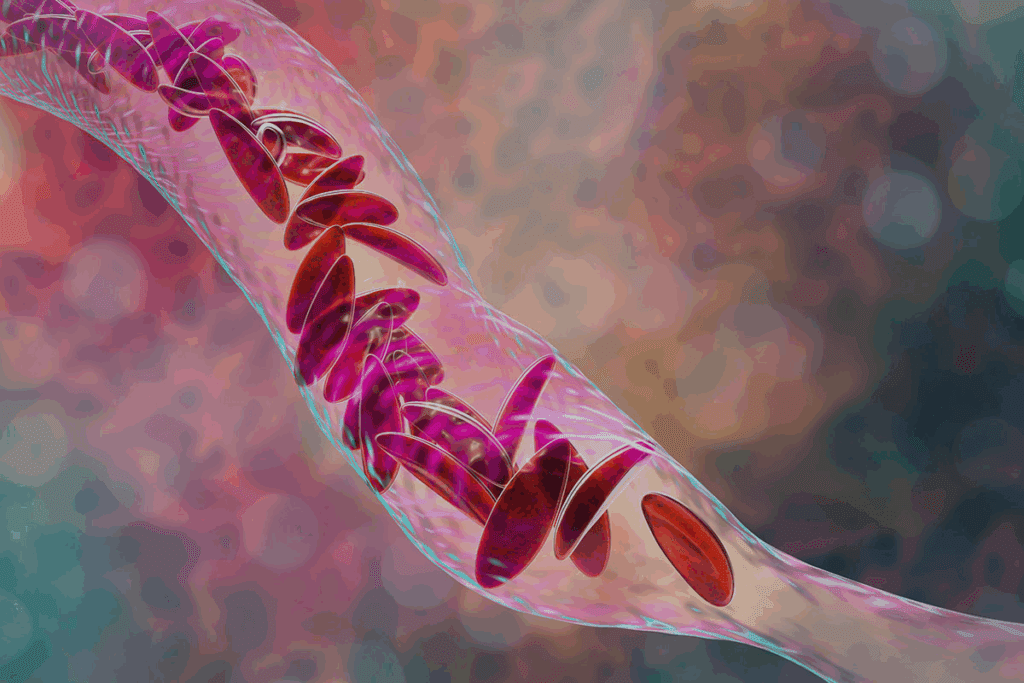
Mechanism of Sickling and Vaso-occlusion
When HbS polymerizes, red blood cells become stiff and sickle-shaped. This happens more often in low oxygen, acid, and dehydration. Sickled cells can break down easily and block small blood vessels, causing vaso-occlusion.
Vaso-occlusion is a major problem in sickle cell disease. It leads to sudden pain and can damage organs over time.
- Increased adhesion of sickled red blood cells to the endothelium
- Activation of various cellular and molecular pathways that promote vaso-occlusion
- Release of inflammatory mediators that further exacerbate the condition
Genetic Inheritance Patterns in Sickle Cell Disease
Sickle cell disease is passed down in an autosomal recessive pattern. This means you need two defective HBB genes, one from each parent, to have the disease. Carriers of the sickle cell trait, with one normal and one defective HBB gene, usually don’t show symptoms but can pass the mutated gene to their kids.
“Understanding the genetic basis of sickle cell disease is essential for genetic counseling and for predicting the risk of transmission to future generations.”
The chance of having a child with sickle cell disease depends on the parents’ genotypes. If both parents are carriers, there’s a 25% chance with each pregnancy of having a sickle cell disease child.
Clinical Manifestations That Guide Sickle Cell Disease Diagnosis
Sickle cell disease (SCD) shows many symptoms, making diagnosis tricky but key for treatment. Each patient’s symptoms can be different, which makes it hard to diagnose but very important.
Acute Pain Crisis Presentations
Acute pain crises, or vaso-occlusive crises, are a big sign of SCD. They happen when sickled red blood cells block blood vessels. This causes pain and is why people often go to the doctor.
A study in the Journal of Pain Research says managing these crises is complex. It needs medicine and support.
- Pain crises can start from dehydration, infections, or extreme weather.
- The pain’s severity and how often it happens can differ a lot between people.
- Managing pain well is key to improving life quality for those with SCD.
Chronic Complications and Organ Damage
SCD leads to long-term problems and damage to organs. This is because of repeated blockages and breakdown of red blood cells. Common issues include chronic anemia, spleen problems, and a higher risk of infections.
| Complication | Description | Clinical Impact |
| Chronic Anemia | Long-lasting low red blood cell count or hemoglobin. | Feeling tired, weak, and short of breath. |
| Splenic Sequestration | Blood suddenly pools in the spleen, causing severe anemia. | Can be life-threatening if not treated quickly. |
| Increased Infection Risk | Asplenia and immune issues. | More likely to get infections from certain bacteria. |
Age-Related Presentation Differences
SCD symptoms change with age. Babies and young kids show different signs than adults. For example, hand-foot syndrome is common in young children.
“The clinical presentation of SCD evolves with age, necessitating age-specific management strategies.”
Hematologist
Knowing these age differences is key for early diagnosis and right treatment in all age groups.
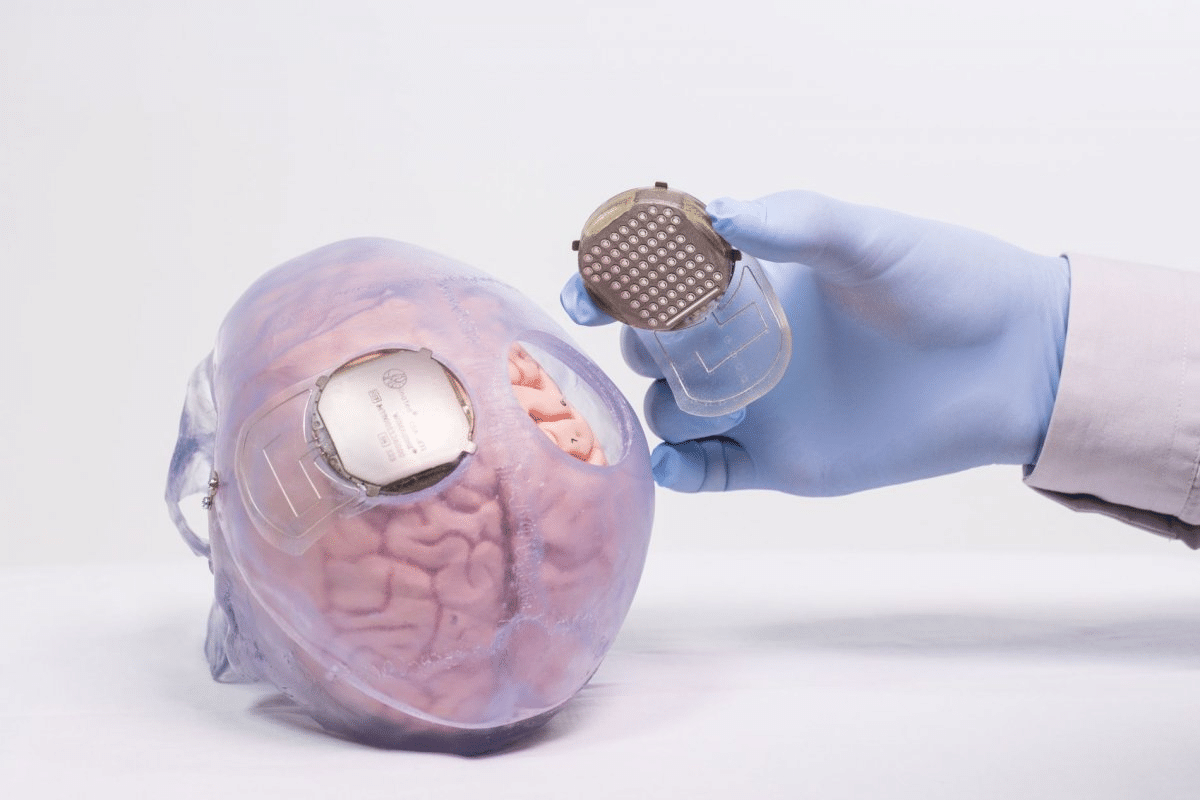
Laboratory Diagnosis of Sickle Cell Anemia
Diagnosing sickle cell anemia involves several lab tests. These tests help find the abnormal hemoglobin S. We will look at the main tests used to diagnose sickle cell anemia.
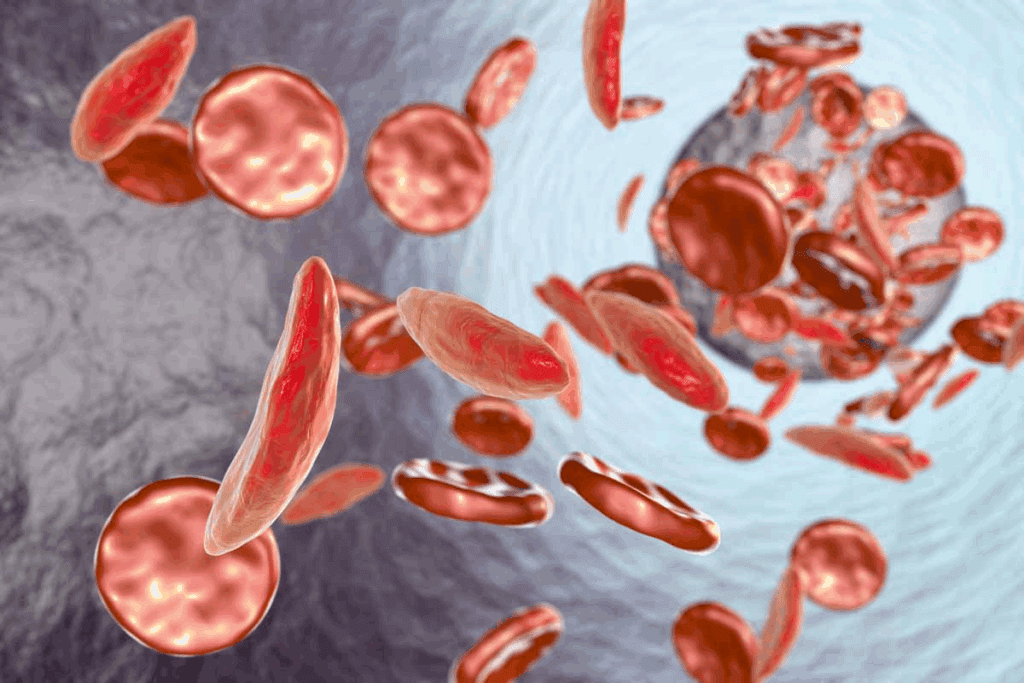
Complete Blood Count and Hemolysis Markers
A complete blood count (CBC) is often the first test for sickle cell disease. It shows anemia and other issues like too many white blood cells. Tests like lactate dehydrogenase (LDH) and indirect bilirubin show red blood cell damage.
Sickle Cell Disease Peripheral Smear Findings
Looking at the peripheral blood smear is key. It shows sickle-shaped red blood cells, target cells, and Howell-Jolly bodies
Reticulocyte Count and Bilirubin Levels
The reticulocyte count is high in sickle cell disease. It shows the bone marrow is working hard to replace lost red blood cells. Bilirubin levels, like indirect bilirubin, also go up due to red blood cell breakdown. These tests help understand how severe the disease is.
Hemoglobin Electrophoresis in Sickle Cell Disease Diagnosis
Hemoglobin electrophoresis is a key tool in diagnosing sickle cell disease. It helps identify and measure different hemoglobin types, like Hemoglobin S (HbS). HbS is the main cause of sickle cell disease.
Interpreting Sickle Cell Disease Electrophoresis Results
Understanding hemoglobin electrophoresis results is vital for sickle cell disease diagnosis. This method separates hemoglobin types by charge. In sickle cell disease, HbS is the main type found.
We check for HbS and other hemoglobins like HbA, HbF, and others. This helps us see how much HbS is present.
Key findings in sickle cell disease electrophoresis include:
- Presence of HbS
- Quantity of HbS relative to other hemoglobins
- Presence of other hemoglobin variants
Quantification of HbS and Other Hemoglobin Variants
Measuring HbS and other hemoglobin types is key for sickle cell disease diagnosis. The amount of HbS can affect how severe the disease is.
| Hemoglobin Variant | Normal Percentage | Sickle Cell Disease Percentage |
| HbA | 95-98% | 0% |
| HbS | 0% | 80-90% |
| HbF | Variable, often increased |
High-Performance Liquid Chromatography Alternatives
Hemoglobin electrophoresis is a traditional method for diagnosing sickle cell disease. High-performance liquid chromatography (HPLC) is an alternative that offers precise measurements of hemoglobin types. HPLC is great for finding and measuring small amounts of hemoglobin.
We use these methods to accurately diagnose and treat sickle cell disease. Knowing the strengths and weaknesses of each method is important for good patient care.
Differential Diagnosis for Sickle Cell vs. Other Hemoglobinopathies
Diagnosing sickle cell disease means figuring out if it’s different from other blood disorders. Sickle cell disease (SCD) is a group of disorders with at least one abnormal hemoglobin S allele. It’s important to tell it apart from thalassemia, autoimmune hemolytic anemia, and other blood disorders.
Distinguishing HbS from Other Hemoglobin Variants
One big challenge in diagnosing SCD is telling Hemoglobin S (HbS) apart from other abnormal hemoglobins. HbS causes red blood cells to sickle. Other variants like Hemoglobin C (HbC) and Hemoglobin E (HbE) can also cause anemia but are different.
Lab tests like hemoglobin electrophoresis and high-performance liquid chromatography (HPLC) are key. They help find and measure different hemoglobin types. This helps doctors accurately diagnose SCD.
Compound Heterozygous Sickle Cell States
Compound heterozygous states happen when someone has two different mutant alleles, one being HbS. For example, HbS/HbC disease and HbS/β-thalassemia. These conditions can be hard to diagnose because they vary in severity.
- HbS/HbC disease can cause severe anemia and crises, like homozygous SCD.
- HbS/β-thalassemia’s severity depends on the β-thalassemia mutation and normal β-globin production.
Diagnostic Challenges in Mixed Hemoglobinopathies
Mixed hemoglobinopathies, like HbS with other variants, are tough to diagnose. Having multiple variants makes lab results hard to interpret. This often needs careful analysis and extra tests.
Key diagnostic considerations include:
- Clinical presentation and family history.
- Laboratory findings, including complete blood count, reticulocyte count, and hemoglobin electrophoresis.
- Molecular testing to identify specific mutations.
By using clinical evaluation and advanced lab tests, doctors can accurately diagnose SCD. This ensures the right treatment and management for patients.
Sickle Cell Disease vs. Thalassemia Syndromes
Understanding the differences between sickle cell disease and thalassemia is key. Both are genetic disorders that affect how the body makes hemoglobin. Yet, they show different symptoms and lab results.
Clinical Distinction Between SCD and Thalassemias
Sickle cell disease (SCD) is caused by hemoglobin S (HbS). It leads to painful crises and anemia. Thalassemia, on the other hand, is due to a lack of globin chains. This causes severe anemia and other issues.
SCD is marked by sudden pain and long-term organ damage. Thalassemia major, by contrast, needs frequent blood transfusions because of severe anemia.
SCD patients often have a history of pain and organ problems. Thalassemia patients might grow slowly and have bone issues due to their marrow.
Laboratory Parameters for Differentiation
Lab tests are vital in telling SCD apart from thalassemia. Complete Blood Count (CBC) and hemoglobin electrophoresis are key. SCD shows anemia and high reticulocytes on CBC, with HbS on electrophoresis. Thalassemia has small, pale red cells and high HbF and/or HbA2 on electrophoresis.
We use these tests to spot the difference. For example, SCD patients have a lot of HbS, while thalassemia patients have more HbF.
HbS-Beta-Thalassemia: A Diagnostic Challenge
HbS-beta-thalassemia is a mix of SCD and beta-thalassemia. It’s hard to diagnose because of its complex genetics and symptoms. Patients can have mild to severe anemia and pain crises.
We identify HbS-beta-thalassemia through hemoglobin electrophoresis. It shows HbS and high HbF or HbA2. The severity can vary, so close monitoring is needed.
Differentiating Sickle Cell Disease vs. Sickle Cell Trait
It’s important to know the difference between Sickle Cell Disease and Sickle Cell Trait. This helps in giving the right medical care and advice on genetics. People with Sickle Cell Trait are usually healthy. But those with Sickle Cell Disease face serious health problems.
Hematological Differences Between Trait and Disease
Sickle Cell Disease happens when red blood cells have hemoglobin S (HbS). This causes them to sickle under certain conditions. On the other hand, Sickle Cell Trait has one normal and one abnormal HBB gene. This means they have both normal hemoglobin (HbA) and HbS.
The main differences in blood include:
- Hemoglobin Levels: People with Sickle Cell Disease often have less hemoglobin because of constant breakdown. Those with Sickle Cell Trait usually have normal hemoglobin levels.
- Peripheral Smear: Sickle Cell Disease shows sickle-shaped red blood cells. Sickle Cell Trait shows normal red blood cells.
- Reticulocyte Count: Sickle Cell Disease has high reticulocyte counts due to constant breakdown. Sickle Cell Trait has a normal count.
Clinical Manifestations in Trait vs. Disease
People with Sickle Cell Trait are usually fine but might face issues in extreme situations. Sickle Cell Disease, on the other hand, leads to frequent pain, more infections, and chronic problems.
Key differences in symptoms include:
- Pain Crises: Sickle Cell Disease has frequent pain crises, while Sickle Cell Trait rarely does.
- Infection Risk: Sickle Cell Disease increases the risk of infections because of asplenia.
- Organ Damage: Sickle Cell Disease often causes organ damage, but Sickle Cell Trait does not.
Genetic Counseling Considerations
Genetic counseling is key for those with Sickle Cell Trait, mainly when planning families. It’s important to know the chances of passing Sickle Cell Disease to children.
Genetic counseling focuses on:
| Genotype of Parents | Risk of Sickle Cell Disease in Offspring |
| Both parents have Sickle Cell Trait | 25% chance of Sickle Cell Disease |
| One parent has Sickle Cell Trait, the other has Sickle Cell Disease | 50% chance of Sickle Cell Disease |
Healthcare providers can give better care and advice by understanding these differences and risks.
Distinguishing Sickle Cell Disease from Autoimmune Hemolytic Anemia and Leukemias
It’s important to tell Sickle Cell Disease (SCD) apart from other blood disorders like Autoimmune Hemolytic Anemia (AIHA) and leukemias. SCD is caused by abnormal hemoglobin, making red blood cells sickle. AIHA happens when the body attacks its own red blood cells. Leukemias are cancers of the blood or bone marrow.
Comparing Hemolytic Parameters
Looking at hemolytic parameters helps tell SCD, AIHA, and leukemias apart. These include lactate dehydrogenase (LDH) levels, reticulocyte count, and bilirubin levels. SCD shows high levels of these because of constant blood cell breakdown. AIHA also has high LDH and reticulocyte count due to immune system attacks. Leukemias can have different levels based on how much the bone marrow is affected.
| Disease | LDH Levels | Reticulocyte Count | Bilirubin Levels |
| SCD | Elevated | Elevated | Elevated |
| AIHA | Elevated | Elevated | Variable |
| Leukemias | Variable | Variable | Variable |
Bone Marrow Examination Findings
Bone marrow tests are key in telling SCD, AIHA, and leukemias apart. SCD shows more red blood cell production in the bone marrow. AIHA also has more red blood cell production but has autoimmune antibodies. Leukemias have cancer cells in the bone marrow, seen through tests.
Immunological Testing and Flow Cytometry
Immunological tests and flow cytometry help diagnose SCD, AIHA, and leukemias. The Direct Coombs test is positive in AIHA, showing antibodies on red blood cells. Flow cytometry is great for finding specific markers in leukemias. SCD doesn’t need these tests for diagnosis but they help rule out other conditions.
By using clinical checks and lab tests, doctors can accurately diagnose SCD, AIHA, and leukemias. This ensures the right treatment and care for each patient.
Homozygous SS Disease vs. Heterozygous SC Disease Comparison
It’s important to know the difference between homozygous SS disease and heterozygous SC disease. Both are types of sickle cell disease (SCD), but they have different symptoms and lab results.
Clinical Severity and Symptom Differences
Homozygous SS disease, or sickle cell anemia, is more serious than SC disease. People with SS disease have more and worse sickle cell crises, anemia, and organ damage. SC disease is milder, but it can cause problems like spleen issues and more infections.
SS disease is caused by two bad hemoglobin S genes. This means more HbS and worse sickling. SC disease, with one HbS and one HbC gene, is less severe.
Laboratory Findings in SS vs. SC Disease
Lab tests help tell SS and SC disease apart. The main differences are in hemoglobin electrophoresis, blood counts, and smear results.
| Laboratory Parameter | Homozygous SS Disease | Heterozygous SC Disease |
| Hemoglobin Electrophoresis | Predominantly HbS, variable HbF | HbS and HbC present, less HbF |
| Hemoglobin Level | Typically lower (around 6-8 g/dL) | Mildly reduced or normal |
| Peripheral Smear | More sickled cells, target cells, and nucleated RBCs | Fewer sickled cells, more target cells |
Treatment Approach Variations
SS and SC disease need different treatments. SS disease needs more aggressive care, like blood transfusions and hydroxyurea. SC disease might need less treatment, focusing on easing symptoms and preventing problems.
Key differences in treatment approaches include:
- Frequency and necessity of blood transfusions
- Use of hydroxyurea and other disease-modifying therapies
- Intensity of pain management strategies
Healthcare providers must understand these differences to give better care and improve patient outcomes.
Conclusion: Integrated Approach to Sickle Cell Disease Diagnosis
Getting sickle cell disease right is key for better care and outcomes. We’ve talked about how to tell it apart from other diseases. This includes looking at symptoms, lab tests, and genetics.
Diagnosing SCD means checking how the body works, doing blood tests, and looking at genes. This mix helps doctors get it right, making sure it’s not mistaken for other diseases.
This way of diagnosing helps doctors make plans just for each patient. It’s all about giving the best care possible and making life better for those with the disease.
Using this detailed method helps us understand sickle cell disease better. It also means we can give better care to patients all over the world.
FAQ
What is the primary method used to diagnose sickle cell disease?
Hemoglobin electrophoresis is the main way to diagnose sickle cell disease. It spots and measures different hemoglobin types, including HbS.
How does sickle cell disease differ from sickle cell trait?
Sickle cell disease happens when a person has two abnormal hemoglobin genes, making HbS. Sickle cell trait is when a person has one normal and one abnormal gene, leading to a milder form.
What are the clinical manifestations that guide the diagnosis of sickle cell disease?
Signs like pain crises and chronic issues help diagnose sickle cell disease. These symptoms change with age and vary in severity.
How is sickle cell disease distinguished from thalassemia syndromes?
Sickle cell disease is told apart from thalassemia by clinical and lab tests. Tests like hemoglobin electrophoresis and genetic tests show the specific hemoglobin types and mutations.
What laboratory tests are used to diagnose sickle cell anemia?
Tests for sickle cell anemia include hemoglobin electrophoresis and a reticulocyte count. These tests show the disease’s presence and how severe it is.
What is the difference between homozygous SS disease and heterozygous SC disease?
Homozygous SS disease is more severe, with two HbS genes. Heterozygous SC disease is milder, with one HbS and one HbC gene.
How is sickle cell disease diagnosed in infants and young children?
Newborn screening programs use tests like hemoglobin electrophoresis to spot sickle cell disease in babies and young kids.
What is the role of genetic counseling in sickle cell disease?
Genetic counseling is key for sickle cell disease, mainly for those with sickle cell trait. It informs about passing the condition to future generations and aids in family planning.
How is sickle cell disease distinguished from autoimmune hemolytic anemia and leukemias?
Sickle cell disease is differentiated from other conditions through tests like bone marrow exams and immunological tests. These help find the cause of anemia and other symptoms.
What is the significance of quantifying HbS and other hemoglobin variants in sickle cell disease diagnosis?
Measuring HbS and other hemoglobin types is vital in diagnosing sickle cell disease. It shows how severe the disease is, guides treatment, and checks if therapy is working.
References
- National Heart, Lung, and Blood Institute. (2022). Evidence-based management of sickle cell disease: Expert panel report (EPR). National Institutes of Health. https://www.nhlbi.nih.gov/health-topics/evidence-based-management-sickle-cell-disease