Feeling tired, pale, or short of breath? You’re not alone. Millions worldwide suffer from anemia, a condition that can significantly impact daily life. At Liv Hospital, we understand the importance of accurate diagnosis and personalized treatment.
Clinicians rely on anemia charts to classify the condition into different types based on red blood cell indices. Our experts use advanced SPRT chart analytics to quickly identify the type and cause, ensuring precise treatment.
We use clear and concise tools to help our patients receive the best care possible. By combining these tools with our commitment to excellence, we provide complete support for international patients seeking advanced medical treatments.
Key Takeaways
- Anemia affects millions worldwide, causing fatigue, weakness, and other health issues.
- Accurate diagnosis is key for effective treatment.
- Liv Hospital uses advanced SPRT chart analytics for precise diagnosis.
- Personalized treatment plans are tailored to each patient’s needs.
- Comprehensive support is provided for international patients.
The Global Burden of Anemia
Anemia is a big health problem all over the world. It happens when there aren’t enough red blood cells. These cells carry oxygen to our bodies.
Prevalence and Demographics
The World Health Organization (WHO) says anemia affects a lot of people. Women and children are hit the hardest. Women of childbearing age and kids under five are most affected.
Many things can cause anemia. It can be from not eating enough, chronic diseases, or losing too much blood. Places with bad food and no good healthcare see more anemia.
Health and Economic Impact
Anemia makes people tired, weak, and less sharp. It can also lead to bad pregnancy outcomes and higher death rates. In severe cases, it can make people less productive.
Anemia also costs a lot. It hurts not just the person but also the whole country. It raises healthcare costs and makes people miss work.
To fight anemia, we need to do many things. We must improve food, manage diseases, and better healthcare. Knowing how big anemia is helps us tackle it. This way, we can make the world healthier and wealthier.
Fundamentals of Red Blood Cell Analysis
To diagnose anemia accurately, understanding red blood cell analysis is key. Red blood cell (RBC) analysis is vital for diagnosing and managing anemia. It helps healthcare professionals classify anemia types and choose the right treatment.
Normal RBC Parameters
Normal RBC parameters are important for diagnosing issues. Key parameters include:
- Mean Corpuscular Volume (MCV): Shows the average size of red blood cells, helping to identify anemia types.
- Mean Corpuscular Hemoglobin (MCH): Tells us the average hemoglobin in each red blood cell.
- Mean Corpuscular Hemoglobin Concentration (MCHC): Shows the average hemoglobin concentration in red blood cells.
Knowing these parameters is key for accurate diagnosis. For example, a low MCV means microcytic anemia, while a high MCV means macrocytic anemia.
Key Diagnostic Indices
Several diagnostic indices are also important for anemia diagnosis:
- Red Cell Distribution Width (RDW): Shows the variation in red blood cell size, helping to spot iron deficiency anemia.
- Reticulocyte Count: Checks how well the bone marrow makes new red blood cells, helping find the anemia cause.
By looking at these indices and RBC parameters, doctors get a full picture of a patient’s condition. This detailed approach is vital for accurate diagnosis and effective treatment.
We use these tools to classify anemia into types like microcytic, normocytic, or macrocytic. Each type has its own causes and treatments. The anemia chart is a helpful tool for doctors. It helps them understand anemia diagnosis by organizing lab values and clinical findings.
Using the Anemia Chart in Clinical Practice
Anemia charts are key in doctor’s offices. They help doctors quickly see the size and health of red blood cells. This makes it easier to figure out what kind of anemia a patient has and why.
Morphological Classification
Sorting anemia into types is a big step in diagnosing it. Doctors look at the size and hemoglobin in red blood cells. There are three main types: microcytic, normocytic, and macrocytic anemia.
- Microcytic anemia means small red blood cells, often from not enough iron.
- Normocytic anemia has normal-sized red blood cells, seen in sudden blood loss or long-term illness.
- Macrocytic anemia has big red blood cells, usually from not enough vitamin B12 or folate.
Interpreting Laboratory Values
Understanding lab results is key to making the right diagnosis. Important numbers include Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin (MCH), and Mean Corpuscular Hemoglobin Concentration (MCHC).
A low MCV means microcytic anemia, while a high MCV points to macrocytic anemia. MCH and MCHC tell us about the hemoglobin inside red blood cells.
Differential Diagnosis Approach
When diagnosing anemia, doctors look at many possible causes. For example, microcytic anemia could be from iron lack, thalassemia, or long-term illness.
“A thorough differential diagnosis is vital for finding the real cause of anemia and the right treatment.”
Doctors use lab results and the patient’s symptoms to narrow down the possible causes. This helps them create a treatment plan that works best for the patient.
Using anemia charts in practice makes diagnosing and treating anemia more accurate. It combines looking at red blood cell types, lab results, and possible causes. This way, doctors can better manage anemia and help patients get better.
The Complete Anemia Chart: Morphological Classification
Understanding anemia starts with the morphological classification in the anemia chart. It divides anemia into three types based on Mean Corpuscular Volume (MCV) values. These types are microcytic, normocytic, and macrocytic. By looking at MCV values, doctors can find the cause of anemia and decide on further tests.
Microcytic Anemia (Low MCV)
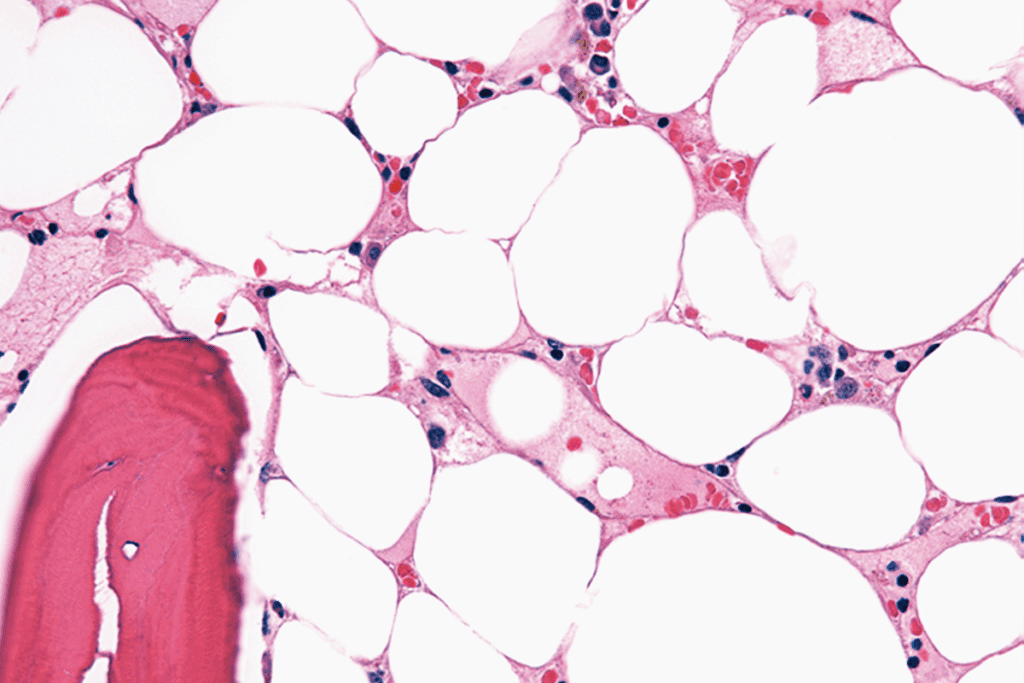
Microcytic anemia has red blood cells that are smaller than usual, with an MCV under 80 fL. Common causes include iron deficiency, thalassemia, and chronic diseases. Iron deficiency anemia is the most common worldwide, caused by poor diet, blood loss, or increased iron needs. Thalassemia, a genetic disorder, also causes microcytic anemia.
“Iron deficiency anemia is a significant public health concern, affecting millions of people worldwide, particularlly in regions with limited access to nutritional resources.”
Normocytic Anemia (Normal MCV)
Normocytic anemia has red blood cells of normal size, with an MCV between 80-100 fL. It’s often seen in chronic illness, acute blood loss, or bone marrow disorders. The causes can vary, needing detailed tests to find the exact reason.
- Chronic kidney disease
- Cancer
- HIV/AIDS
- Rheumatoid arthritis
Normocytic anemia can also be caused by mixed deficiencies or early stages of nutritional deficiencies.
Macrocytic Anemia (High MCV)
Macrocytic anemia has red blood cells larger than usual, with an MCV over 100 fL. Main causes include vitamin B12 or folate deficiency, alcohol abuse, and certain medications. Megaloblastic anemia, with large, immature red blood cells, is a sign of vitamin B12 or folate deficiency.
Correct diagnosis and treatment of macrocytic anemia depend on finding the underlying cause. This could be a nutritional deficiency, a side effect of medication, or something else.
Type 1: Iron Deficiency Anemia
Iron deficiency anemia is a common condition that affects millions. It happens when the body doesn’t have enough iron. This leads to less hemoglobin in red blood cells.
Etiology and Pathophysiology
This condition comes from not getting enough iron, not absorbing it well, or losing blood too much. Over time, the body’s iron stores go down. This means less hemoglobin is made.
Many things can cause this, like not eating enough iron, having stomach problems, or losing a lot of blood during menstruation.
Inadequate iron intake is common in people who eat very little or need more iron, like pregnant women. Poor absorption can happen if you have stomach diseases or have had stomach surgery.
Laboratory Findings
Tests are key to finding iron deficiency anemia. They show low iron and ferritin levels. A complete blood count (CBC) also shows small, pale red blood cells.
A study on the National Center for Biotechnology Information says these tests help tell iron deficiency anemia apart from other anemias.
Clinical Manifestations and Management
People with this anemia might feel tired, weak, and pale. They might also have trouble breathing. Treatment includes iron pills to build up iron levels and fixing the reason for the lack.
It’s also important to get enough iron through food. Eating foods high in iron, like red meat, spinach, and fortified cereals, helps keep iron levels up.
Type 2: Anemia of Chronic Disease
Anemia of chronic disease is a big problem for people with long-term illnesses like kidney disease or cancer. It’s caused by inflammation and problems with iron use. This makes it hard to diagnose and treat.
Inflammatory Mechanisms
Anemia of chronic disease is linked to inflammation in the body. This inflammation stops the production of a key hormone for red blood cells. Cytokines also mess with iron use, even when there’s enough iron.
“The inflammatory response is a double-edged sword; while it’s essential for fighting off infections, it can also lead to complications like anemia of chronic disease,” as noted by recent studies. Understanding these mechanisms is key to finding good treatments.
Distinguishing from Iron Deficiency
It’s hard to tell anemia of chronic disease apart from iron deficiency anemia. Both can cause fatigue and weakness. But they need different treatments. Laboratory tests are very important in making the right diagnosis. For example, serum ferritin levels can tell us if it’s anemia of chronic disease or iron deficiency.
- Serum ferritin levels
- Transferrin saturation
- Erythropoietin levels
By looking at these lab results, doctors can accurately diagnose and plan treatment.
Treatment Considerations
Treating anemia of chronic disease needs a detailed plan. Fixing the underlying condition is key, along with treating the anemia. Doctors might use erythropoiesis-stimulating agents (ESAs) to help make more red blood cells. They might also give iron supplements. But, using ESAs can have risks, like heart problems.
“The goal of treatment is not only to alleviate the symptoms of anemia but also to improve the patient’s quality of life and overall outcomes.”
Understanding the causes, knowing how to tell it apart from iron deficiency, and choosing treatments wisely are all important. This way, doctors can give the best care to those with this complex condition.
Type 3: Hemolytic Anemia
Hemolytic anemia is a group of disorders where red blood cells are destroyed early. It can happen due to genetic or acquired factors. A detailed diagnostic approach is needed.
Classification and Causes
Hemolytic anemia is divided based on its causes. This includes genetic conditions like sickle cell disease and thalassemia. It also includes acquired conditions like autoimmune hemolytic anemia. Knowing the cause is key to managing it well.
Diagnostic Markers
Signs of hemolytic anemia include a high reticulocyte count and lactate dehydrogenase (LDH) levels. These show the bone marrow’s effort to replace lost red blood cells. A thorough lab test is vital for diagnosis.
Therapeutic Approaches
Treatment for hemolytic anemia depends on the cause. For autoimmune cases, corticosteroids might be used. For severe cases, supportive care like blood transfusions is needed. We will explore these treatments further.
Type 4: Megaloblastic Anemia
Megaloblastic anemia is a condition that affects how red blood cells are made. It’s mainly caused by not enough vitamin B12 or folate. These are key for making DNA.
B12 and Folate Metabolism
This anemia happens when DNA making is blocked because of vitamin B12 or folate lack. These vitamins are vital for making red blood cells. Without enough, you get big red blood cells and megaloblasts in the bone marrow.
Vitamin B12 is important for the nervous system and making red blood cells. Not having enough can cause nerve problems and anemia. Folate is also key for avoiding anemia and keeping health up.
Diagnostic Workup
To find megaloblastic anemia, doctors do a detailed check. This includes:
- Complete Blood Counts (CBC) to see how bad the anemia is
- Reticulocyte count to check how the bone marrow is doing
- Vitamin B12 and folate levels to find out what’s missing
This thorough test helps figure out why you have megaloblastic anemia. It also helps decide how to treat it.
Treatment Protocols
Fixing megaloblastic anemia means treating the cause. Giving vitamin B12 or folate is the main treatment. Whether it’s given by mouth or injection depends on how bad the lack is and how you react.
| Treatment Aspect | Vitamin B12 Deficiency | Folate Deficiency |
| Primary Treatment | Vitamin B12 injections | Oral folate supplementation |
| Monitoring | Reticulocyte count, CBC | Reticulocyte count, CBC |
| Duration | Lifelong | Until deficiency is corrected |
Knowing the causes and using the right treatments, doctors can manage megaloblastic anemia well. This helps patients get better.
Type 5: Aplastic Anemia
Aplastic anemia is a serious condition where the bone marrow fails to make enough blood cells. This leads to a lack of red and white blood cells and platelets. It causes many health problems.
Bone Marrow Failure Mechanisms
The causes of aplastic anemia are complex. Autoimmune processes and toxic exposures can destroy the cells needed to make blood. Knowing these causes helps doctors find better treatments.
Aplastic anemia can start for many reasons. It can lead to a big drop in blood cell production. This results in a lack of red and white blood cells and platelets.
Severity Classification
It’s important to know how severe aplastic anemia is. Doctors use blood counts and bone marrow biopsies to figure this out. Severe aplastic anemia has very low blood counts and a bone marrow that looks empty.
- Bone marrow cellularity less than 25%
- Two or more of the following:
- Absolute neutrophil count (ANC) less than 500 cells/μL
- Platelet count less than 20,000/μL
- Reticulocyte count less than 1%
Management Strategies
Treating aplastic anemia involves several steps. These include immunosuppressive therapy and hematopoietic stem cell transplantation. The treatment plan depends on how severe the condition is, the patient’s age, and any other health issues.
Quick diagnosis and treatment are key to better outcomes. Understanding aplastic anemia helps doctors find the best ways to manage it.
The SPRT Chart Breakdown for Anemia Diagnosis
The SPRT chart is key in diagnosing anemia. It gives a detailed look at how well tests work. This helps doctors make better choices for their patients.
Sensitivity: Detecting True Positives
Sensitivity is very important in finding anemia. It shows how well a test can spot people with the condition. A good test will catch most cases, avoiding false negatives.
High sensitivity is vital for quick treatment. We’ll dive deeper into why it matters.
Precision: Accuracy of Positive Results
Precision is also critical. It shows how many true positives there are among all positive results. For anemia, high precision means fewer wrong treatments and less worry for patients.
Doctors aim to find the right balance between sensitivity and precision. Let’s see how they do it.
Recall: Complete Detection Rate
Recall is like sensitivity. It shows how well a test finds all anemia cases. A high recall rate means the test catches most instances.
Knowing recall is key for doctors to catch all anemia cases. We’ll look at its importance more closely.
Trade-off: Balancing Diagnostic Parameters
When using tests for anemia, there’s a trade-off. Sensitivity, precision, and recall must be balanced. Doctors need to find the best mix for their tests.
For example, making a test more sensitive might make it less precise. Understanding these trade-offs helps doctors choose the right tests.
| Diagnostic Metric | Description | Importance in Anemia Diagnosis |
| Sensitivity | Measures true positive rate | High sensitivity ensures most cases are detected |
| Precision | Measures accuracy of positive results | High precision avoids unnecessary treatment |
| Recall | Measures complete detection rate | High recall ensures most cases are identified |
Conclusion: Optimizing Anemia Diagnosis and Treatment
To improve anemia diagnosis and treatment, we need to understand anemia types and how to diagnose them. We’ve looked at different anemia types, like iron deficiency and anemia of chronic disease. Each has its own signs and lab results.
Using anemia charts and the SPRT chart helps doctors diagnose faster and more accurately. This leads to better treatment plans, improving patients’ lives. It’s key to keep up with new research in anemia care to offer top-notch treatment.
By using anemia charts and the SPRT chart, doctors can make better choices. This helps in diagnosing and treating anemia more effectively. As we learn more about anemia, we can give our patients the best care possible.
FAQ
What is anemia and how is it diagnosed?
Anemia is when you don’t have enough red blood cells or hemoglobin. This can cause fatigue, weakness, and shortness of breath. Doctors use lab tests and charts to find out if you have anemia.
What is the SPRT chart and how is it used in anemia diagnosis?
The SPRT chart is a tool for doctors to help with anemia diagnosis. It helps them understand how accurate tests are. This way, doctors can make better decisions for their patients.
What are the different types of anemia and their causes?
There are many types of anemia, like iron deficiency and anemia of chronic disease. Each type has its own causes and signs. For example, low MCV means microcytic anemia, and high MCV means macrocytic anemia.
How is iron deficiency anemia diagnosed and managed?
Doctors check lab results to diagnose iron deficiency anemia. They then treat it with iron supplements. They also look for the cause, like not eating enough iron or losing blood too much.
What is the difference between anemia of chronic disease and iron deficiency anemia?
Anemia of chronic disease happens in people with long-term illnesses. It’s different from iron deficiency anemia. Doctors need to know this to treat it right. They look at inflammation and treatment options.
How is the SPRT chart used to optimize anemia diagnosis?
The SPRT chart helps doctors make the best decisions for anemia tests. It shows how accurate tests are. This way, doctors can give the best care to patients with anemia.
What is megaloblastic anemia and how is it treated?
Megaloblastic anemia is caused by not enough vitamin B12 or folate. Doctors treat it with supplements. They diagnose it by checking blood counts and vitamin levels.
What is aplastic anemia and how is it managed?
Aplastic anemia is when the bone marrow doesn’t make blood cells. Doctors diagnose it by looking at bone marrow and blood counts. They need to understand the bone marrow failure to manage it well.
References
- World Health Organization. (2021). Anaemia. https://www.who.int/health-topics/anaemia










