Last Updated on November 26, 2025 by Bilal Hasdemir

Modern medicine has changed how we diagnose and treat heart disease. Techniques like angiography procedure and stent placement are key. At Liv Hospital, we focus on patient trust and safety. We make sure every procedure is done with care and precision.
Angiography is not traditional surgery. It’s a minimally invasive method using imaging and catheters. A coronary angiogram spots blockages in coronary arteries. X-ray images help doctors decide on treatment.
Key Takeaways
- Angiography is a minimally invasive procedure, not traditional surgery.
- It helps diagnose and treat blood vessel conditions.
- Coronary angiogram identifies blockages in coronary arteries.
- X-ray images guide treatment decisions.
- Liv Hospital prioritizes patient trust and safety.
Understanding Angiography: Is Angiography Surgery?

Angiography is a medical imaging technique that lets doctors see inside blood vessels. It helps diagnose vascular diseases. This tool is key for planning treatments for heart and blood vessel problems.
Definition and Purpose of Angiography
Angiography involves putting a catheter into an artery. It’s guided to the heart or other vessels. Then, a contrast dye is injected to show blood vessels on X-ray images.
This helps doctors spot blockages, aneurysms, or other issues. The main goal is to get clear images of blood vessels. This helps in making accurate diagnoses and treatment plans.
We use angiography to check blood vessel health and find the best treatment. It’s great for diagnosing heart and blood vessel diseases. It helps us decide if a patient needs angioplasty, stenting, or other treatments.
Differentiating Angiography from Traditional Surgery
Angiography is an invasive procedure but not traditional surgery. It doesn’t need big cuts like surgery does. Instead, it uses a small skin puncture for the catheter.
This approach cuts down recovery time and lowers risks. Angioplasty, often done with angiography, uses a balloon to widen narrowed arteries. This improves blood flow.
We see angiography as different from traditional surgery because it’s less invasive. It doesn’t remove or repair tissues. Instead, it focuses on seeing the vascular system and treating blockages or narrowing. This is important for patients to know what to expect and how to recover.
Common Conditions Requiring Angiography and Stent Placement
Many vascular conditions affect heart health, leading to the need for angiography and stent placement. Angiography lets doctors see inside blood vessels. This helps find blockages or abnormalities. Stent placement then helps restore normal blood flow.
Coronary Artery Disease and Atherosclerosis
Coronary artery disease (CAD) happens when plaque builds up in coronary arteries. This buildup, known as atherosclerosis, can narrow arteries. Narrowed arteries reduce blood flow to the heart. Doctors use angiography to see how bad CAD is and if stents are needed.
The American Heart Association says CAD is a top cause of death globally. “Coronary artery disease is when the heart’s main blood vessels get damaged or diseased,” the AHA reports. “It’s mainly caused by atherosclerosis, where plaque builds up in arteries.”
Other Vascular Conditions Requiring Intervention
Other vascular conditions also need angiography and stent placement. These include peripheral artery disease (PAD) and carotid artery disease. PAD affects arteries outside the heart, while carotid artery disease affects brain-supplying arteries.
| Condition | Description | Treatment |
| Coronary Artery Disease (CAD) | Buildup of plaque in coronary arteries | Angiography, Stent Placement |
| Peripheral Artery Disease (PAD) | Blockages in arteries outside the heart | Angiography, Stent Placement |
| Carotid Artery Disease | Narrowing of arteries supplying blood to the brain | Angiography, Possible Stenting |
It’s important for patients to know about these conditions and treatments. Angiography is key in diagnosing these issues. Stent placement is often a major part of treatment.
Preparing for Your Angiography Procedure
We’ll help you get ready for your angiography. This includes the steps you need to take before the procedure. These steps are important for a smooth and successful angiography.
Pre-Procedure Testing and Evaluation
You’ll have tests before your angiography to check your health and blood vessels. These might include blood work, ECGs, and imaging like chest X-rays or echocardiograms. These tests help your healthcare team understand your blood vessel condition.
You’ll also need to share your medical history. This includes any allergies, past surgeries, or current medications. This info is key for planning your angiography safely and effectively.
Medication Adjustments and Fasting Requirements
Your doctor might ask you to stop or adjust some medications before the procedure. This includes blood thinners to reduce bleeding risks. It’s very important to follow these instructions for your safety.
You might need to fast from midnight the night before. This is to avoid complications with anesthesia. Your healthcare team will give you specific fasting and pre-procedure instructions.
By following these instructions and completing the necessary tests, you can make sure your angiography goes well. And you’ll recover smoothly.
The Angiography Procedure: Step by Step
Let’s walk through the angiography procedure step by step. You’ll understand what to expect. This test is key for seeing inside blood vessels and organs, like the coronary arteries.
Patient Preparation and Sedation
The test happens in a special lab with advanced imaging tools. We keep a close eye on the patient’s health.
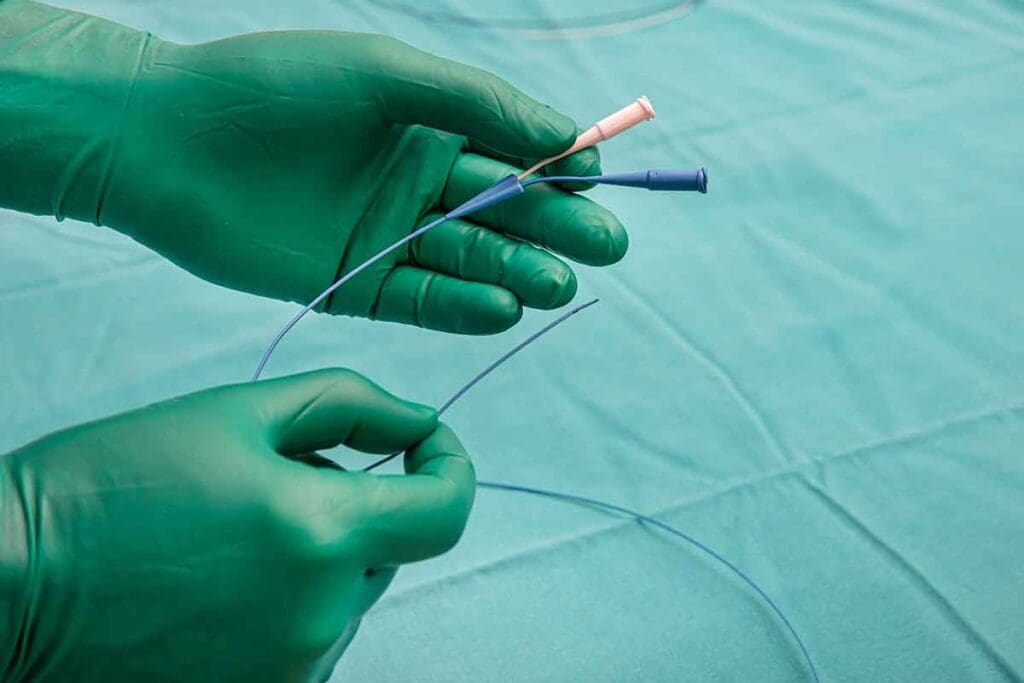
Catheter Insertion Techniques
Inserting a catheter into an artery is a key step. We use a method called percutaneous access, making a small skin puncture. Then, we guide the catheter to the coronary arteries with live images.
Catheter insertion has improved a lot, making procedures safer and more precise. Whether to use radial or femoral access depends on the patient and the doctor’s choice.
Contrast Dye Administration and Imaging
With the catheter in, we give contrast dye to see the coronary arteries. The dye makes the blood vessels stand out on the screen, helping us spot problems.
Getting the dye right is key for a good diagnosis. We use a special injector for safe and controlled dye delivery.
As the dye moves through the arteries, we take detailed pictures with a fluoroscopy system. These pictures help us see how much vascular disease there is.
A study in the Journal of the American College of Cardiology says, “Coronary angiography is the best way to find coronary artery disease.” Our team uses the best methods for accurate results.
Understanding Heart Stents: Types and Functions
Heart stents are key in fighting coronary artery disease. They act as a scaffold to keep arteries open. These small, metal mesh tubes are used during angioplasty to ensure the artery stays open. This helps improve blood flow to the heart.
There are many types of heart stents, each with its own benefits. Knowing these differences is important for both patients and healthcare providers. It helps them choose the best treatment option.
Bare Metal Stents vs. Drug-Eluting Stents
Bare metal stents (BMS) and drug-eluting stents (DES) are the most used stents. Bare metal stents are made of metal mesh to support the artery. On the other hand, drug-eluting stents have a drug coating that releases over time. This helps prevent the artery from narrowing again.
| Characteristics | Bare Metal Stents (BMS) | Drug-Eluting Stents (DES) |
| Material | Metal mesh | Metal mesh with drug coating |
| Re-narrowing Rate | Higher | Lower |
| Medication | No | Yes, released over time |
Biodegradable Stents and Future Technologies
Biodegradable stents, or bioresorbable stents, are a new type. They dissolve over time. Made from materials that the body absorbs, they might reduce long-term complications of metal stents.
Future stent technologies aim to improve safety and outcomes. Advances in materials and drug delivery systems will shape the next stent generation.
Angioplasty and Stent Placement Procedure
The angioplasty process uses a balloon to widen blocked arteries. Then, a stent is placed to keep the artery open. This method is key in treating heart disease and other vascular issues.
Balloon Angioplasty Technique
Balloon angioplasty widens narrowed or blocked arteries. A catheter with a deflated balloon is inserted into the artery. Once in place, the balloon is inflated to push the plaque against the artery walls, improving blood flow.
Key Steps in Balloon Angioplasty:
- Insertion of a catheter with a balloon into the artery
- Guiding the catheter to the blockage site using imaging techniques
- Inflating the balloon to widen the artery
- Deflating the balloon and removing the catheter
Stent Deployment Process
After angioplasty, a stent is placed to keep the artery open. The stent is a small, mesh-like tube that fits over the blockage. There are various stents, like bare metal and drug-eluting stents, each with its own advantages.
Types of Stents:
| Stent Type | Description | Benefits |
| Bare Metal Stents | Simple metal mesh stents | Less risk of long-term complications |
| Drug-Eluting Stents | Stents coated with medication | Reduces risk of restenosis |
Confirming Proper Placement
After the stent is deployed, imaging is used to check its position and blood flow. This step is vital to ensure the procedure’s success and to lower the risk of complications.
By combining balloon angioplasty with stent placement, we can effectively restore blood flow to the heart. This reduces symptoms and improves life quality for those with heart disease.
Recovery After Angiography and Stent Placement
Knowing what to expect after angiography and stent placement can make recovery easier. This time is key and needs careful attention and following medical advice.
Immediate Post-Procedure Care
Right after the procedure, we watch your vital signs and the access site for any problems. It’s common to stay under observation for a few hours to check for bleeding or other vascular issues.
During this time, you might need to:
- Stay calm and avoid hard activities
- Keep the access site dry
- Follow specific instructions about medication and follow-up care
Differences Between Femoral and Radial Access Recovery
The access site affects your recovery. Femoral access from the groin area might keep you lying flat for hours to avoid bleeding. On the other hand, radial access from the wrist lets you move around sooner and leave the hospital faster.
| Recovery Aspect | Femoral Access | Radial Access |
| Bed Rest | Several hours | Minimal to none |
| Mobility | Limited initially | Generally unrestricted |
Hospital Discharge and Home Care Instructions
Before you go home, we give you detailed care instructions. This includes:
- Keeping the access site clean and dry
- Watching for signs of infection or complications
- Following your medication schedule
- Avoiding heavy lifting or hard activities for a while
It’s also important to keep your follow-up appointments. This helps ensure you’re healing right and can address any worries.
By following these guidelines and talking openly with your healthcare team, you can smoothly go through recovery. This way, you can avoid or lessen any complications.
Potential Risks and Complications
It’s important to know the risks of angiography and stent placement. These procedures are usually safe but can have complications. Being informed helps make better choices.
Procedure-Related Complications
Complications can happen during or after these procedures. Some include:
- Bleeding or hematoma at the catheter insertion site
- Allergic reactions to the contrast dye used during the procedure
- Damage to blood vessels, including dissection or perforation
- Renal complications, mainly in those with kidney disease
Complication rates depend on the patient and the procedure. Studies show a low complication rate, usually 1-5%.
| Complication Type | Frequency | Risk Factors |
| Bleeding or Hematoma | 1-3% | Anticoagulant use, larger catheter size |
| Allergic Reaction to Contrast | 0.5-2% | History of allergies, previous contrast reaction |
| Vascular Damage | 0.5-1.5% | Complex lesion morphology, tortuous vessels |
| Renal Complications | 1-2% | Pre-existing kidney disease, diabetes |
Stent-Related Complications
Stent complications can happen soon after or years later. These include:
- Stent thrombosis (clot formation within the stent)
- In-stent restenosis (re-narrowing of the stented segment)
- Stent migration or malposition
To lower these risks, patients often take antiplatelet therapy. Regular check-ups with a healthcare provider are key to watch the stent and heart health.
Knowing these risks helps patients prepare for the procedure and recovery. Working with their healthcare team is essential to reduce risks and get the best results.
Life After Cardiac Stent Placement
Getting a cardiac stent is just the start. It’s important to know how to live with it for good health. After the procedure, patients need to focus on a few key things. This ensures the stent works right and keeps the heart healthy.
Antiplatelet Therapy and Medication Adherence
Antiplatelet therapy is a big part of caring for a stent. Patients usually take two medicines: aspirin and a P2Y12 inhibitor (like clopidogrel). These help stop blood clots from forming on the stent.
Sticking to your medication is key. It’s important to take your medicines as told. Stopping them too soon can lead to serious problems like stent thrombosis.
Lifestyle Modifications for Heart Health
Besides medicine, lifestyle changes are also important for heart health. These include:
- Eating a heart-healthy diet with lots of fruits, veggies, whole grains, and lean proteins.
- Doing regular exercise as your doctor suggests.
- Quitting smoking to lower heart risk.
- Keeping a healthy weight through diet and exercise.
- Managing stress with activities like meditation or yoga.
Follow-up Care and Monitoring
Regular follow-up care is key after getting a stent. This includes:
- Seeing your cardiologist regularly to check the stent and heart health.
- Having tests like echocardiograms or stress tests to check heart function.
- Watching for signs like chest pain or shortness of breath.
By following antiplatelet therapy, making lifestyle changes, and going to follow-up visits, patients can greatly improve their health after getting a cardiac stent.
Conclusion: The Evolution and Impact of Cardiac Stents
Interventional cardiology has seen big steps forward, thanks to cardiac stents. These stents have changed how we treat heart disease. They offer a less invasive option compared to old surgical methods.
Research shows that new stent technology helps patients more. It cuts down on restenosis and improves how long stents stay open. This is true for drug-eluting stents, in particular.
As we keep making stents better, we’ll see even better results for patients. The ongoing work on stent technology is key. It helps us stay ahead in medical care, giving patients the best treatment options.
FAQ
What is the difference between angioplasty and stent placement?
Angioplasty uses a balloon to widen blocked arteries. Stent placement uses a small mesh tube to keep the artery open. They are often done together.
Do I need to keep my leg straight after angioplasty with stenting?
If the procedure was done through the groin, you might need to keep your leg straight. This helps prevent bleeding. But, if it was done through the wrist, you won’t need to.
What are the types of heart stents available?
There are several heart stents, like bare metal, drug-eluting, and biodegradable ones. Each has its own benefits and risks. Your doctor can explain these in detail.
How is a heart stent put in?
A stent is placed during angioplasty. A catheter guides it to the narrowed artery. Then, a balloon is inflated, and the stent is deployed to keep the artery open.
What is the recovery time after angiography and stent placement?
Recovery time varies. It depends on the access site and individual factors. Usually, patients can go home the same day or the next morning. Full recovery takes a few days to a week.
What are the possible risks and complications of angiography and stent placement?
Risks include bleeding and allergic reactions to contrast dye. Stent-related complications are also possible. But, these risks are low. Your doctor will discuss the specific risks with you.
How do I care for myself after cardiac stent placement?
After stent placement, follow your doctor’s advice on medication and lifestyle changes. These support heart health. Also, follow up with your doctor for monitoring and care.
Can I exercise after having a stent placed in my heart?
Yes, exercise is important for heart health after stent placement. But, your doctor will guide you on the right type and intensity of exercise for your condition.
How do I spell heart stent?
The correct spelling is S-T-E-N-T.
What is the difference between a stent and a stint?
A stent is a medical device to keep arteries open. A stint refers to a period of time doing something. In medical terms, it’s always “stent.”
Are cardiac stents safe?
Cardiac stents are generally safe when used correctly. Modern stent technology has greatly improved outcomes. But, as with any medical procedure, there are risks and complications.
Reference
- Omeh, D. J. (2023). Angiography. In StatPearls. StatPearls Publishing. Retrieved October 2025, from https://www.ncbi.nlm.nih.gov/books/NBK557477/